- mu Opioid receptor
-
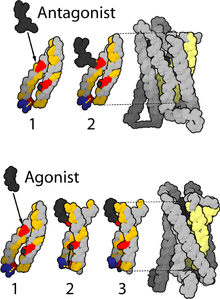 Active and inactive μ-opioid receptors.[1]
Active and inactive μ-opioid receptors.[1]
The μ-opioid receptors (MOR) are a class of opioid receptors with high affinity for enkephalins and beta-endorphin but low affinity for dynorphins. They are also referred to as μ opioid peptide (MOP) receptors. The prototypical μ receptor agonist is the opium alkaloid morphine; μ (mu) refers to morphine.
Contents
Types
There are three well-characterized variants of the μ opioid receptor, though reverse-transcriptase PCR has identified up to 10 total splice variants in humans.[2][3]
More is known about the μ1 opioid receptor than is known about the other types, but some information does exist. TRIMU 5 is a selective agonist of the μ2 receptor.[4]
In 2003, a μ3 variant was described,[5] which was responsive to opiate alkaloids but not opioid peptides.[6]
Location
They can exist either presynaptically or postsynaptically depending upon cell types.
The μ-receptors exist mostly presynaptically in the periaqueductal gray region, and in the superficial dorsal horn of the spinal cord (specifically the substantia gelatinosa of Rolando). Other areas where μ-receptors have been located include the external plexiform layer of the olfactory bulb, the nucleus accumbens, in several layers of the cerebral cortex and in some of the nuclei of the amygdala, as well as the nucleus of the solitary tract.
μ receptors are also found in the intestinal tract. This causes constipation, a major side effect of μ agonists, due to inhibition of peristaltic action.
Activation
MOR can mediate acute changes in neuronal excitability via "disinhibition" of presynaptic release of GABA (see works from Charles Chavkin and Roger Nicoll). Activation of the MOR leads to different effects on dendritic spines depending upon the agonist, and may be an example of functional selectivity at the μ receptor.[7] The physiological and pathological roles of these two distinct mechanisms remain to be clarified. Perhaps, both might be involved in opioid addiction and opioid-induced deficits in cognition.
Activation of the μ receptor by an agonist such as morphine causes analgesia, sedation, slightly reduced blood pressure, itching, nausea, euphoria, decreased respiration, miosis (constricted pupils) and decreased bowel motility often leading to constipation. Some of these side effects, such as sedation, euphoria and decreased respiration, tend to lessen with continued use as tolerance develops. Analgesia, miosis and reduced bowel motility tend to persist; little tolerance develops to these effects.
The canonical MOR1 isoform is responsible for morphine-induced analgesia whereas the alternatively spliced MOR1D isoform (through heterodimerization with the gastrin-releasing peptide receptor) is required for morphine-induced itching.[8]
Deactivation
As with other G protein-coupled receptors, signalling by the mu opioid receptor is terminated through several different mechanisms, which are upregulated with chronic use, leading to rapid tachyphylaxis.[9] The most important regulatory proteins for the mu opioid receptor are the β-arrestins Arrestin beta 1 and Arrestin beta 2,[10][11][12] and the RGS proteins RGS4, RGS9-2, RGS14 and RGSZ2.[13][14]
Long-term or high dose use of opioids may also lead to additional mechanisms of tolerance becoming involved. This includes downregulation of mu opioid receptor gene expression, so the number of receptors presented on the cell surface is actually reduced, as opposed to the more short-term desensitisation induced by β-arrestins or RGS proteins.[15][16][17] Another long-term adaptation to opioid use can be upregulation of glutamate and other pathways in the brain which can exert an opioid-opposing effect and so reduce the effects of opioid drugs by altering downstream pathways, regardless of mu opioid receptor activation.[18][19]
Tolerance and overdoses
Opioid overdoses kill through apnea and fatal hypoxia, often aggravated by simultaneous use of alcohol, benzodiazepines or barbiturates. Substantial tolerance to respiratory depression develops quickly, and tolerant individuals can withstand larger doses (an example of Mithridatism). However tolerance to respiratory depression is lost just as quickly during withdrawal. Many[citation needed] overdoses occur in people who misuse their medication after being in withdrawal long enough to lose the tolerance to respiratory depression. Less commonly, massive overdoses have been known to cause circulatory collapse.
Opioid overdoses can be rapidly reversed with any of several opioid antagonists: naloxone, or naltrexone, differing primarily in their duration of action and potency. While commonly referred to as antagonists, and when used to treat an overdose they do appear to function as such, naloxone & naltrexone are inverse agonists.[citation needed]
See also
References
- ^ Zhorov BS, Ananthanarayanan VS. Homology models of μ-opioid receptor with organic and inorganic cations at conserved aspartates in the second and third transmembrane domains. Arch Biochem Biophys. 37:31-49, 2000.
- ^ Dortch-Carnes J, Russell K (2007). "Morphine-stimulated nitric oxide release in rabbit aqueous humor". Exp. Eye Res. 84 (1): 185–90. doi:10.1016/j.exer.2006.09.014. PMC 1766947. PMID 17094965. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1766947.
- ^ Pan L, Xu J, Yu R, Xu MM, Pan YX, Pasternak GW (2005). "Identification and characterization of six new alternatively spliced variants of the human mu opioid receptor gene, Oprm". Neuroscience. 133 (1): 209–20. doi:10.1016/j.neuroscience.2004.12.033. PMID 15893644.
- ^ Eisenberg RM (1994). "TRIMU-5, a μ2-opioid receptor agonist, stimulates the hypothalamo-pituitary-adrenal axis". Pharmacol. Biochem. Behav. 47 (4): 943–6. doi:10.1016/0091-3057(94)90300-X. PMID 8029266.
- ^ Cadet P, Mantione KJ, Stefano GB (2003). "Molecular identification and functional expression of μ3, a novel alternatively spliced variant of the human μ opiate receptor gene". J. Immunol. 170 (10): 5118–23. PMID 12734358.
- ^ Stefano GB (2004). "Endogenous morphine: a role in wellness medicine". Med. Sci. Monit. 10 (6): ED5. PMID 15173675.
- ^ Liao D, Lin H, Law PY, Loh HH (February 2005). "Mu-opioid receptors modulate the stability of dendritic spines". Proc. Natl. Acad. Sci. U.S.A. 102 (5): 1725–30. doi:10.1073/pnas.0406797102. PMC 545084. PMID 15659552. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=545084.
- ^ Liu X-Y, Liu Z-C, Sun Y-G, Ross M, K S, Tsai F-F, Li Q-F, Jeffry J, Kim J-Y, Loh HH, Chen Z-F. "Unidirectional Cross-Activation of GRPR by MOR1D Uncouples Itch and Analgesia Induced by Opioids". Cell 147 (2): 447–458. doi:10.1016/j.cell.2011.08.043. Lay summary – Washington University in St. Louis Press Release.
- ^ Martini L, Whistler JL (October 2007). "The role of mu opioid receptor desensitization and endocytosis in morphine tolerance and dependence". Current Opinion in Neurobiology 17 (5): 556–64. doi:10.1016/j.conb.2007.10.004. PMID 18068348.
- ^ Zuo Z (September 2005). "The role of opioid receptor internalization and beta-arrestins in the development of opioid tolerance". Anesthesia and Analgesia 101 (3): 728–34, table of contents. doi:10.1213/01.ANE.0000160588.32007.AD. PMID 16115983.
- ^ Marie N, Aguila B, Allouche S (November 2006). "Tracking the opioid receptors on the way of desensitization". Cellular Signalling 18 (11): 1815–33. doi:10.1016/j.cellsig.2006.03.015. PMID 16750901.
- ^ DuPen A, Shen D, Ersek M (September 2007). "Mechanisms of opioid-induced tolerance and hyperalgesia". Pain Management Nursing : Official Journal of the American Society of Pain Management Nurses 8 (3): 113–21. doi:10.1016/j.pmn.2007.02.004. PMID 17723928.
- ^ Garzón J, Rodríguez-Muñoz M, Sánchez-Blázquez P (May 2005). "Morphine alters the selective association between mu-opioid receptors and specific RGS proteins in mouse periaqueductal gray matter". Neuropharmacology 48 (6): 853–68. doi:10.1016/j.neuropharm.2005.01.004. PMID 15829256.
- ^ Hooks SB, Martemyanov K, Zachariou V (January 2008). "A role of RGS proteins in drug addiction". Biochemical Pharmacology 75 (1): 76–84. doi:10.1016/j.bcp.2007.07.045. PMID 17880927.
- ^ Sirohi S, Dighe SV, Walker EA, Yoburn BC (November 2008). "The analgesic efficacy of fentanyl: relationship to tolerance and mu-opioid receptor regulation". Pharmacology, Biochemistry, and Behavior 91 (1): 115–20. doi:10.1016/j.pbb.2008.06.019. PMC 2597555. PMID 18640146. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2597555.
- ^ Lopez-Gimenez JF, Vilaró MT, Milligan G (November 2008). "Morphine desensitization, internalization, and down-regulation of the mu opioid receptor is facilitated by serotonin 5-hydroxytryptamine2A receptor coactivation". Molecular Pharmacology 74 (5): 1278–91. doi:10.1124/mol.108.048272. PMID 18703670.
- ^ Kraus J (2009). "Regulation of mu-opioid receptors by cytokines". Frontiers in Bioscience (Scholar Edition) 1: 164–70. PMID 19482692.
- ^ García-Fuster MJ, Ramos-Miguel A, Rivero G, La Harpe R, Meana JJ, García-Sevilla JA (November 2008). "Regulation of the extrinsic and intrinsic apoptotic pathways in the prefrontal cortex of short- and long-term human opiate abusers". Neuroscience 157 (1): 105–19. doi:10.1016/j.neuroscience.2008.09.002. PMID 18834930.
- ^ Ueda H, Ueda M (2009). "Mechanisms underlying morphine analgesic tolerance and dependence". Frontiers in Bioscience : a Journal and Virtual Library 14: 5260–72. PMID 19482614.
External links
- "Opioid Receptors: μ". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology. http://www.iuphar-db.org/GPCR/ReceptorDisplayForward?receptorID=2405.
- MeSH mu+Opioid+Receptor
Cell surface receptor: G protein-coupled receptors Class A:
Rhodopsin likeOtherMetabolites and
signaling moleculesOtherBile acid · Cannabinoid (CB1, CB2, GPR (18, 55, 119)) · EBI2 · Estrogen · Free fatty acid (1, 2, 3, 4) · Lactate · Lysophosphatidic acid (1, 2, 3, 4, 5, 6) · Lysophospholipid (1, 2, 3, 4, 5, 6, 7, 8) · Niacin (1, 2) · Oxoglutarate · PAF · Sphingosine-1-phosphate (1, 2, 3, 4, 5) · SuccinatePeptideOtherAnaphylatoxin (C3a, C5a) · Angiotensin (1, 2) · Apelin · Bombesin (BRS3, GRPR, NMBR) · Bradykinin (B1, B2) · Chemokine · Cholecystokinin (A, B) · Endothelin (A, B) · Formyl peptide (1, 2, 3) · FSH · Galanin (1, 2, 3) · GHB receptor · Gonadotropin-releasing hormone (1, 2) · Ghrelin · Kisspeptin · Luteinizing hormone/choriogonadotropin · MAS (1, 1L, D, E, F, G, X1, X2, X3, X4) · Melanocortin (1, 2, 3, 4, 5) · MCHR (1, 2) · Motilin · Opioid (Delta, Kappa, Mu, Nociceptin & Zeta, but not Sigma) · Orexin (1, 2) · Oxytocin · Prokineticin (1, 2) · Prolactin-releasing peptide · Relaxin (1, 2, 3, 4) · Somatostatin (1, 2, 3, 4, 5) · Tachykinin (1, 2, 3) · Thyrotropin · Thyrotropin-releasing hormone · Urotensin-II · Vasopressin (1A, 1B, 2)MiscellaneousGPR (1, 3, 4, 6, 12, 15, 17, 18, 19, 20, 21, 22, 23, 25, 26, 27, 31, 32, 33, 34, 35, 37, 39, 42, 44, 45, 50, 52, 55, 61, 62, 63, 65, 68, 75, 77, 78, 81, 82, 83, 84, 85, 87, 88, 92, 101, 103, 109A, 109B, 119, 120, 132, 135, 137B, 139, 141, 142, 146, 148, 149, 150, 151, 152, 153, 160, 161, 162, 171, 173, 174, 176, 177, 182, 183)OtherClass B: Secretin like OtherBrain-specific angiogenesis inhibitor (1, 2, 3) · Cadherin (1, 2, 3) · Calcitonin · CALCRL · CD97 · Corticotropin-releasing hormone (1, 2) · EMR (1, 2, 3) · Glucagon (GR, GIPR, GLP1R, GLP2R) · Growth hormone releasing hormone · PACAPR1 · GPR · Latrophilin (1, 2, 3, ELTD1) · Methuselah-like proteins · Parathyroid hormone (1, 2) · Secretin · Vasoactive intestinal peptide (1, 2)Class C: Metabotropic
glutamate / pheromoneOtherClass F:
Frizzled / SmoothenedFrizzledSmoothenedB trdu: iter (nrpl/grfl/cytl/horl), csrc (lgic, enzr, gprc, igsr, intg, nrpr/grfr/cytr), itra (adap, gbpr, mapk), calc, lipd; path (hedp, wntp, tgfp+mapp, notp, jakp, fsap, hipp, tlrp) Neuropeptide receptors G protein-coupled receptor OtherOther neuropeptide receptorsAngiotensin · Bradykinin (B1, B2) / Tachykinin (TACR1) · Calcitonin gene-related peptide · Galanin · GPCR neuropeptide (B/W, FF, S, Y) · NeurotensinType I cytokine receptor Enzyme-linked receptor Other B trdu: iter (nrpl/grfl/cytl/horl), csrc (lgic, enzr, gprc, igsr, intg, nrpr/grfr/cytr), itra (adap, gbpr, mapk), calc, lipd; path (hedp, wntp, tgfp+mapp, notp, jakp, fsap, hipp, tlrp) Anxiety disorder: Obsessive–compulsive disorder (F42, 300.3) History Yale–Brown Obsessive Compulsive ScaleBiology NeuroanatomyReceptorsSymptoms Obsessions (associative, diagnostic, injurious, scrupulous, pathogenic, sexual) · Compulsions (impulses, rituals, tics) · Thought suppression (avoidance) · Hoarding (animals, books, possessions)Treatment Mu opioidergicsNMDA glutamatergicsNK-1 tachykininergicsOtherBehavioralOrganizations Notable people Edna B. Foa · Stanley Rachman · Adam S. Radomsky · Jeffrey M. Schwartz · Susan Swedo · Jeff Bell · Emily ColasPopular culture LiteratureFictionalNonfictionEverything in Its Place · Just CheckingMediaRelated Obsessive–compulsive personality disorder · Obsessional jealousy · Purely Obsessional OCD · Social anxiety disorder · Tourette syndromeCategories:- Human proteins
- Opioid receptor
Wikimedia Foundation. 2010.