- Naltrexone
-
Not to be confused with the related chemical naloxone.
Naltrexone 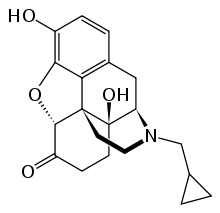
Systematic (IUPAC) name 17-(cyclopropylmethyl)-4,5α-epoxy- 3,14-dihydroxymorphinan-6-one Clinical data Trade names Revia AHFS/Drugs.com monograph MedlinePlus a685041 Pregnancy cat. Category B3 (Australia) Legal status Schedule 4 (Australia) Routes oral
hepaticPharmacokinetic data Bioavailability 5–40% Protein binding 21% Metabolism hepatic Half-life 4 h (naltrexone),
13 h (6-β-naltrexol)Excretion renal Identifiers CAS number 16590-41-3 
ATC code N07BB04 PubChem CID 5360515 IUPHAR ligand 1639 DrugBank APRD00005 ChemSpider 4514524 
UNII 5S6W795CQM 
KEGG D05113 
ChEBI CHEBI:7465 
ChEMBL CHEMBL142 
Chemical data Formula C20H23NO4 Mol. mass 341.401 g/mol SMILES eMolecules & PubChem Physical data Melt. point 169 °C (336 °F)  (what is this?) (verify)
(what is this?) (verify)Naltrexone is an opioid receptor antagonist used primarily in the management of alcohol dependence and opioid dependence. It is marketed in generic form as its hydrochloride salt, naltrexone hydrochloride, and marketed under the trade names Revia and Depade. In some countries including the United States, a once-monthly extended-release injectable formulation is marketed under the trade name Vivitrol. Also in the US, Methylnaltrexone Bromide, a closely related drug, is marketed as Relistor, for the treatment of opioid induced constipation.
Naltrexone should not be confused with naloxone (which is used in emergency cases of overdose rather than for longer-term dependence control) nor nalorphine. Both nalorphine and naloxone are full antagonists and will treat an opioid overdose, but naltrexone is longer-acting than naloxone (although neither is an irreversible antagonist like naloxazone), making naloxone a better emergency antidote.
Contents
Chemical structure
Naltrexone can be described as a substituted oxymorphone – here the tertiary amine methyl-substituent is replaced with methylcyclopropane.
Naltrexone is the N-cyclopropylmethyl derivative of oxymorphone.
Pharmacology
Naltrexone and its active metabolite 6-β-naltrexol are competitive antagonists at μ- and κ-opioid receptors, and to a lesser extent at δ-opioid receptors.[1] The plasma halflife of naltrexone is about 4 h, for 6-β-naltrexol 13 h. The blockade of opioid receptors is the basis behind its action in the management of opioid dependence—it reversibly blocks or attenuates the effects of opioids.
Its use in alcohol (ethanol) dependence has been studied and has been shown to be effective [1]. Its mechanism of action in this indication is not fully understood, but as an opioid-receptor antagonist it's likely to be due[citation needed] to the modulation of the dopaminergic mesolimbic pathway which is hypothesised to be a major center of the reward associated with addiction (being one of the primary centers for risk-reward analysis in the brain, and a tertiary "pleasure center") that all major drugs of abuse are believed to activate.
Naltrexone is metabolised mainly to 6β-naltrexol by the liver enzyme dihydrodiol dehydrogenase. Other metabolites include 2-hydroxy-3-methoxy-6β-naltrexol and 2-hydroxy-3-methoxy-naltrexone. These are then further metabolised by conjugation with glucuronide.
Rapid detoxification
Naltrexone is sometimes used for rapid detoxification ("rapid detox") regimens for opioid dependence. The principle of rapid detoxification is to induce opioid-receptor blockage while the patient is in a state of impaired consciousness, so as to attenuate the withdrawal symptoms experienced by the patient. Rapid detoxification under general anaesthesia involves an unconscious patient and requires intubation and external ventilation. Rapid detoxification is also possible under sedation. The rapid detoxification procedure is followed by oral naltrexone daily for up to 12 months for opioid dependence management. There are a number of practitioners who will use a naltrexone implant, usually placed in the lower abdomen, to replace the oral naltrexone. This implant procedure has not been shown scientifically to be successful in "curing" subjects of their addiction, though it does provide a better solution than oral naltrexone for medication compliance reasons. There is currently scientific disagreement as to whether this procedure should be performed under local or general anesthesia, due to the rapid, and sometimes severe, withdrawal that occurs from the naltrexone displacing the opiates from the receptor sites.
Rapid detoxification has been criticised by some for its questionable efficacy in long-term opioid dependence management.[2] Rapid detoxification has often been misrepresented as a one-off "cure" for opioid dependence, when it is only intended as the initial step in an overall drug rehabilitation regimen. Rapid detoxification is effective for short-term opioid detoxification, but is approximately 10 times more expensive than conventional detoxification procedures. Aftercare can also be an issue,[2] since at least one well-known center in the United States reported that they will remove an implant from any patient arriving in their facility before admission.[citation needed][who?]
The usefulness of naltrexone in opioid dependence is very limited by the low retention in treatment. Like disulfiram in alcohol dependence, it temporarily blocks substance intake and does not affect craving. Sustained-release preparations of naltrexone have shown rather promising results, it remains a treatment only for a small part of the opioid-dependent population, usually the ones with an unusually stable social situation and motivation (e.g., dependent health care professionals). It is given orally by physicians to help reduce the side effects of opiate dependence. Naltrexone implants have been used successfully in Australia for a number of years as part of a long-term protocol for treating opiate addiction. Naltrexone treats the physical dependence on opioids, but further psychosocial interventions are often required to enable people to maintain abstinence.[3]
Alcohol dependence
The main use of naltrexone is for the treatment of alcohol dependence. After publication of the first two randomized, controlled trials in 1992, a number of studies have confirmed its efficacy in reducing frequency and severity of relapse to drinking.[4] The multi-center COMBINE study has recently proven the usefulness of naltrexone in an ordinary, primary care setting, without adjunct psychotherapy.[5]. Mechanism of action may be antagonism to endogenous opiates such as tetrahydropapaveroline, whose production is augmented in the presence of alcohol.[6]
The standard regimen is one 50 mg tablet per day. Initial problems of nausea usually disappear after a few days, and other side effects (e.g., heightened liver enzymes) are rare. Drug interactions are not significant, besides the obvious antagonism of opioid analgesics. Naltrexone has two effects on alcohol consumption.[7] The first is to reduce craving while naltrexone is being taken. The second, referred to as the Sinclair Method, occurs when naltrexone is taken in conjunction with normal drinking, and this reduces craving over time. The first effect persists only while the naltrexone is being taken, but the second persists as long as the alcoholic does not drink without first taking naltrexone.
Roy Eskapa, who wrote a book advocating the Sinclair Method, argues that Naltrexone does not work in conjunction with abstinence.[8] Eskapa cites as evidence a Finnish clinical trial in which "Naltrexone tended to be worse than those for placebo,"[9] and two studies that produced "almost identical graphs": an alcoholism clinical trial at Yale[10] and a Naltrexone for cocaine addiction trial at the University of Texas.[11]
Depot injectable naltrexone (Vivitrol, formerly Vivitrex, but changed after a request by the FDA) was approved by the FDA on April 13, 2006 for the treatment of alcohol dependence.[12] This version is made and marketed by Alkermes in the United States, and is marketed by Johnson & Johnson in Russia. Cephalon Inc. originally marketed the drug in the United States, however, Alkermes reclaimed Vivitrol commercialization rights in 2008.[13] The recommended dose of Vivitrol 380 mg is delivered intramuscularly once a month. The injection should be administered by a healthcare professional.[14]
The clinical trial that the approval of Vivitrol was based on showed that when compared with a placebo, 380 mg of Vivitrol resulted in a 25% decrease in the event rate of heavy drinking days and 190 mg resulted in a 17% decrease. The 6-month randomized, double-blind, placebo-controlled study was conducted between February 2002 and September 2003. Of the 899 individuals screened, 627 were diagnosed as alcohol-dependent adults and were randomized to receive treatment. The main outcome measure was the event rate of heavy drinking days in the intent-to-treat population. The study’s authors concluded that: “Long-acting naltrexone was well tolerated and resulted in reductions in heavy drinking among treatment-seeking alcohol dependent patients during 6 months of therapy.”[15]
Another study released by the National Institute of Health in February 2008 and published in the Archives of General Psychiatry has shown that alcoholics having a certain gene variant of the opioid receptor were far more likely to experience success at cutting back or discontinuing their alcohol intake altogether.[16]
Opiate addiction
Naltrexone helps patients overcome urges to abuse opiates by blocking the drugs’ euphoric effects. While some patients do well with the oral formulation, there is a drawback in that it must be taken daily, and a patient whose craving becomes overwhelming can obtain opiate euphoria simply by skipping a dose before resuming abuse.
The FDA approved Vivitrol, the long-acting version of naltrexone, on October 12, 2010 for the prevention of relapse to opioid dependence, following opioid detoxification. “This drug approval represents a significant advancement in addiction treatment,” said Janet Woodcock, M.D., director of the FDA’s Center Drug Evaluation and Research.[17]
Nora Volkow, M.D., Director of the National Institute on Drug Abuse (NIDA), stated that: “As a depot formulation, dosed monthly, Vivitrol obviates the daily need for patients to motivate themselves to stick to a treatment regimen - a formidable task, especially in the face of multiple triggers of craving and relapse. This new option increases the pharmaceutical choices for treating opioid addiction, and may be seen as advantageous by those unwilling to consider agonist or partial agonist approaches to treatment. NIDA is continuing to support research on Vivitrol's effectiveness in this country, including a focus on criminal justice involved populations transitioning back into the community.”[18]
The phase 3 clinical study upon which the FDA granted approval for Vivitrol in treating opioid dependence had an enrollment of 250. Primary outcome measures were percent of weekly urine tests that were negative for opioids and the length of the study retention during the double-blind period. The study began in June 2008 and was completed in November 2009.
Alkermes presented positive results from the phase 3 clinical study of Vivitrol for the treatment of opioid dependence at the American Psychiatric Association 2010 Annual Meeting in May 2010. The study met its primary efficacy endpoint and data showed that patients treated once-monthly with Vivitrol demonstrated statistically significant higher rates of clean (opioid-free) urine screens, compared to patients treated with a placebo, as measured by the cumulative distribution of clean urine screens (p<0.0002).[19] The results of the study are expected to be published soon.
Another option for the treatment of opiate addiction is the naltrexone implant, which may be surgically inserted under the skin. The implant provides a sustained dose of naltrexone to the patient, thereby preventing the problems which may be associated with skipping doses. It must be replaced every several months. Naltrexone implants are made by at least three companies, though none have been approved by the U.S. Food and Drug Administration (FDA) or the Australian Therapeutic Goods Administration.[20]
Depersonalization disorder
Naltrexone is sometimes used in the treatment of depersonalization disorder. While studies have suggested it is less effective than naloxone for treating depersonalization, naloxone is impractical for daily use because it must be injected intravenously. A 2005 naltrexone study demonstrated an average of 30% reduction of depersonalization symptoms, as measured by 3 validated dissociation scales [21]. Most of the efforts in studying naltrexone for depersonalization thus far have been directed by Dr. Daphne Simeon at the Mount Sinai School of Medicine.
Safety
In alcohol dependence, naltrexone is considered a safe medication. Control of liver values prior to initiation of treatment is recommended. There has been some controversy regarding the use of opioid-receptor antagonists, such as naltrexone, in the long-term management of opioid dependence due to the effect of these agents in sensitising the opioid receptors. That is, after therapy, the opioid receptors continue to have increased sensitivity for a period during which the patient is at increased risk of opioid overdose. This effect reinforces the necessity of monitoring of therapy and provision of patient support measures by medical practitioners. All individuals taking naltrexone are encouraged to keep a card or a note in their wallet in case of an injury or another medical emergency. This is to let medical personnel know that special procedures are required if opiate-based painkillers are to be used.
Other uses
Low dose naltrexone
Main article: Low dose naltrexone"Low dose naltrexone" (LDN) describes the "off-label" use of naltrexone at low doses for diseases not related to chemical dependency or intoxication, such as multiple sclerosis.[22] Preliminary research suggests low dose naltrexone may be useful in preventing opioid tolerance and dependence when combined with an opioid,[23] reduce the severity of opioid withdrawal,[24] or improve fibromyalgia symptoms,[25] though much more research needs to be done before it can be recommended for clinical use.
Although there have been dramatic claims about its efficacy in treating a wide range of diseases including cancer and HIV, these claims are not generally supported by scientific evidence.[22] This treatment has gotten significant attention on the Internet, especially through websites run by organizations promoting its use.[26]
Tobacco study
The Chicago Stop Smoking Research Project at the University of Chicago found that naltrexone did not help improve study subjects quit smoking better than placebo.[27]
Self-injurious behaviors
Some studies suggest that self-injurious behaviors present in persons with developmental disabilities (including autism) can sometimes be remedied with naltrexone.[28] In these cases, it is believed that the self-injury is being done to release beta-endorphin, which binds to the same receptors as heroin and morphine.[29] By removing the "rush" generated by self-injury, the behavior may stop.
Behavioral addiction
There are indications that naltrexone might be beneficial in the treatment of impulse control disorders such as kleptomania (compulsive stealing), trichotillomania, or pathological gambling.[30] A 2008 case study reported successful use of naltrexone in suppressing and treating an internet pornography addiction.[31]
External links
- LDNscience.org, a website dedicated to promoting and studying the therapeutic indications of low dose naltrexone.
References
- ^ Shader, RI. "Antagonists, Inverse Agonists, and Protagonists." Journal of Clinical Psychopharmacology. 2003 Aug; 23(4):321–322. PMID 12920405
- ^ a b Wodak, Dr. Alex (Summer 07/08). "I woke up cured of Naltrexone!" (Online Version of published magazine article). User's News (New South Wales User's and AIDS Association). http://www.nuaa.org.au/index.php?option=com_content&view=article&id=105:i-woke-up-cured-of-naltrexone&catid=7:issue-no-53&Itemid=57. Retrieved 2009-03-22. ""Maybe there was an increased risk of death when people took naltrexone for a while and then started taking heroin? Maybe the success rate of naltrexone, whether started with UROR or ROD, was not as great as some had claimed?""
- ^ Hanson, Merideth (2001). "Three". In Alex Gitterman. The Handbook of Social Work practice with vulnerable and resilient populations, 2nd Edition (Second ed.). New York: Columbia University Press.
- ^ Latt NC, Jurd S, Houseman J, Wutzke SE (June 2002). "Naltrexone in alcohol dependence: a randomised controlled trial of effectiveness in a standard clinical setting". Med J Aust 176 (11): 530–4. PMID 12064984. http://www.mja.com.au/public/issues/176_11_030602/lat10411_fm.html.
- ^ "Naltrexone or Specialized Alcohol Counseling an Effective Treatment for Alcohol Dependence When Delivered with Medical Management" (Press release). National Institutes of Health. May 2, 2006. http://www.nih.gov/news/pr/may2006/niaaa-02.htm. Retrieved 2009-04-16.
- ^ Haber, H; Roske, I; Rottmann, M; Georgi, M; Melzig, MF (1997). "Alcohol induces formation of morphine precursors in the striatum of rats". Life sciences 60 (2): 79–89. doi:10.1016/S0024-3205(96)00597-8. PMID 9000113.
- ^ Sinclair JD (2001). "Evidence about the use of naltrexone and for different ways of using it in the treatment of alcoholism". Alcohol and Alcoholism 36 (1): 2–10. doi:10.1093/alcalc/36.1.2. PMID 11139409. http://alcalc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=11139409.
- ^ Eskapa, Roy (2008). The Cure for Alcoholism. BenBella Books. pp. 35. ISBN 1933771550. http://www.TheCureForAlcoholism.com.
- ^ P. Heinälä et al., "Targeted Use of Naltrexone without Prior Detoxification in the Treatment of Alcohol Dependence: A Factorial Double-Blind Placebo-Controlled Trial," Journal of Clinical Psychopharmacology 21 (2001): 287-292.
- ^ S.S. O'Malley, A. Jaffe, G. Chang, G. Witte, R. S. Schottenfeld, and B. J. Rounsaville, "Naltrexone in the Treatment of Alcohol Dependence," in Opioids, Bulimia, and Alcohol Abuse and Alcoholism, ed. L. D. Reid (New York: Springer, 1990), 149-157. S.S. O'Malley, A. J. Jaffe, G. Chang, R. S. Schottenfeld, and B. J. Rounsaville, "Naltrexone and Coping Skills Therapy for Alcohol Dependence," Archives of General Psychiatry 49 (1992): 881-887.
- ^ J. M. Schmitz, A. L. Stotts, H. M. Rhoades, and J. Grabowski, "Naltrexone and Relapse Prevention Treatment for Cocaine-Dependent Patients," Addictive Behavior 26 (2001): 167-180.
- ^ “Alcoholism Once A Month Injectable Drug, Vivitrol, Approved By FDA,” Medical News Today, April 16, 2006.
- ^ “Alkermes reclaims Vivitrol commercialization rights from Cephalon,” Mass High Tech, December 1, 2008.
- ^ Vivitrol Prescribing Information
- ^ James C. Garbutt, MD; Henry R. Kranzler, MD; Stephanie S. O’Malley, PhD; David R. Gastfriend, MD; Helen M. Pettinati, PhD; Bernard L. Silverman, MD; John W. Loewy, PhD; Elliot W. Ehrich, MD; “Efficacy and Tolerability of Long-Acting Injectable Naltrexone for Alcohol DependenceA Randomized Controlled Trial,” Journal of the American Medical Association, Vol. 293 No. 13, April 6, 2005.
- ^ Anton R, Oroszi G, O’Malley S, Couper D, Swift R, Pettinati H, Goldman D (2008). "An Evaluation of Opioid Receptor (OPRM1) as a Predictor of Naltrexone Response in the Treatment of Alcohol Dependence". Archives of General Psychiatry 65 (2): 135–144. doi:10.1001/archpsyc.65.2.135. PMC 2666924. PMID 18250251. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2666924.
- ^ “FDA approves injectable drug to treat opoid-dependence patients,” U.S. Food and Drug Administration press announcement.
- ^ Nora D. Volkow, M.D, “Message from the Director on Important Treatment Advances for Addiction to Heroin and other Opiates,” National Institute on Drug Abuse, National Institutes of Health, October 2010.
- ^ “Alkermes Announces Positive Results from Phase 3 Clinical Study of Naltrexone for Extended-Release Injectable Suspension for the Treatment of Opioid Dependence”, Drugs.com November 16, 2009.
- ^ [|Therapeutic Goods Administration]. "Australian Register of Therapeutic Goods Medicines" (Online database of approved medicines). https://www.ebs.tga.gov.au/ebs/ANZTPAR/PublicWeb.nsf/cuMedicines?OpenView. Retrieved 2009-03-22.
- ^ Simeon, Daphne. "An Open Trial of Naltrexone in the Treatment of Depersonalization Disorder". Journal of Clinical Psychopharmacology. http://journals.lww.com/psychopharmacology/Abstract/2005/06000/An_Open_Trial_of_Naltrexone_in_the_Treatment_of.13.aspx. Retrieved 10/13/2011.
- ^ a b Novella, Steven. "Low Dose Naltrexone – Bogus or Cutting Edge Science?". http://www.sciencebasedmedicine.org/index.php/low-dose-naltrexone-bogus-or-cutting-edge-science/. Retrieved 5 July 2011.
- ^ Webster LR (August 2007). "Oxytrex: an oxycodone and ultra-low-dose naltrexone formulation". Expert Opin Investig Drugs 16 (8): 1277–83. doi:10.1517/13543784.16.8.1277. PMID 17685875.
- ^ Mannelli P, Gottheil E, Van Bockstaele EJ (2006). "Antagonist treatment of opioid withdrawal translational low dose approach". J Addict Dis 25 (2): 1–8. doi:10.1300/J069v25n02_01. PMID 16785213.
- ^ Ngian GS, Guymer EK, Littlejohn GO (February 2011). "The use of opioids in fibromyalgia" (PDF). Int J Rheum Dis 14 (1): 6–11. doi:10.1111/j.1756-185X.2010.01567.x. PMID 21303476. http://onlinelibrary.wiley.com/doi/10.1111/j.1756-185X.2010.01567.x/pdf.
- ^ Bowling, Allen C.. "Low-dose naltrexone (LDN) The “411” on LDN". National Multiple Sclerosis Society. http://www.nationalmssociety.org/multimedia-library/momentum-magazine/back-issues/momentum-spring-09/index.aspx. Retrieved 6 July 2011.
- ^ King A, de Wit H, Riley R, Cao D, Niaura R, Hatsukami D (2006). "Efficacy of naltrexone in smoking cessation: A preliminary study and an examination of sex differences". Nicotine & Tobacco Research 8 (5): 671–82. doi:10.1080/14622200600789767. PMID 17008194.
- ^ Smith, Stanley G.; Gupta, Krishan K.; Smith, Sylvia H. (June, 1995). "Effects of naltrexone on self-injury, stereotypy, and social behavior of adults with developmental disabilities". Journal of Developmental and Physical Disabilities 7 (2): 137–146. doi:10.1007/BF02684958.
- ^ Manley, Cynthia (1998-03-20). "Self-injuries may have biochemical base: study". The Reporter. http://www.mc.vanderbilt.edu/reporter/index.html?ID=461.
- ^ Grant, J (2009-04-03). "Drug Suppresses The Compulsion To Steal, Study Shows". Science daily. http://www.sciencedaily.com/releases/2009/04/090401101900.htm.
- ^ Bostwick, J. M. (2008-02-01). "Internet Sex Addiction Treated With Naltrexone". Mayo Clinic Proceedings. http://www.mayoclinicproceedings.com/content/83/2/226.long.
Antiaddictives (N07B) Nicotine dependence/
(Nicotinic agonist)Nicotine • Dianicline • Varenicline • Lobeline • Mecamylamine • Scopolamine
NDRI (Bupropion) • AA (Clonidine) • CB1 (Surinabant)Alcohol dependence AD inhibitor (Disulfiram, Calcium carbimide) • mGluR (Acamprosate) • Opioid receptor antagonists (Naltrexone, Nalmefene) • Topiramate • AA (Clonidine) • BaclofenOpioid dependence Stimulant dependence Benzodiazepine dependence Cocaine dependence Sedative-Hypnotic dependence Categories:- Opioid antagonists
- Alcohol abuse
- Morphinans
- Phenols
- Ketones
- Alcohols
- Semisynthetic opioids
- Ethers
Wikimedia Foundation. 2010.
