- Cocaine dependence
-
Cocaine dependence Classification and external resources ICD-10 F14.2 ICD-9 304.2 eMedicine med/3116 MeSH D019970 Cocaine dependence (or addiction) is a psychological desire to regularly use cocaine. It can result in cardiovascular and brain damage such as constricting blood vessels in the brain, causing strokes and constricting arteries in the heart, causing heart attacks [1]specifically in the central nervous system.
The use of cocaine can cause mood swings, paranoia, insomnia, psychosis, high blood pressure, tachycardia, panic attacks, cognitive impairments and drastic changes in the personality that can lead to aggressive, compulsive, criminal and/or erratic behaviors.
The symptoms of cocaine withdrawal (also known as comedown or crash) range from moderate to severe: dysphoria, depression, anxiety, psychological and physical weakness, pain and compulsive craving.
Historically, the addiction was known as cocainism.[2]
Contents
Risk
According to a study of 1081 US residents aged over 11 years who had used cocaine for the first time within 24 months prior to assessment, the risk of becoming cocaine-dependent within 2 years of first use (recent-onset) is 5-6%; after 10 years, it increases to 15-16%. These are the aggregate rates for all types of use considered, i.e., smoking, snorting, injecting. Among recent-onset users, the relative rates are higher for smoking (3.4 times) and much higher for injecting. They also vary, based on other characteristics, such as sex: among recent-onset users, women are 3.3 times more likely to become addicted, compared with men; age: among recent-onset users, those who started using at ages 12 or 13 were 4 times as likely to become addicted, compared with those who started between ages 18 and 20.[3]
However, a study of non-deviant[nb 1] users in Amsterdam found "relative absence of destructive and compulsive use patterns over a ten year period" and concluded that cocaine users can and do exercise control. "Our respondents applied two basic types of controls to themselves: 1) restricting use to certain situations and to emotional states in which cocaine's effects would be most positive, and 2) limiting mode of ingestion to snorting of modest amounts of cocaine, staying below 2.5 grams a week for some, and below 0.5 grams a week for most. Nevertheless, those whose use level exceeded 2.5 grams a week all returned to lower levels."[4]
Presentation
The immediate craving of the addict for more soon after use is due to the short-lived high that usually subsides within an hour, leading to prolonged, multi-dose binge use. When administration stops after binge use, it is followed by a "crash" (also known as a "come down"), the onset of severely dysphoric mood with escalating exhaustion until sleep is achieved, which is sometimes accomplished by taking sleeping medications, or sedatives, a popular one being Seroquel[citation needed], or by combination use of alcohol and cannabis. Resumption of use may occur upon awakening or may not occur for several days, but the intense euphoria of such use can, as it has in many users, produce intense craving and develop rather quickly into addiction.
Many habitual abusers develop a transient manic-like condition similar to amphetamine psychosis and schizophrenia, whose symptoms include aggression, severe paranoia, and tactile hallucinations (including the feeling of insects under the skin, or "coke bugs, also known as formication.") during binges.[5]
Cocaine has positive reinforcement effects, which refers to the effect that certain stimuli have on behavior. Good feelings become associated with the drug, causing a frequent user to take the drug as a response to bad news or mild depression. This activation strengthens the response that was just made. If the drug was taken by a fast acting route such as injection or inhalation, the response will be the act of taking more cocaine, so the response will be reinforced. Powder cocaine, being a club drug, is mostly consumed in the evening and night hours. Because cocaine is a stimulant, a user will often drink large amounts of alcohol during and after usage or smoke cannabis to dull "crash" or "come down" effects and hasten slumber. Benzodiazepines (e.g., temazepam, alprazolam, clonazepam) are also used for this purpose. Other drugs such as heroin and various pharmaceuticals are often used to amplify reinforcement or to minimize such negative effects, further increasing addiction potential and harmfulness.
Mechanism of dependence
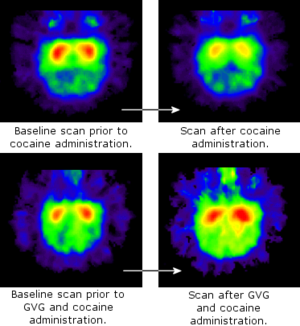 Positron Emission Tomography scans showing the average level of dopamine receptors in six primates' brains. Red is high- and blue is low-concentration of dopamine receptors. The higher the level of dopamine, the fewer receptors there will be.
Positron Emission Tomography scans showing the average level of dopamine receptors in six primates' brains. Red is high- and blue is low-concentration of dopamine receptors. The higher the level of dopamine, the fewer receptors there will be.
It is speculated that cocaine's intense addictive properties stem partially from its DAT-blocking effects (in particular, increasing the dopaminergic transmission from ventral tegmental area neurons). However, a study has shown that mice with no dopamine transporters still exhibit the rewarding effects of cocaine administration.[6] Later work demonstrated that a combined DAT/SERT knockout eliminated the rewarding effects.[7] The rewarding effects of cocaine are influenced by circadian rhythms,[8] possibly by involving a set of genes termed "clock genes".[9]
There is a correlation between a variant of the CAMK4 gene and cocaine addiction; a German study found that addicts were 25% more likely to have a variant of the gene than people who did not use cocaine.[10][11]
However, chronic cocaine addiction is not solely due to cocaine reward. Chronic repeated use is needed to produce cocaine-induced changes in brain reward centers and consequent chronic dysphoria. Dysphoria magnifies craving for cocaine because cocaine reward rapidly, albeit transiently, improves mood. This contributes to continued use and a self-perpetuating, worsening condition, since those addicted usually cannot appreciate that long-term effects are opposite those occurring immediately after use.
Treatment
A study published in May, 2008, in the journal Molecular Psychiatry, detailed the effect of long-term cocaine intake on the amount and activity of thousands of proteins in monkeys. The researchers used “proteomic” technology, which enables the simultaneous analysis of thousands of proteins, to compare the “proteome” (all proteins expressed at a given time) between a group of monkeys that self-administered cocaine and a group that did not receive the drug. The study provides a comprehensive assessment of biochemical changes occurring in the cocaine-addicted brain. The profound changes in structure, metabolism and signaling of neurons may explain why relapse occurs and why it is difficult to reverse these changes after the drug use is discontinued.[12]
On February 14, 2011 two Swiss psychologists, Dr. Geneva Francois Crespo and Dr. Sylvie Petit Jean, published two years of trials and research which demonstrates that gambling along with psychotherapy is the best method to break the cocaine addiction cycle. According to Dr. Crespo - "After cocaine is used, it activates the reward center inside the brain. The brain released euphoric hormones and neurotransmitters such as dopamine, oxytocin and adrenaline which act as a mood enhancer. The same occurs with gambling: the brain perceives a reward from winning or the potential of a reward. The reward causes intense moments of happiness, which compensate for the desire to use cocaine". Further research is being conducted on long term relapse rates.[13][14]
Withdrawal symptoms
After taking cocaine on a regular basis, the user will almost inevitably become addicted. When the drug is discontinued immediately, the user will experience what has come to be known as a "crash" along with a number of other cocaine withdrawal symptoms, including paranoia, depression, exhaustion, anxiety, itching, mood swings, irritability, fatigue, insomnia, an intense craving for more cocaine, and in some cases nausea and vomiting. Some cocaine users also report having similar symptoms to schizophrenia patients and feel that their mind is lost. Some users also report feeling a crawling sensation on the skin known as "coke bugs". These symptoms can last for weeks or, in some cases, months. Even after most withdrawal symptoms dissipate most users feel the need to continue using the drug; this feeling can last for years. About 30-40% of cocaine addicts will turn to other substances such as medication and alcohol after giving up cocaine. There are various medications on the market to ease cocaine withdrawal symptoms.[15]
Therapy
Cognitive Behavioral Therapy (CBT) combined with Motivational Therapy (MT) have proven to be effective to treat drug and alcohol addictions. Cocaine vaccines are on trial that will stop desirable effects from the drug.[16] The National Institutes of Health of US, particularly National Institute on Drug Abuse (NIDA) is researching modafinil, a narcolepsy drug and mild stimulant, as a potential cocaine treatment. Twelve-step programs such as Cocaine Anonymous (modeled on Alcoholics Anonymous) are claimed by participants to be helpful in achieving long-term abstinence; however, the 12 step based programs have no statistically-measurable effect and does not release any quantifiable measure of its success rates. Cocaine addiction continues to be the most difficult to manage behind heroin, and according to some scientists, addiction to cocaine may be almost impossible to stop. Citation Needed
Medications
Medications that have been investigated include Acetylcysteine,[17][18][19] Baclofen,[20][21] Bupropion,[22] Vanoxerine,[23] and Vigabatrin.[20] Dr. Kim Janda has been working for years on a vaccination that would cure cocaine addiction.[24]
See also
- SB-277011-A - a dopamine D3 receptor antagonist, used in the study of cocaine addiction. Where cocaine reduces the threshold for brain electrical self-stimulation in rats, an indication of cocaine's rewarding effects, SB-277011-A completely reverses this effect.
Notes
- ^ The study's authors stated that they wanted to know which effects and consequences of cocaine use would become visible with persons who are mainstream citizens or as close to that social stratum as possible
References
- ^ http://www.webmd.com/mental-health/cocaine-use-and-its-effects
- ^ Medical herald. 1891. p. 79. http://books.google.com/books?id=XMVXAAAAMAAJ&pg=PA79. Retrieved 16 June 2011.
- ^ O'Brien MS, Anthony JC (2005). "Risk of becoming cocaine dependent: epidemiological estimates for the United States, 2000–2001.". Neuropsychopharmacology 30 (5): 1006–1018. doi:10.1038/sj.npp.1300681. PMID 15785780. http://www.nature.com/npp/journal/v30/n5/full/1300681a.html.
- ^ Cohen, Peter; Sas, Arjan (1994). Cocaine use in Amsterdam in non deviant subcultures. Addiction Research, Vol. 2, No. 1, pp. 71-94.
- ^ Gawin. FH. (1991). "Cocaine addiction: Psychology and neurophysiology". Science 251 (5001): 1580–6. doi:10.1126/science.2011738. PMID 2011738.
- ^ Sora, et al.; Wichems, C; Takahashi, N; Li, XF; Zeng, Z; Revay, R; Lesch, KP; Murphy, DL et al. (June 23, 1998). "Cocaine reward models: Conditioned place preference can be established in dopamine- and in serotonin-transporter knockout mice". Proc. Natl. Acad. Sci. U.S.A. 95 (13): 7600–7704. doi:10.1073/pnas.95.13.7699. PMC 22727. PMID 9636213. http://www.pnas.org/cgi/content/full/95/13/7699.
- ^ Sora, et al.; Hall, FS; Andrews, AM; Itokawa, M; Li, XF; Wei, HB; Wichems, C; Lesch, KP et al. (April 24, 2001). "Molecular mechanisms of cocaine reward: Combined dopamine and serotonin transporter knockouts eliminate cocaine place preference". Proc. Natl. Acad. Sci. U.S.A. 98 (9): 5300–5. doi:10.1073/pnas.091039298. PMC 33204. PMID 11320258. http://www.pnas.org/cgi/content/full/98/9/5300.
- ^ Kurtuncu et al.; Arslan, AD; Akhisaroglu, M; Manev, H; Uz, T (April 12, 2004). "Involvement of the pineal gland in diurnal cocaine reward in mice". European Journal of Pharmacology 489 (3): 203–5. doi:10.1016/j.ejphar.2004.03.010. PMID 15087244.
- ^ Yuferov V, Butelman ER, Kreek MJ (2005). "Biological clock: biological clocks may modulate drug addiction". Eur. J. Hum. Genet. 13 (10): 1101–3. doi:10.1038/sj.ejhg.5201483. PMID 16094306.
- ^ Ian Sample (2009-11-11). "All in the family - scientists discover gene for cocaine addiction". The Guardian. http://www.guardian.co.uk/science/2008/nov/11/drugs-drugsandalcohol.
- ^ Bilbao, A; Parkitna, JR; Engblom, D; Perreau-Lenz, S; Sanchis-Segura, C; Schneider, M; Konopka, W; Westphal, M et al. (2008). "Loss of the Ca2+/calmodulin-dependent protein kinase type IV in dopaminoceptive neurons enhances behavioral effects of cocaine". Proc. Natl. Acad. Sci. U.S.A. 105 (45): 17549–54. doi:10.1073/pnas.0803959105. PMC 2582267. PMID 19001277. http://www.pnas.org/content/105/45/17549.abstract.
- ^ Newswise: Research Reveals Molecular Fingerprint of Cocaine Addiction
- ^ Der Standard: Stimulus to stimulus in the race (in German)
- ^ BlackJack Champ News: Swiss docs prove gambling cure for cocaine users
- ^ Cocaine withdrawal Symptoms Resource
- ^ "Baylor Doctors are Working on Cocaine Vaccine". CocaineHelp.org. January 17, 2008. http://www.cocainehelp.org/Article75641.html. Retrieved 2008-09-11.
- ^ Mardikian PN, LaRowe SD, Hedden S, Kalivas PW, Malcolm RJ (March 2007). "An open-label trial of N-acetylcysteine for the treatment of cocaine dependence: a pilot study". Prog. Neuropsychopharmacol. Biol. Psychiatry 31 (2): 389–94. doi:10.1016/j.pnpbp.2006.10.001. PMID 17113207.
- ^ LaRowe SD, Myrick H, Hedden S, et al. (July 2007). "Is cocaine desire reduced by N-acetylcysteine?". Am J Psychiatry 164 (7): 1115–7. doi:10.1176/appi.ajp.164.7.1115. PMID 17606664.
- ^ Gass JT, Olive MF (January 2008). "Glutamatergic substrates of drug addiction and alcoholism". Biochem. Pharmacol. 75 (1): 218–65. doi:10.1016/j.bcp.2007.06.039. PMC 2239014. PMID 17706608. http://linkinghub.elsevier.com/retrieve/pii/S0006-2952(07)00418-2.
- ^ a b Karila L, Gorelick D, Weinstein A, et al. (May 2008). "New treatments for cocaine dependence: a focused review". Int. J. Neuropsychopharmacol. 11 (3): 425–38. doi:10.1017/S1461145707008097. PMID 17927843. http://journals.cambridge.org/abstract_S1461145707008097.
- ^ Ling W, Shoptaw S, Majewska D (May 1998). "Baclofen as a cocaine anti-craving medication: a preliminary clinical study". Neuropsychopharmacology 18 (5): 403–4. doi:10.1016/S0893-133X(97)00128-0. PMID 9536455. http://www.nature.com/npp/journal/v18/n5/full/1395109a.html.
- ^ Margolin A, Kosten TR, Avants SK, et al. (December 1995). "A multicenter trial of bupropion for cocaine dependence in methadone-maintained patients". Drug Alcohol Depend 40 (2): 125–31. doi:10.1016/0376-8716(95)01198-6. PMID 8745134. http://linkinghub.elsevier.com/retrieve/pii/0376871695011986.
- ^ Cherstniakova SA, Bi D, Fuller DR, Mojsiak JZ, Collins JM, Cantilena LR (September 2001). "Metabolism of vanoxerine, 1-[2-[bis(4-fluorophenyl)methoxyethyl]-4-(3-phenylpropyl)piperazine, by human cytochrome P450 enzymes"]. Drug Metab. Dispos. 29 (9): 1216–20. PMID 11502731. http://dmd.aspetjournals.org/cgi/pmidlookup?view=long&pmid=11502731.
- ^ Douglas Quenqua (3 Oct 2011). "An Addiction Vaccine, Tantalizingly Close". New York Times. http://www.nytimes.com/2011/10/04/health/04vaccine.html?hp.
Psychoactive substance-related disorder (F10–F19, 291–292; 303–305) General Alcohol Opioids Cannabis Sedative/hypnotic benzodiazepine: SID (Benzodiazepine overdose, Benzodiazepine withdrawal) · SUD (Benzodiazepine drug misuse, Benzodiazepine dependence)Cocaine Stimulants SID (Stimulant psychosis) · SUD (Amphetamine dependence) · Health effects of caffeine (Caffeine-induced sleep disorder)Hallucinogen Tobacco Volatile solvents Multiple Categories:
Wikimedia Foundation. 2010.
