- Multiple sclerosis
-
Multiple sclerosis Classification and external resources 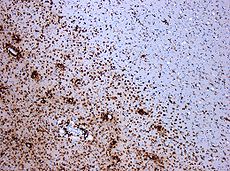
Demyelination by MS. The CD68 colored tissue shows several macrophages in the area of the lesion. Original scale 1:100ICD-10 G35 ICD-9 340 OMIM 126200 DiseasesDB 8412 MedlinePlus 000737 eMedicine neuro/228 oph/179 emerg/321 pmr/82 radio/461 MeSH D009103 GeneReviews Multiple Sclerosis Overview Multiple sclerosis (abbreviated MS, known as disseminated sclerosis or encephalomyelitis disseminata) is an inflammatory disease in which the fatty myelin sheaths around the axons of the brain and spinal cord are damaged, leading to demyelination and scarring as well as a broad spectrum of signs and symptoms.[1] Disease onset usually occurs in young adults, and it is more common in women.[1] It has a prevalence that ranges between 2 and 150 per 100,000.[2] MS was first described in 1868 by Jean-Martin Charcot.[3]
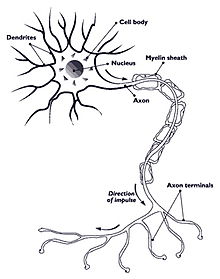
MS affects the ability of nerve cells in the brain and spinal cord to communicate with each other effectively. Nerve cells communicate by sending electrical signals called action potentials down long fibers called axons, which are contained within an insulating substance called myelin. In MS, the body's own immune system attacks and damages the myelin. When myelin is lost, the axons can no longer effectively conduct signals.[4] The name multiple sclerosis refers to scars (scleroses—better known as plaques or lesions) particularly in the white matter of the brain and spinal cord, which is mainly composed of myelin.[3] Although much is known about the mechanisms involved in the disease process, the cause remains unknown. Theories include genetics or infections. Different environmental risk factors have also been found.[4][5]
Almost any neurological symptom can appear with the disease, and often progresses to physical and cognitive disability.[4] MS takes several forms, with new symptoms occurring either in discrete attacks (relapsing forms) or slowly accumulating over time (progressive forms).[6] Between attacks, symptoms may go away completely, but permanent neurological problems often occur, especially as the disease advances.[6]
There is no known cure for multiple sclerosis. Treatments attempt to return function after an attack, prevent new attacks, and prevent disability.[4] MS medications can have adverse effects or be poorly tolerated, and many patients pursue alternative treatments, despite the lack of supporting scientific study. The prognosis is difficult to predict; it depends on the subtype of the disease, the individual patient's disease characteristics, the initial symptoms and the degree of disability the person experiences as time advances.[7] Life expectancy of people with MS is 5 to 10 years lower than that of the unaffected population.[1]
Contents
Classification
Several subtypes, or patterns of progression, have been described. Subtypes use the past course of the disease in an attempt to predict the future course. They are important not only for prognosis but also for therapeutic decisions. In 1996 the United States National Multiple Sclerosis Society standardized four subtype definitions:[6]
- relapsing remitting,
- secondary progressive,
- primary progressive, and
- progressive relapsing.
The relapsing-remitting subtype is characterized by unpredictable relapses followed by periods of months to years of relative quiet (remission) with no new signs of disease activity. Deficits suffered during attacks may either resolve or leave sequelae, the latter being more common as a function of time.[1] This describes the initial course of 80% of individuals with MS.[1] When deficits always resolve between attacks, this is sometimes referred to as benign MS,[8] although patients will still accrue some degree of disability in the long term.[1] The relapsing-remitting subtype usually begins with a clinically isolated syndrome (CIS). In CIS, a patient has an attack suggestive of demyelination, but does not fulfill the criteria for multiple sclerosis.[1][9] However only 30 to 70% of persons experiencing CIS later develop MS.[9]
Secondary progressive MS (sometimes called "galloping MS") describes around 65% of those with an initial relapsing-remitting MS, who then begin to have progressive neurologic decline between acute attacks without any definite periods of remission.[1][6] Occasional relapses and minor remissions may appear.[6] The median time between disease onset and conversion from relapsing-remitting to secondary progressive MS is 19 years.[10] The primary progressive subtype describes the approximately 10–15% of individuals who never have remission after their initial MS symptoms.[11] It is characterized by progression of disability from onset, with no, or only occasional and minor, remissions and improvements.[6] The age of onset for the primary progressive subtype is later than for the relapsing-remitting, but similar to mean age of progression between the relapsing-remitting and the secondary progressive. In both cases it is around 40 years of age.[1]
Progressive relapsing MS describes those individuals who, from onset, have a steady neurologic decline but also suffer clear superimposed attacks. This is the least common of all subtypes.[6]
Atypical variants of MS with non-standard behavior have been described; these include Devic's disease, Balo concentric sclerosis, Schilder's diffuse sclerosis and Marburg multiple sclerosis. There is debate on whether they are MS variants or different diseases.[12] Multiple sclerosis also behaves differently in children, taking more time to reach the progressive stage.[1] Nevertheless they still reach it at a lower mean age than adults.[1]
Signs and symptoms
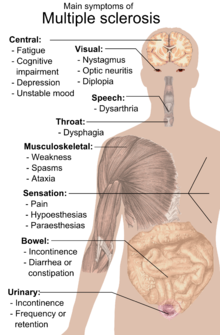
A person with MS can suffer almost any neurological symptom or sign, including changes in sensation such as loss of sensitivity or tingling, pricking or numbness (hypoesthesia and paresthesia), muscle weakness, clonus, muscle spasms, or difficulty in moving; difficulties with coordination and balance (ataxia); problems in speech (dysarthria) or swallowing (dysphagia), visual problems (nystagmus, optic neuritis including phosphenes,[13][14] or diplopia), fatigue, acute or chronic pain, and bladder and bowel difficulties.[1] Cognitive impairment of varying degrees and emotional symptoms of depression or unstable mood are also common.[1] Uhthoff's phenomenon, an exacerbation of extant symptoms due to an exposure to higher than usual ambient temperatures, and Lhermitte's sign, an electrical sensation that runs down the back when bending the neck, are particularly characteristic of MS although not specific.[1] The main clinical measure of disability progression and symptom severity is the Expanded Disability Status Scale or EDSS.[15]
Symptoms of MS usually appear in episodic acute periods of worsening (called relapses, exacerbations, bouts, attacks, or "flare-ups"), in a gradually progressive deterioration of neurologic function, or in a combination of both.[6] Multiple sclerosis relapses are often unpredictable, occurring without warning and without obvious inciting factors with a rate rarely above one and a half per year.[1] Some attacks, however, are preceded by common triggers. Relapses occur more frequently during spring and summer.[16] Viral infections such as the common cold, influenza, or gastroenteritis increase the risk of relapse.[1] Stress may also trigger an attack.[17] Pregnancy affects the susceptibility to relapse, with a lower relapse rate at each trimester of gestation. During the first few months after delivery, however, the risk of relapse is increased.[1] Overall, pregnancy does not seem to influence long-term disability. Many potential triggers have been examined and found not to influence MS relapse rates. There is no evidence that vaccination and breast feeding,[1] physical trauma,[18] or Uhthoff's phenomenon[16] are relapse triggers.
Causes
Most likely MS occurs as a result of some combination of genetic, environmental and infectious factors,[1] and possibly other factors like vascular problems.[19] Epidemiological studies of MS have provided hints on possible causes for the disease. Theories try to combine the known data into plausible explanations, but none has proved definitive.
Genetics
MS is not considered a hereditary disease. However, a number of genetic variations have been shown to increase the risk of developing the disease.[20]
The risk of acquiring MS is higher in relatives of a person with the disease than in the general population, especially in the case of siblings, parents, and children.[4] The disease has an overall familial recurrence rate of 20%.[1] In the case of monozygotic twins, concordance occurs only in about 35% of cases, while it goes down to around 5% in the case of siblings and even lower in half-siblings. This indicates susceptibility is partly polygenically driven.[1][4]
It seems to be more common in some ethnic groups than others.[21]
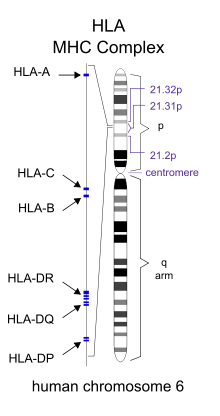
Apart from familial studies, specific genes have been linked with MS. Differences in the human leukocyte antigen (HLA) system—a group of genes in chromosome 6 that serves as the major histocompatibility complex (MHC) in humans—increase the probability of suffering MS.[1] The most consistent finding is the association between multiple sclerosis and alleles of the MHC defined as DR15 and DQ6.[1] Other loci have shown a protective effect, such as HLA-C554 and HLA-DRB1*11.[1]
Environmental factors
Different environmental factors, both of infectious and non infectious origin have been proposed as risk factors for MS. Although some are partly modifiable, only further research—especially clinical trials—will reveal whether their elimination can help prevent MS.[22]
MS is more common in people who live farther from the equator, although many exceptions exist.[1] Decreased sunlight exposure has been linked with a higher risk of MS.[22] Decreased vitamin D production and intake has been the main biological mechanism used to explain the higher risk among those less exposed to sun.[22][23][24]
Severe stress may also be a risk factor although evidence is weak.[22] Smoking has also been shown to be an independent risk factor for developing MS.[23] Association with occupational exposures and toxins—mainly solvents—has been evaluated, but no clear conclusions have been reached.[22]Vaccinations were also considered as causal factors for the disease; however, most studies show no association between MS and vaccines.[22] Several other possible risk factors, such as diet[25] and hormone intake, have been investigated; however, evidence on their relation with the disease is "sparse and unpersuasive".[23]
Gout occurs less than would statistically be expected in people with MS, and low levels of uric acid have been found in MS patients as compared to normal individuals. This led to the theory that uric acid protects against MS, although its exact importance remains unknown.[26]
Infections
Many microbes have been proposed as potential infectious triggers of MS, but none have been substantiated.[4]
Genetic susceptibility can explain some of the geographic and epidemiological variations in MS incidence, like the high incidence of the disease among some families or the risk decline with genetic distance, but does not account for other phenomena, such as the changes in risk that occur with migration at an early age.[5] An explanation for this epidemiological finding could be that some kind of infection, produced by a widespread microbe rather than a rare pathogen, is the origin of the disease.[5] Different hypotheses have elaborated on the mechanism by which this may occur. The hygiene hypothesis proposes that exposure to several infectious agents early in life is protective against MS, the disease being a response to a later encounter with such agents.[1] The prevalence hypothesis proposes that the disease is due to a pathogen more common in regions of high MS prevalence. This pathogen is very common, causing in most individuals an asymptomatic persistent infection. Only in a few cases, and after many years since the original infection, does it cause demyelination.[5][27] The hygiene hypothesis has received more support than the prevalence hypothesis.[5]
Evidence for viruses as a cause includes the presence of oligoclonal bands in the brain and cerebrospinal fluid of most patients, the association of several viruses with human demyelination encephalomyelitis, and induction of demyelination in animals through viral infection.[28] Human herpes viruses are a candidate group of viruses linked to MS. Individuals who have never been infected by the Epstein-Barr virus have a reduced risk of having the disease, and those infected as young adults have a greater risk than those who had it at a younger age.[1][5] Although some consider that this goes against the hygiene hypothesis, since the non-infected have probably experienced a more hygienic upbringing,[5] others believe that there is no contradiction since it is a first encounter at a later moment with the causative virus that is the trigger for the disease.[1] Other diseases that have also been related with MS are measles, mumps and rubella.[1]
Pathophysiology
Blood-brain barrier breakdown
The blood–brain barrier is a capillary system that should prevent entrance of T cells into the nervous system.[4] The blood–brain barrier is normally not permeable to these types of cells, unless triggered by infection or a virus, which decreases the integrity of the tight junctions forming the barrier.[4] When the blood–brain barrier regains its integrity, usually after infection or virus has cleared, the T cells are trapped inside the brain.[4]
Autoimmunology
MS is currently believed to be an immune-mediated disorder mediated by a complex interaction of the individual's genetics and as yet unidentified environmental insults.[4] Damage is believed to be caused by the patient's own immune system. The immune system attacks the nervous system, possibly as a result of exposure to a molecule with a similar structure to one of its own.[4]
- Lesions
The name multiple sclerosis refers to the scars (scleroses – better known as plaques or lesions) that form in the nervous system. MS lesions most commonly involve white matter areas close to the ventricles of the cerebellum, brain stem, basal ganglia and spinal cord; and the optic nerve. The function of white matter cells is to carry signals between grey matter areas, where the processing is done, and the rest of the body. The peripheral nervous system is rarely involved.[4]
More specifically, MS destroys oligodendrocytes, the cells responsible for creating and maintaining a fatty layer—known as the myelin sheath—which helps the neurons carry electrical signals.[4] MS results in a thinning or complete loss of myelin and, as the disease advances, the cutting (transection) of the neuron's extensions or axons. When the myelin is lost, a neuron can no longer effectively conduct electrical signals.[4] A repair process, called remyelination, takes place in early phases of the disease, but the oligodendrocytes cannot completely rebuild the cell's myelin sheath.[29] Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons.[29] Different lesion patterns have been described.[30]
- Inflammation
Apart from demyelination, the other pathologic hallmark of the disease is inflammation. According to a strictly immunological explanation of MS, the inflammatory process is caused by T cells, a kind of lymphocyte. Lymphocytes are cells that play an important role in the body's defenses.[4] In MS, T cells gain entry into the brain via the previously described blood–brain barrier. Evidence from animal models also point to a role of B cells in addition to T cells in development of the disease.[31]
The T cells recognize myelin as foreign and attack it as if it were an invading virus. This triggers inflammatory processes, stimulating other immune cells and soluble factors like cytokines and antibodies. Leaks form in the blood–brain barrier, which in turn cause a number of other damaging effects such as swelling, activation of macrophages, and more activation of cytokines and other destructive proteins.[4]
Diagnosis
 T1-weighted MRI scans (post-contrast) of the same brain slice at monthly intervals. Bright spots indicate active lesions.
T1-weighted MRI scans (post-contrast) of the same brain slice at monthly intervals. Bright spots indicate active lesions.
Multiple sclerosis can be difficult to diagnose since its signs and symptoms may be similar to other medical problems.[1][32] Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process especially in the first stages of the disease.[1] Historically, the Schumacher and Poser criteria were both popular.[33]
Currently, the McDonald criteria focus on a demonstration with clinical, laboratory and radiologic data of the dissemination of MS lesions in time and space for non-invasive MS diagnosis, though some have stated that the only proved diagnosis of MS is autopsy, or occasionally biopsy, where lesions typical of MS can be detected through histopathological techniques.[1][34][35]
Clinical data alone may be sufficient for a diagnosis of MS if an individual has suffered separate episodes of neurologic symptoms characteristic of MS.[34] Since some people seek medical attention after only one attack, other testing may hasten and ease the diagnosis. The most commonly used diagnostic tools are neuroimaging, analysis of cerebrospinal fluid and evoked potentials. Magnetic resonance imaging of the brain and spine shows areas of demyelination (lesions or plaques). Gadolinium can be administered intravenously as a contrast to highlight active plaques and, by elimination, demonstrate the existence of historical lesions not associated with symptoms at the moment of the evaluation.[34][36] Testing of cerebrospinal fluid obtained from a lumbar puncture can provide evidence of chronic inflammation of the central nervous system. The cerebrospinal fluid is tested for oligoclonal bands of IgG on electrophoresis, which are inflammation markers found in 75–85% of people with MS.[34][37] The nervous system of a person with MS responds less actively to stimulation of the optic nerve and sensory nerves due to demyelination of such pathways. These brain responses can be examined using visual and sensory evoked potentials.[38]
Management
Although there is no known cure for multiple sclerosis, several therapies have proven helpful. The primary aims of therapy are returning function after an attack, preventing new attacks, and preventing disability. As with any medical treatment, medications used in the management of MS have several adverse effects. Alternative treatments are pursued by some patients, despite the shortage of supporting, comparable, replicated scientific study.
Acute attacks
During symptomatic attacks, administration of high doses of intravenous corticosteroids, such as methylprednisolone, is the routine therapy for acute relapses.[1] Although generally effective in the short term for relieving symptoms, corticosteroid treatments do not appear to have a significant impact on long-term recovery.[39] Oral and intravenous administration seem to have similar efficacy.[40] Consequences of severe attacks which do not respond to corticosteroids might be treated by plasmapheresis.[1]
Disease-modifying treatments
Fingolimod (trade name Gilenya) was approved for MS by the FDA in 2010, and in Europe in 2011. As of 2011[update], after this approval, there are six disease-modifying treatments for MS approved by regulatory agencies of various countries, being the other five: Interferon beta-1a (trade names Avonex, CinnoVex, ReciGen and Rebif) and interferon beta-1b (U.S. trade name Betaseron, in Europe and Japan Betaferon). A third medication is glatiramer acetate (Copaxone), a non-interferon, non-steroidal immunomodulator. The fourth medication, mitoxantrone, is an immunosuppressant also used in cancer chemotherapy. The fifth is a humanized monoclonal antibody immunomodualtor, natalizumab (marketed as Tysabri).[1] The interferons and glatiramer acetate are delivered by frequent injections, varying from once-per-day for glatiramer acetate to once-per-week (but intra-muscular) for Avonex. Natalizumab and mitoxantrone are given by IV infusion at monthly intervals.
All six kinds of medications are modestly effective at decreasing the number of attacks in relapsing-remitting MS (RRMS) while the capacity of interferons and glatiramer acetate is more controversial. Studies of their long-term effects are still lacking.[1][41] Comparisons between immunomodulators (all but mitoxantrone) show that the most effective is natalizumab, both in terms of relapse rate reduction and halting disability progression.[42] Mitoxantrone may be the most effective of them all; however, it is generally not considered as a long-term therapy, as its use is limited by severe secondary effects.[1][41] The earliest clinical presentation of RRMS is the clinically isolated syndrome (CIS). Treatment with interferons during an initial attack can decrease the chance that a patient will develop clinical MS.[1]
Treatment of progressive MS is more difficult than relapsing-remitting MS. Mitoxantrone has shown positive effects in patients with secondary progressive and progressive relapsing courses. It is moderately effective in reducing the progression of the disease and the frequency of relapses in patients in short-term follow-up.[43] No treatment has been proven to modify the course of primary progressive MS.[44]
As with many medical treatments, these treatments have several adverse effects. One of the most common is irritation at the injection site for glatiramer acetate and the interferon treatments. Over time, a visible dent at the injection site, due to the local destruction of fat tissue, known as lipoatrophy, may develop. Interferons produce symptoms similar to influenza;[45] some patients taking glatiramer experience a post-injection reaction manifested by flushing, chest tightness, heart palpitations, breathlessness, and anxiety, which usually lasts less than thirty minutes.[46] More dangerous but much less common are liver damage from interferons,[47] severe cardiotoxicity, infertility, and acute myeloid leukemia of mitoxantrone,[1][41] and the putative link between natalizumab and some cases of progressive multifocal leukoencephalopathy.[1]
Management of the effects of MS
Disease-modifying treatments reduce the progression rate of the disease, but do not stop it. As multiple sclerosis progresses, the symptomatology tends to increase. The disease is associated with a variety of symptoms and functional deficits that result in a range of progressive impairments and disability. Management of these deficits is therefore very important. Both drug therapy and neurorehabilitation have shown to ease the burden of some symptoms, though neither influences disease progression.[1][48] Some symptoms have a good response to medication, such as unstable bladder and spasticity, while management of many others is much more complicated.[1] As for any patient with neurologic deficits, a multidisciplinary approach is key to improving quality of life; however, there are particular difficulties in specifying a 'core team' because people with MS may need help from almost any health profession or service at some point.[1] Multidisciplinary rehabilitation programs increase activity and participation of patients but do not influence impairment level.[49]
Historically, individuals suffering from MS were advised against participation in physical activity due to worsening symptoms.[50] However, under the direction of a physiotherapist, participation in physical activity can be safe and has been proven beneficial for patients with MS.[51] Research has supported the rehabilitative role of physical activity in improving muscle power,[52] mobility,[52] mood,[53] bowel health,[54] general conditioning and quality of life.[52] However, it is important to be cautious about not overworking or overheating the patient during the course of exercise. Physiotherapists have the expertise needed to adequately prescribe exercise programs that are suitable for the individual. The FITT equation (frequency of exercise, intensity of exercise, type of exercise and time/duration of exercise) is typically used to prescribe exercises.[51] Depending on the patient, activities may include resistance training,[55] walking, swimming, yoga, tai chi, and others.[54] Determining an appropriate and safe exercise program is challenging and must be carefully individualized to each patient being sure to account for all contraindications and precautions.[51]
Alternative treatments
As with most chronic diseases, alternative treatments for multiple sclerosis, which are unsupported by clinical or scientific evidence, are pursued by some patients.[56] Examples are a dietary regimen,[57] herbal medicine (including the use of medical cannabis),[58] hyperbaric oxygenation[59] and self-infection with hookworm (known generally as helminthic therapy).[60]
Prognosis
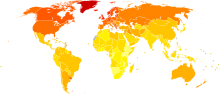 Disability-adjusted life year for multiple sclerosis per 100,000 inhabitants in 2004
Disability-adjusted life year for multiple sclerosis per 100,000 inhabitants in 2004 no dataless than 1313–1616–1919–2222–2525–2828–3131–3434–3737–4040–43more than 43
no dataless than 1313–1616–1919–2222–2525–2828–3131–3434–3737–4040–43more than 43The prognosis (the expected future course of the disease) for a person with multiple sclerosis depends on the subtype of the disease; the individual's sex, age, and initial symptoms; and the degree of disability the person experiences.[7] The disease evolves and advances over decades, 30 being the mean years to death since onset.[1]
Female sex, relapsing-remitting subtype, optic neuritis or sensory symptoms at onset, few attacks in the initial years and especially early age at onset, are associated with a better course.[7][61]
The life expectancy of people with MS is 5 to 10 years lower than that of unaffected people.[1] Almost 40% of patients reach the seventh decade of life.[61] Nevertheless, two-thirds of the deaths in people with MS are directly related to the consequences of the disease.[1] Suicide also has a higher prevalence than in the healthy population, while infections and complications are especially hazardous for the more disabled ones.[1]
Although most patients lose the ability to walk prior to death, 90% are still capable of independent walking at 10 years from onset, and 75% at 15 years.[61][62]
Epidemiology
Two main measures are used in epidemiological studies: incidence and prevalence. Incidence is the number of new cases per unit of person–time at risk (usually number of new cases per thousand person–years); while prevalence is the total number of cases of the disease in the population at a given time. Prevalence is known to depend not only on incidence, but also on survival rate and migrations of affected people. MS has a prevalence that ranges between 2 and 150 per 100,000 depending on the country or specific population.[2] Studies on populational and geographical patterns of epidemiological measures have been very common in MS,[27] and have led to the proposal of different etiological (causal) theories.[5][22][23][27]
MS usually appears in adults in their thirties but it can also appear in children.[1] The primary progressive subtype is more common in people in their fifties.[11] As with many autoimmune disorders, the disease is more common in women, and the trend may be increasing.[1][63] In children, the sex ratio difference is higher,[1] while in people over fifty, MS affects males and females almost equally.[11]
There is a north-to-south gradient in the northern hemisphere and a south-to-north gradient in the southern hemisphere, with MS being much less common in people living near the equator.[1][63] Climate, sunlight and intake of vitamin D have been investigated as possible causes of the disease that could explain this latitude gradient.[23] However, there are important exceptions to the north–south pattern and changes in prevalence rates over time;[1] in general, this trend might be disappearing.[63] This indicates that other factors such as environment or genetics have to be taken into account to explain the origin of MS.[1] MS is also more common in regions with northern Europe populations.[1] But even in regions where MS is common, some ethnic groups are at low risk of developing the disease, including the Samis, Turkmen, Amerindians, Canadian Hutterites, Africans, and New Zealand Māori.[64]
Environmental factors during childhood may play an important role in the development of MS later in life. Several studies of migrants show that if migration occurs before the age of 15, the migrant acquires the new region's susceptibility to MS. If migration takes place after age 15, the migrant retains the susceptibility of his home country.[1][22] However, the age–geographical risk for developing multiple sclerosis may span a larger timescale.[1] A relationship between season of birth and MS has also been found which lends support to an association with sunlight and vitamin D. For example fewer people with MS are born in November as compared to May.[65]
History
Medical discovery
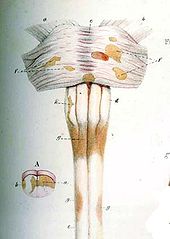
The French neurologist Jean-Martin Charcot (1825–1893) was the first person to recognize multiple sclerosis as a distinct disease in 1868.[66] Summarizing previous reports and adding his own clinical and pathological observations, Charcot called the disease sclerose en plaques. The three signs of MS now known as Charcot's triad 1 are nystagmus, intention tremor, and telegraphic speech, though these are not unique to MS. Charcot also observed cognition changes, describing his patients as having a "marked enfeeblement of the memory" and "conceptions that formed slowly".[3]
Prior to Charcot, Robert Carswell (1793–1857), a British professor of pathology, and Jean Cruveilhier (1791–1873), a French professor of pathologic anatomy, had described and illustrated many of the disease's clinical details, but did not identify it as a separate disease.[66] Specifically, Carswell described the injuries he found as "a remarkable lesion of the spinal cord accompanied with atrophy".[1] Under the microscope, Swiss pathologist Georg Eduard Rindfleisch (1836–1908) noted in 1863 that the inflammation-associated lesions were distributed around blood vessels.[67][68]
After Charcot's description, Eugène Devic (1858–1930), Jozsef Balo (1895–1979), Paul Ferdinand Schilder (1886–1940), and Otto Marburg (1874–1948) described special cases of the disease. During all the 20th century there was an important development on the theories about the cause and pathogenesis of MS while efficacious treatments began to appear in 1990.[1]
Historical cases
There are several historical accounts of people who lived before or shortly after the disease was described by Charcot and probably had MS.
A young woman called Halldora, who lived in Iceland around 1200, suddenly lost her vision and mobility, but after praying to the saints, recovered them seven days after. Saint Lidwina of Schiedam (1380–1433), a Dutch nun, may be one of the first clearly identifiable MS patients. From the age of 16 until her death at 53, she suffered intermittent pain, weakness of the legs, and vision loss—symptoms typical of MS.[69] Both cases have led to the proposal of a 'Viking gene' hypothesis for the dissemination of the disease.[70]
Augustus Frederick d'Este (1794–1848), son of Prince Augustus Frederick, Duke of Sussex and Lady Augusta Murray and the grandson of George III of the United Kingdom, almost certainly suffered from MS. D'Este left a detailed diary describing his 22 years living with the disease. His diary began in 1822 and ended in 1846, although it remained unknown until 1948. His symptoms began at age 28 with a sudden transient visual loss (amaurosis fugax) after the funeral of a friend. During the course of his disease, he developed weakness of the legs, clumsiness of the hands, numbness, dizziness, bladder disturbances, and erectile dysfunction. In 1844, he began to use a wheelchair. Despite his illness, he kept an optimistic view of life.[71][72]
Another early account of MS was kept by the British diarist W. N. P. Barbellion, nom-de-plume of Bruce Frederick Cummings (1889–1919), who maintained a detailed log of his diagnosis and struggle with MS.[72] His diary was published in 1919 as The Journal of a Disappointed Man.[73]
Research directions
Therapies
Research directions on MS treatments include investigations of MS pathogenesis and heterogeneity; research of more effective, convenient, or tolerable new treatments for RRMS; creation of therapies for the progressive subtypes; neuroprotection strategies; and the search for effective symptomatic treatments.[74] A number of treatments that may curtail attacks or improve function are under investigation. Emerging agents for RRMS that have shown promise in phase 2 trials include alemtuzumab (trade name Campath), daclizumab (trade name Zenapax), rituximab, dirucotide, BHT-3009, cladribine, dimethyl fumarate, estriol, fingolimod, laquinimod, minocycline, statins, temsirolimus and teriflunomide.[74]
In 2010, an FDA committee recommended approving fingolimod for the treatment of MS attacks,[75] and on September 22, 2010, fingolimod (trade name Gilenya) became the first oral drug approved by the Food and Drug Administration to reduce relapses and delay disability progression in patients with relapsing forms of multiple sclerosis.[76] Clinical trials of fingolimod have demonstrated side effects in treated patients, including cardiovascular conditions, macular edema, infections, liver toxicity and malignancies.[77][78]
Much interest has been focused on the prospect of utilizing vitamin D analogs in the prevention and management of CIS and MS, especially given its possible role in the pathogenesis of the disease. While there is anecdotal evidence of benefit for low dose naltrexone,[79] only results from a pilot study in primary progressive MS have been published.[80]
Disease biomarkers
The variable clinical presentation of MS and the lack of diagnostic laboratory tests lead to delays in diagnosis and the impossibility of predicting diagnosis. New diagnostic methods are being investigated. These include work with anti-myelin antibodies, analysis of microarray gene expression and studies with serum and cerebrospinal fluid but none of them has yielded reliable positive results.[81]
Currently there are no clinically established laboratory investigations available that can predict prognosis. However, several promising approaches have been proposed. Investigations on the prediction of evolution have centered on monitoring disease activity. Disease activation biomarkers include interleukin-6, nitric oxide and nitric oxide synthase, osteopontin, and fetuin-A.[81] On the other hand since disease progression is the result of neurodegeneration the roles of proteins indicative of neuronal, axonal, and glial loss such as neurofilaments, tau and N-acetylaspartate are under investigation.[81]
A final investigative field is work with biomarkers that distinguish between medication responders and nonresponders.[81]
Chronic cerebrospinal venous insufficiency
In 2008, Italian vascular surgeon Paolo Zamboni reported research suggesting that MS involves a vascular disease process he referred to as chronic cerebrospinal venous insufficiency (CCSVI, CCVI), in which veins from the brain are constricted. He found CCSVI in the majority of MS patients, performed a surgical procedure to correct it and claimed that 73% of patients improved.[82] Concern has been raised with Zamboni's research as it was neither blinded nor controlled[83] and further studies have had variable results.[84] This has raised serious objections to the hypothesis of CCSVI originating multiple sclerosis.[85] The neurology community currently recommends not to use the proposed treatment until its effectiveness is confirmed by controlled studies, the need for which has been recognized by the scientific bodies engaged in MS research.[86]
See also
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf Compston A, Coles A (October 2008). "Multiple sclerosis". Lancet 372 (9648): 1502–17. doi:10.1016/S0140-6736(08)61620-7. PMID 18970977.
- ^ a b Rosati G (April 2001). "The prevalence of multiple sclerosis in the world: an update". Neurol. Sci. 22 (2): 117–39. doi:10.1007/s100720170011. PMID 11603614.
- ^ a b c Clanet M (June 2008). "Jean-Martin Charcot. 1825 to 1893" (PDF). Int MS J 15 (2): 59–61. PMID 18782501. http://www.msforum.net/Site/ViewPDF/ViewPDF.aspx?ArticleID=E80DC748-5048-4BD2-9393-18BCAE0A1514&doctype=Article.
* Charcot, J. (1868). "Histologie de la sclerose en plaques". Gazette des hopitaux, Paris 41: 554–5. - ^ a b c d e f g h i j k l m n o p q Compston A, Coles A (April 2002). "Multiple sclerosis". Lancet 359 (9313): 1221–31. doi:10.1016/S0140-6736(02)08220-X. PMID 11955556.
- ^ a b c d e f g h Ascherio A, Munger KL (April 2007). "Environmental risk factors for multiple sclerosis. Part I: the role of infection". Ann. Neurol. 61 (4): 288–99. doi:10.1002/ana.21117. PMID 17444504.
- ^ a b c d e f g h Lublin FD, Reingold SC (April 1996). "Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis". Neurology 46 (4): 907–11. PMID 8780061.
- ^ a b c Weinshenker BG (1994). "Natural history of multiple sclerosis". Ann. Neurol. 36 (Suppl): S6–11. doi:10.1002/ana.410360704. PMID 8017890.
- ^ Pittock SJ, Rodriguez M (2008). "Benign multiple sclerosis: a distinct clinical entity with therapeutic implications". Curr. Top. Microbiol. Immunol.. Current Topics in Microbiology and Immunology 318: 1–17. doi:10.1007/978-3-540-73677-6_1. ISBN 978-3-540-73676-9. PMID 18219812.
- ^ a b Miller D, Barkhof F, Montalban X, Thompson A, Filippi M (May 2005). "Clinically isolated syndromes suggestive of multiple sclerosis, part I: natural history, pathogenesis, diagnosis, and prognosis". Lancet Neurol 4 (5): 281–8. doi:10.1016/S1474-4422(05)70071-5. PMID 15847841.
- ^ Rovaris M, Confavreux C, Furlan R, Kappos L, Comi G, Filippi M (April 2006). "Secondary progressive multiple sclerosis: current knowledge and future challenges". Lancet Neurol 5 (4): 343–54. doi:10.1016/S1474-4422(06)70410-0. PMID 16545751.
- ^ a b c Miller DH, Leary SM (October 2007). "Primary-progressive multiple sclerosis". Lancet Neurol 6 (10): 903–12. doi:10.1016/S1474-4422(07)70243-0. PMID 17884680.
- ^ Stadelmann C, Brück W (November 2004). "Lessons from the neuropathology of atypical forms of multiple sclerosis". Neurol. Sci. 25 (Suppl 4): S319–22. doi:10.1007/s10072-004-0333-1. PMID 15727225.
- ^ Davis FA, Bergen D, Schauf C, McDonald I, Deutsch W (November 1976). "Movement phosphenes in optic neuritis: a new clinical sign". Neurology 26 (11): 1100–4. PMID 988518.
- ^ Page NG, Bolger JP, Sanders MD (January 1982). "Auditory evoked phosphenes in optic nerve disease". J. Neurol. Neurosurg. Psychiatr. 45 (1): 7–12. doi:10.1136/jnnp.45.1.7. PMC 491258. PMID 7062073. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=491258.
- ^ Kurtzke JF (1983). "Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS)". Neurology 33 (11): 1444–52. PMID 6685237.
- ^ a b Tataru N, Vidal C, Decavel P, Berger E, Rumbach L (2006). "Limited impact of the summer heat wave in France (2003) on hospital admissions and relapses for multiple sclerosis". Neuroepidemiology 27 (1): 28–32. doi:10.1159/000094233. PMID 16804331.
- ^ Heesen C, Mohr DC, Huitinga I, et al. (March 2007). "Stress regulation in multiple sclerosis: current issues and concepts". Mult. Scler. 13 (2): 143–8. doi:10.1177/1352458506070772. PMID 17439878.
- ^ Martinelli V (2000). "Trauma, stress and multiple sclerosis". Neurol. Sci. 21 (4 Suppl 2): S849–52. doi:10.1007/s100720070024. PMID 11205361. http://link.springer-ny.com/link/service/journals/10072/bibs/00214%20Suppl%202/0021S849.htm.
- ^ Minagar A, Jy W, Jimenez JJ, Alexander JS. (April 2006). "Multiple sclerosis as a vascular disease". Neurol Res. 28 (3): 230–5. doi:10.1179/016164106X98080. PMID 16687046. http://www.shreveportphysiology.com/Alexander-MS.pdf.pdf.
- ^ Dyment DA, Ebers GC, Sadovnick AD (February 2004). "Genetics of multiple sclerosis". Lancet Neurol 3 (92): 104–10. doi:10.1016/S1474-4422(03)00663-X. PMID 14747002.
- ^ "Who gets MS?". Multiple Sclerosis Trust. December 30, 2009. http://www.mstrust.org.uk/information/publications/msexplained/who_gets_ms.jsp. Retrieved April 18, 2011.
- ^ a b c d e f g h Marrie RA (December 2004). "Environmental risk factors in multiple sclerosis aetiology". Lancet Neurol 3 (12): 709–18. doi:10.1016/S1474-4422(04)00933-0. PMID 15556803.
- ^ a b c d e Ascherio A, Munger KL (June 2007). "Environmental risk factors for multiple sclerosis. Part II: Noninfectious factors". Ann. Neurol. 61 (6): 504–13. doi:10.1002/ana.21141. PMID 17492755.
- ^ Ascherio A, Munger KL, Simon KC (June 2010). "Vitamin D and multiple sclerosis". Lancet Neurol 9 (6): 599–612. doi:10.1016/S1474-4422(10)70086-7. PMID 20494325.
- ^ Ghadirian P, Jain M, Ducic S, Shatenstein B, Morisset R (1998). "Nutritional factors in the aetiology of multiple sclerosis: a case-control study in Montreal, Canada". Int J Epidemiol. 27 (5): 845–52. doi:10.1093/ije/27.5.845. PMID 9839742. (primary source)
- ^ Spitsin S, Koprowski H (2008). "Role of uric acid in multiple sclerosis". Curr. Top. Microbiol. Immunol.. Current Topics in Microbiology and Immunology 318: 325–42. doi:10.1007/978-3-540-73677-6_13. ISBN 978-3-540-73676-9. PMID 18219824.
- ^ a b c Kurtzke JF (October 1993). "Epidemiologic evidence for multiple sclerosis as an infection". Clin. Microbiol. Rev. 6 (4): 382–427. PMC 358295. PMID 8269393. http://cmr.asm.org/cgi/pmidlookup?view=long&pmid=8269393.
- ^ Gilden DH (March 2005). "Infectious causes of multiple sclerosis". The Lancet Neurology 4 (3): 195–202. doi:10.1016/S1474-4422(05)01017-3. PMID 15721830.
- ^ a b Chari DM (2007). "Remyelination in multiple sclerosis". Int. Rev. Neurobiol.. International Review of Neurobiology 79: 589–620. doi:10.1016/S0074-7742(07)79026-8. ISBN 9780123737366. PMID 17531860.
- ^ Pittock SJ, Lucchinetti CF (March 2007). "The pathology of MS: new insights and potential clinical applications". Neurologist 13 (2): 45–56. doi:10.1097/01.nrl.0000253065.31662.37. PMID 17351524.
- ^ Iglesias A, Bauer J, Litzenburger T, Schubart A, Linington C (November 2001). "T- and B-cell responses to myelin oligodendrocyte glycoprotein in experimental autoimmune encephalomyelitis and multiple sclerosis". Glia 36 (2): 220–34. doi:10.1002/glia.1111. PMID 11596130.
- ^ Trojano M, Paolicelli D (November 2001). "The differential diagnosis of multiple sclerosis: classification and clinical features of relapsing and progressive neurological syndromes". Neurol. Sci. 22 (Suppl 2): S98–102. doi:10.1007/s100720100044. PMID 11794488. http://link.springer-ny.com/link/service/journals/10072/bibs/122%20Suppl%202000/122%20Suppl%2020S98.htm.
- ^ Poser CM, Brinar VV (June 2004). "Diagnostic criteria for multiple sclerosis: an historical review". Clin Neurol Neurosurg 106 (3): 147–58. doi:10.1016/j.clineuro.2004.02.004. PMID 15177763.
- ^ a b c d McDonald WI, Compston A, Edan G, et al. (July 2001). "Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis". Ann. Neurol. 50 (1): 121–7. doi:10.1002/ana.1032. PMID 11456302.
- ^ Polman CH, Reingold SC, Edan G, et al. (December 2005). "Diagnostic criteria for multiple sclerosis: 2005 revisions to the "McDonald Criteria"". Ann. Neurol. 58 (6): 840–6. doi:10.1002/ana.20703. PMID 16283615.
- ^ Rashid W, Miller DH (February 2008). "Recent advances in neuroimaging of multiple sclerosis". Semin Neurol 28 (1): 46–55. doi:10.1055/s-2007-1019127. PMID 18256986.
- ^ Link H, Huang YM (November 2006). "Oligoclonal bands in multiple sclerosis cerebrospinal fluid: an update on methodology and clinical usefulness". J. Neuroimmunol. 180 (1–2): 17–28. doi:10.1016/j.jneuroim.2006.07.006. PMID 16945427.
- ^ Gronseth GS, Ashman EJ (May 2000). "Practice parameter: the usefulness of evoked potentials in identifying clinically silent lesions in patients with suspected multiple sclerosis (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology 54 (9): 1720–5. PMID 10802774. http://www.neurology.org/cgi/pmidlookup?view=long&pmid=10802774.
- ^ The Royal College of Physicians (2004) (PDF). Multiple Sclerosis. National clinical guideline for diagnosis and management in primary and secondary care. Salisbury, Wiltshire: Sarum ColourView Group. pp. 54–57. ISBN 1-86016-182-0. http://www.rcplondon.ac.uk/pubs/books/MS/MSfulldocument.pdf. Retrieved on 2010-01-07.
- ^ Burton JM, O'Connor PW, Hohol M, Beyene J (2009). Burton, Jodie M. ed. "Oral versus intravenous steroids for treatment of relapses in multiple sclerosis". Cochrane Database Syst Rev (3): CD006921. doi:10.1002/14651858.CD006921.pub2. PMID 19588409.
- ^ a b c Comi G (October 2009). "Treatment of multiple sclerosis: role of natalizumab". Neurol. Sci.. 30 Suppl 2 (S2): S155–8. doi:10.1007/s10072-009-0147-2. PMID 19882365.
- ^ Johnson KP (2007). "Control of multiple sclerosis relapses with immunomodulating agents". J. Neurol. Sci. 256 (Suppl 1): S23–8. doi:10.1016/j.jns.2007.01.060. PMID 17350652.
- ^ Martinelli Boneschi F, Rovaris M, Capra R, Comi G (2005). Martinelli Boneschi, Filippo. ed. "Mitoxantrone for multiple sclerosis". Cochrane database of systematic reviews (Online) (4): CD002127. doi:10.1002/14651858.CD002127.pub2. PMID 16235298.
- ^ Leary SM, Thompson AJ (2005). "Primary progressive multiple sclerosis: current and future treatment options". CNS drugs 19 (5): 369–76. doi:10.2165/00023210-200519050-00001. PMID 15907149.
- ^ Sládková T, Kostolanský F (2006). "The role of cytokines in the immune response to influenza A virus infection". Acta Virol. 50 (3): 151–62. PMID 17131933.
- ^ Munari L, Lovati R, Boiko A (2004). Munari, Luca M.. ed. "Therapy with glatiramer acetate for multiple sclerosis". Cochrane database of systematic reviews (Online) (1): CD004678. doi:10.1002/14651858.CD004678. PMID 14974077.
- ^ Tremlett H, Oger J (November 2004). "Hepatic injury, liver monitoring and the beta-interferons for multiple sclerosis". J. Neurol. 251 (11): 1297–303. doi:10.1007/s00415-004-0619-5. PMID 15592724.
- ^ Kesselring J, Beer S (2005). "Symptomatic therapy and neurorehabilitation in multiple sclerosis". The Lancet Neurology 4 (10): 643–52. doi:10.1016/S1474-4422(05)70193-9. PMID 16168933.
- ^ Khan F, Turner-Stokes L, Ng L, Kilpatrick T (2007). Khan, Fary. ed. "Multidisciplinary rehabilitation for adults with multiple sclerosis". Cochrane Database Syst Rev (2): CD006036. doi:10.1002/14651858.CD006036.pub2. PMID 17443610.
- ^ Smith, Cath; Leigh Hale; Kärin Olson; Anthony Schneiders (2009). "How does exercise influence fatigue in people with multiple sclerosis?". Disability and Rehabilitation 31 (9): 685–692. doi:10.1080/09638280802273473. PMID 18841515.
- ^ a b c O'Sullivan, Susan (2007). Physical Rehabilitation Fifth Edition. Philadelphia: F.A. Davis Company. pp. 136–146. ISBN 978- 0-8036-1247-1.
- ^ a b c Stroud NM, Minahan CL (2009). "The impact of regular physical activity on fatigue, depression and quality of life in persons with multiple sclerosis". Health and Quality of Life Outcomes 7: 68. doi:10.1186/1477-7525-7-68. PMC 2717927. PMID 19619337. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2717927.
- ^ Rietberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G (2005). Kwakkel, Gert. ed. "Exercise therapy for multiple sclerosis". Cochrane Database of Systematic Reviews CD003980 (1): CD003980. doi:10.1002/14651858.CD003980.pub2. PMID 15674920.
- ^ a b "Multiple sclerosis: its effects on you and those you love" (pdf). Multiple Sclerosis Society of Canada. 2008. http://mssociety.ca/en/pdf/ms-effects.pdf. Retrieved 2011-05-11.
- ^ Dalgas U, Stenager E, Jakobsen J et al. (2009). "Resistance training improves muscle strength and functional capacity in multiple sclerosis". Neurology 73 (18): 1478–1484. doi:10.1212/WNL.0b013e3181bf98b4. PMID 19884575.
- ^ Olsen SA (2009). "A review of complementary and alternative medicine (CAM) by people with multiple sclerosis". Occup Ther Int 16 (1): 57–70. doi:10.1002/oti.266. PMID 19222053.
- ^ Farinotti M, Simi S, Di Pietrantonj C, et al. (2007). Farinotti, Mariangela. ed. "Dietary interventions for multiple sclerosis". Cochrane database of systematic reviews (Online) (1): CD004192. doi:10.1002/14651858.CD004192.pub2. PMID 17253500.
- ^ Chong MS, Wolff K, Wise K, Tanton C, Winstock A, Silber E (2006). "Cannabis use in patients with multiple sclerosis". Mult. Scler. 12 (5): 646–51. doi:10.1177/1352458506070947. PMID 17086912.
- ^ Bennett M, Heard R (2004). Bennett, Michael H. ed. "Hyperbaric oxygen therapy for multiple sclerosis". Cochrane database of systematic reviews (Online) (1): CD003057. doi:10.1002/14651858.CD003057.pub2. PMID 14974004.
- ^ Adams, Tim (23 May 2010). "Gut instinct: the miracle of the parasitic hookworm". The Observer. http://www.guardian.co.uk/lifeandstyle/2010/may/23/parasitic-hookworm-jasper-lawrence-tim-adams.
- ^ a b c Phadke JG (May 1987). "Survival pattern and cause of death in patients with multiple sclerosis: results from an epidemiological survey in north east Scotland". J. Neurol. Neurosurg. Psychiatr. 50 (5): 523–31. doi:10.1136/jnnp.50.5.523. PMC 1031962. PMID 3495637. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1031962.
- ^ Myhr KM, Riise T, Vedeler C, et al (February 2001). "Disability and prognosis in multiple sclerosis: demographic and clinical variables important for the ability to walk and awarding of disability pension". Mult. Scler. 7 (1): 59–65. PMID 11321195. http://msj.sagepub.com/cgi/pmidlookup?view=long&pmid=11321195.
- ^ a b c Alonso A, Hernán MA (July 2008). "Temporal trends in the incidence of multiple sclerosis: a systematic review". Neurology 71 (2): 129–35. doi:10.1212/01.wnl.0000316802.35974.34. PMID 18606967.
- ^ Pugliatti, M; Sotgiu, S, Rosati, G (2002 Jul). "The worldwide prevalence of multiple sclerosis". Clinical neurology and neurosurgery 104 (3): 182–91. doi:10.1016/S0303-8467(02)00036-7. PMID 12127652.
- ^ Kulie T, Groff A, Redmer J, Hounshell J, Schrager S (2009). "Vitamin D: an evidence-based review". J Am Board Fam Med 22 (6): 698–706. doi:10.3122/jabfm.2009.06.090037. PMID 19897699.
- ^ a b Compston A (October 1988). "The 150th anniversary of the first depiction of the lesions of multiple sclerosis". J. Neurol. Neurosurg. Psychiatr. 51 (10): 1249–52. doi:10.1136/jnnp.51.10.1249. PMC 1032909. PMID 3066846. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1032909.
- ^ Lassmann H (1999-10-29). "The pathology of multiple sclerosis and its evolution". Philos Trans R Soc Lond B Biol Sci. 354 (1390): 1635–40. doi:10.1098/rstb.1999.0508. PMC 1692680. PMID 10603616. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1692680.
- ^ Lassmann H (July 2005). "Multiple sclerosis pathology: evolution of pathogenetic concepts". Brain Pathology 15 (3): 217–22. doi:10.1111/j.1750-3639.2005.tb00523.x. PMID 16196388.
- ^ Medaer R (September 1979). "Does the history of multiple sclerosis go back as far as the 14th century?". Acta Neurol. Scand. 60 (3): 189–92. doi:10.1111/j.1600-0447.1979.tb08970.x. PMID 390966.
- ^ Holmøy T (2006). "A Norse contribution to the history of neurological diseases". Eur. Neurol. 55 (1): 57–8. doi:10.1159/000091431. PMID 16479124.
- ^ Firth, D (1948). The Case of August D`Esté. Cambridge: Cambridge University Press.
- ^ a b Pearce JM (2005). "Historical descriptions of multiple sclerosis". Eur. Neurol. 54 (1): 49–53. doi:10.1159/000087387. PMID 16103678.
- ^ Barbellion, Wilhelm Nero Pilate (1919). The Journal of a Disappointed Man. New York: George H. Doran. ISBN 0-7012-1906-8.
- ^ a b Cohen JA (July 2009). "Emerging therapies for relapsing multiple sclerosis". Arch. Neurol. 66 (7): 821–8. doi:10.1001/archneurol.2009.104. PMID 19597083.
- ^ DeNoon, Daniel J. (2010). "FDA Panel Votes to Approve Gilenia, First Oral MS Drug". WebMD. http://www.webmd.com/multiple-sclerosis/news/20100610/fda-panel-votes-to-approve-gilenia-first-oral-ms-drug. Retrieved 2010-06-13.
- ^ FDA press release on approval of Gilenya
- ^ Kappos L; Radue, EW; O'Connor, P; Polman, C; Hohlfeld, R; Calabresi, P; Selmaj, K; Agoropoulou, C et al. (February 2010). "A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis". N Eng J Med 362 (5): 387–401. doi:10.1056/NEJMoa0909494. PMID 20089952.
- ^ Cohen JA; Barkhof, F; Comi, G; Hartung, HP; Khatri, BO; Montalban, X; Pelletier, J; Capra, R et al. (February 2010). "Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis". N Eng J Med 362 (5): 402–415. doi:10.1056/NEJMoa0907839. PMID 20089954.
- ^ Patel PN (September 2007). "Low-dose naltrexone for treatment of multiple sclerosis: clinical trials are needed". Ann Pharmacother 41 (9): 1549–50. doi:10.1345/aph.1H083. PMID 17623758.
- ^ Gironi M, Martinelli-Boneschi F, Sacerdote P, Solaro C, Zaffaroni M, Cavarretta R, Moiola L, Bucello S, Radaelli M, Pilato V, Rodegher M, Cursi M, Franchi S, Martinelli V, Nemni R, Comi G, Martino G (2008). "A pilot trial of low-dose naltrexone in primary progressive multiple sclerosis". Multiple Sclerosis 14 (8): 1076–83. doi:10.1177/1352458508095828. PMID 18728058.
- ^ a b c d Harris VK, Sadiq SA (2009). "Disease biomarkers in multiple sclerosis: potential for use in therapeutic decision making". Mol Diagn Ther 13 (4): 225–44. doi:10.2165/11313470-000000000-00000. PMID 19712003.
- ^ Zamboni P, Galeotti R, Menegatti E, et al. (April 2009). "Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis". J. Neurol. Neurosurg. Psychiatr. 80 (4): 392–9. doi:10.1136/jnnp.2008.157164. PMC 2647682. PMID 19060024. http://jnnp.bmj.com/cgi/content/full/80/4/392.
- ^ Qiu J (May 2010). "Venous abnormalities and multiple sclerosis: another breakthrough claim?". Lancet Neurol 9 (5): 464–5. doi:10.1016/S1474-4422(10)70098-3. PMID 20398855.
- ^ Ghezzi A, Comi G, Federico A (February 2011). "Chronic cerebro-spinal venous insufficiency (CCSVI) and multiple sclerosis". Neurol. Sci. 32 (1): 17–21. doi:10.1007/s10072-010-0458-3. PMID 21161309.
- ^ Dorne H, Zaidat OO, Fiorella D, Hirsch J, Prestigiacomo C, Albuquerque F, Tarr RW. (October 2010). "Chronic cerebrospinal venous insufficiency and the doubtful promise of an endovascular treatment for multiple sclerosis". J NeuroIntervent Surg 2 (4): 309–311. doi:10.1136/jnis.2010.003947.
- ^ Khan O, Filippi M, Freedman MS, Barkhof F, Dore-Duffy P, Lassmann H, Trapp B, Bar-Or A, Zak I, Siegel MJ, Lisak R (2010-02-12). "Chronic cerebrospinal venous insufficiency and multiple sclerosis". Annals of neurology (Annals of Neurology) 67 (3): 286–90. doi:10.1002/ana.22001. PMID 20373339.
Further reading
- Langgartner M, Langgartner I, Drlicek M (April 2005). "The patient's journey: multiple sclerosis". BMJ 330 (7496): 885–8. doi:10.1136/bmj.330.7496.885. PMC 556161. PMID 15831874. http://bmj.bmjjournals.com/cgi/content/full/330/7496/885.
External links
- Multiple sclerosis at the Open Directory Project
- Database for analysis and comparison of global data on the epidemiology of MS
- NIH listing of clinical trials related to MS
- Abstract index of the Cochrane Library
Multiple sclerosis and other demyelinating diseases of CNS (G35–G37, 340–341) Signs and symptoms Ataxia · Depression · Diplopia · Dysarthria · Dysphagia · Fatigue · Incontinence · Neurological fatigue · Nystagmus · Optic neuritis · Pain · Uhthoff's phenomenon · Dawson's fingersDiagnosis and evolution following Investigation Treatment Borderline forms Acute disseminated encephalomyelitis · Balo concentric sclerosis · Neuromyelitis optica · Marburg multiple sclerosis · Schilder's disease · Tumefactive multiple sclerosis
(Guillain-Barré syndrome and CIDP are PNS)Other Immune disorders: hypersensitivity and autoimmune diseases (279.5–6) Type I/allergy/atopy
(IgE)ForeignAtopic dermatitis · Allergic urticaria · Hay fever · Allergic asthma · Anaphylaxis · Food allergy (Milk, Egg, Peanut, Tree nut, Seafood, Soy, Wheat), Penicillin allergyAutoimmunenoneType II/ADCC
(IgM, IgG)ForeignAutoimmuneAutoimmune hemolytic anemia · Idiopathic thrombocytopenic purpura · Bullous pemphigoid · Pemphigus vulgaris · Rheumatic fever · Goodpasture's syndromeType III
(Immune complex)ForeignHenoch–Schönlein purpura · Hypersensitivity vasculitis · Reactive arthritis · Rheumatoid arthritis · Farmer's lung · Post-streptococcal glomerulonephritis · Serum sickness · Arthus reactionAutoimmuneType IV/cell-mediated
(T-cells)ForeignAutoimmuneDiabetes mellitus type 1 · Hashimoto's thyroiditis · Guillain–Barré syndrome · Multiple sclerosis · Coeliac disease · Giant-cell arteritisUnknown/
multipleForeignAutoimmuneSjögren's syndrome · Autoimmune hepatitis · Autoimmune polyendocrine syndrome (APS1, APS2) · Autoimmune adrenalitis · Systemic autoimmune diseaseCategories:
Wikimedia Foundation. 2010.