- Dawson's fingers
-
"Dawson's Fingers" is the name for the multiple sclerosis lesions around the ventricle-based brain veins[1][2] of Multiple Sclerosis patients. The condition is supposed to be the result of inflammation or mechanical damage by blood pressure[3]around long axis of medular veins.
Dawson's fingers spread along, and from, large periventricular collecting veins, and are attributed to perivenular inflammation[4]. Lesions far away from these veins are known as Steiner's splashes[3].
Contents
Distribution
Using high field MRI system, with several variants several areas show lesions, and can be spacially classified in infratentorial, callosal, juxtacortical, periventricular, and other white matter areas[5]. Other authors simplify this in three regions: intracortical, mixed gray-white matter, and juxtacortical[6]. Others classify them as hippocampal, cortical, and WM lesions[7], and finally, others give seven areas: intracortical, mixed white matter-gray matter, juxtacortical, deep gray matter, periventricular white matter, deep white matter, and infratentorial lesions[8]. The distribution of the lesions could be linked to the clinical evolution[9]
Post-mortem authopsy reveal that gray matter demyelination occurs in the motor cortex, cingulate gyrus, cerebellum, thalamus and spinal cord[10]. Cortical lesions have been observed specially in people with SPMS but they also appear in RRMS and clinically isolated syndrome. They are more frequent in men than in women[11] and they can partly explain cognitive deficits.
It is known that two parameters of the cortical lesions, fractional anisotropy (FA) and mean diffusivity (MD), are higher in patients than in controls[12]. They are larger in SPMS than in RRMS and most of them remain unchanged for short follow-up periods. They do not spread into the subcortical white matter and never show gadolinium enhancement. Over a one-year period, CLs can increase their number and size in a relevant proportion of MS patients, without spreading into the subcortical white matter or showing inflammatory features similar to those of white matter lesions.[13]
The first plausible explanation of their distribution was published by Dr. Schelling. He said:
- The specific brain plaques of multiple sclerosis can only be caused by energetic venous back-jets set in motion by intermittent rises in the pressure in the large collecting veins of the neck, but especially of the chest.[3].
But no problems with chest veins was ever found.
Recently, it has been remarked that it can plausibly be accounted for by veno-venous reflux[14][15], according to the CCSVI theory. This results in a finger-like appearance of the lesions extending mainly off the ventricles within the brain.
This morphologic appearance was named Dawson's fingers by Charles Lumsden, after the Scottish pathologist James Walker Dawson [16], who first defined the condition in 1916.
Demyelination process
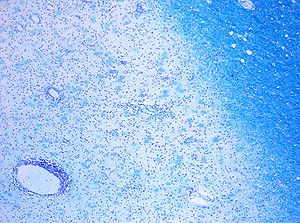
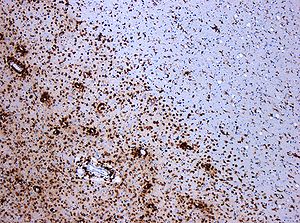 Demyelinization by MS. The CD68 colored tissue shows several Macrophages in the area of the lesion. Original scale 1:100
Demyelinization by MS. The CD68 colored tissue shows several Macrophages in the area of the lesion. Original scale 1:100
Demyelination begins with the blood-brain barrier breakdown. It is a tight vascular barrier between the blood and brain that should prevent the passage of antibodies through it, but in MS patients it does not work. For unknown reasons special areas appear in the brain and spine, followed by leaks in the blood-brain barrier where immune cells infiltrate.
According to the view of most researchers, a special subset of lymphocytes, called T helper cells, specifically Th1 and Th17[17], play a key role in the development of the lesion. Under normal circumstances, these lymphocytes can distinguish between self and non-self. However, in a person with MS, these cells recognize healthy parts of the central nervous system as foreign and attack them as if they were an invading virus, triggering inflammatory processes and stimulating other immune cells and soluble factors like cytokines and antibodies. Many of the myelin-recognizing T cells belong to a terminally differentiated subset called co-stimulation-independent effector-memory T cells[18][19][20][21][22][23][24][25][26][27][28]. Recently other type of immune cells, B Cells, have been also implicated in the pathogenesis of MS[29] and in the degeneration of the axons[30].
The axons themselves can also be damaged by the attacks.[31] Often, the brain is able to compensate for some of this damage, due to an ability called neuroplasticity. MS symptoms develop as the cumulative result of multiple lesions in the brain and spinal cord. This is why symptoms can vary greatly between different individuals, depending on where their lesions occur.
Repair processes, called remyelination, also play an important role in MS. Remyelination is one of the reasons why, especially in early phases of the disease, symptoms tend to decrease or disappear temporarily. Nevertheless, nerve damage and irreversible loss of neurons occur early in MS.
The oligodendrocytes that originally formed a myelin sheath cannot completely rebuild a destroyed myelin sheath. However, the central nervous system can recruit oligodendrocyte stem cells capable of proliferation and migration and differentiation into mature myelinating oligodendrocytes. The newly-formed myelin sheaths are thinner and often not as effective as the original ones. Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons. Under laboratory conditions, stem cells are quite capable of proliferating and differentiating into remyelinating oligodendrocytes; it is therefore suspected that inflammatory conditions or axonal damage somehow inhibit stem cell proliferation and differentiation in affected areas[32]
See also
External links
- Dawson Fingers in Multiple Sclerosis [7]
Sources
- ^ Peter Reimer,Paul M. Parizel,Falko-Alexander Stichnoth. Clinical MR imaging: a practical approach.[1]
- ^ Dawson fingers, at Radiopedia [2]
- ^ a b c Schelling F. MS: The image and its message [3]
- ^ Suzanne Palmer, William G. Bradley, Dar-Yeong Chen, Sangita Patel, Subcallosal Striations: Early Findings of Multiple Sclerosis on Sagittal, Thin-Section, Fast FLAIR MR Images[4]
- ^ Wattjes MP, Harzheim M, Kuhl CK, et al. (1 September 2006). "Does high-field MR imaging have an influence on the classification of patients with clinically isolated syndromes according to current diagnostic mr imaging criteria for multiple sclerosis?". AJNR Am J Neuroradiol. 27 (8): 1794–8. PMID 16971638. http://www.ajnr.org/cgi/pmidlookup?view=long&pmid=16971638.
- ^ Nelson F, Poonawalla AH, Hou P, Huang F, Wolinsky JS, Narayana PA (October 2007). "Improved identification of intracortical lesions in multiple sclerosis with phase-sensitive inversion recovery in combination with fast double inversion recovery MR imaging". AJNR Am J Neuroradiol. 28 (9): 1645–9. doi:10.3174/ajnr.A0645. PMID 17885241.
- ^ Roosendaal SD, Moraal B, Vrenken H, et al. (April 2008). "In vivo MR imaging of hippocampal lesions in multiple sclerosis". J Magn Reson Imaging. 27 (4): 726–31. doi:10.1002/jmri.21294. PMID 18302199.
- ^ Geurts JJ, Pouwels PJ, Uitdehaag BM, Polman CH, Barkhof F, Castelijns JA (July 2005). "Intracortical lesions in multiple sclerosis: improved detection with 3D double inversion-recovery MR imaging". Radiology 236 (1): 254–60. doi:10.1148/radiol.2361040450. PMID 15987979.
- ^ Sampat MP, Berger AM, Healy BC, et al. (October 2009). "Regional white matter atrophy--based classification of multiple sclerosis in cross-sectional and longitudinal data". AJNR Am J Neuroradiol 30 (9): 1731–9. doi:10.3174/ajnr.A1659. PMC 2821733. PMID 19696139. http://www.ajnr.org/cgi/pmidlookup?view=long&pmid=19696139.
- ^ Gilmore CP, Donaldson I, Bö L, Owens T, Lowe JS, Evangelou N (October 2008). "Regional variations in the extent and pattern of grey matter demyelination in Multiple Sclerosis: a comparison between the cerebral cortex, cerebellar cortex, deep grey matter nuclei and the spinal cord". J Neurol Neurosurg Psychiatry. 80 (2): 182–7. doi:10.1136/jnnp.2008.148767. PMID 18829630.
- ^ Calabrese M, De Stefano N, Atzori M, et al. (2007). "Detection of cortical inflammatory lesions by double inversion recovery magnetic resonance imaging in patients with multiple sclerosis". Arch. Neurol. 64 (10): 1416–22. doi:10.1001/archneur.64.10.1416. PMID 17923625.
- ^ Poonawalla AH, Hasan KM, Gupta RK, et al. (2008). "Diffusion-Tensor MR Imaging of Cortical Lesions in Multiple Sclerosis: Initial Findings". Radiology 246 (3): 880. doi:10.1148/radiol.2463070486. PMID 18195384.
- ^ Calabrese M, Filippi M, Rovaris M, Mattisi I, Bernardi V, Atzori M, Favaretto A, Barachino L, Rinaldi L, Romualdi C, Perini P, Gallo P. (2008). "Morphology and evolution of cortical lesions in multiple sclerosis. A longitudinal MRI study". NeuroImage 42 (4): 1324–8. doi:10.1016/j.neuroimage.2008.06.028. PMID 18652903.
- ^ Schelling F (October 1986). "Damaging venous reflux into the skull or spine: relevance to multiple sclerosis". Med. Hypotheses 21 (2): 141–8. doi:10.1016/0306-9877(86)90003-4. PMID 3641027.
- ^ list of CCSVI publications [5][6]
- ^ Dawson, J.W.: The histology of disseminated sclerosis. Trans Roy Soc Edinb, 50: 517, 1916.
- ^ Fransson ME, Liljenfeldt LS, Fagius J, Tötterman TH, Loskog AS. (2009). "The T-cell pool is anergized in patients with multiple sclerosis in remission". Immunology 126 (1): 92–101. doi:10.1111/j.1365-2567.2008.02881.x. PMC 2632699. PMID 18624727. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2632699.
- ^ Markovic-Plese S, Cortese I, Wandinger KP, McFarland HF, Martin R (October 2001). "CD4+CD28- costimulation-independent T cells in multiple sclerosis". J. Clin. Invest. 108 (8): 1185–94. doi:10.1172/JCI12516. PMC 209525. PMID 11602626. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=209525.
- ^ Wulff H, Calabresi PA, Allie R, et al. (June 2003). "The voltage-gated Kv1.3 K(+) channel in effector memory T cells as new target for MS". J. Clin. Invest. 111 (11): 1703–13. doi:10.1172/JCI16921. PMC 156104. PMID 12782673. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=156104.
- ^ Rus H, Pardo CA, Hu L, et al. (August 2005). "The voltage-gated potassium channel Kv1.3 is highly expressed on inflammatory infiltrates in multiple sclerosis brain". Proc. Natl. Acad. Sci. U.S.A. 102 (31): 11094–9. doi:10.1073/pnas.0501770102. PMC 1182417. PMID 16043714. http://www.pnas.org/cgi/pmidlookup?view=long&pmid=16043714.
- ^ Beeton C, Chandy KG (December 2005). "Potassium channels, memory T cells, and multiple sclerosis". Neuroscientist 11 (6): 550–62. doi:10.1177/1073858405278016. PMID 16282596. http://nro.sagepub.com/cgi/pmidlookup?view=long&pmid=16282596.
- ^ Okuda Y, Okuda M, Apatoff BR, Posnett DN (August 2005). "The activation of memory CD4(+) T cells and CD8(+) T cells in patients with multiple sclerosis". J. Neurol. Sci. 235 (1-2): 11–7. doi:10.1016/j.jns.2005.02.013. PMID 15972217. http://linkinghub.elsevier.com/retrieve/pii/S0022-510X(05)00108-5.
- ^ Krakauer M, Sorensen PS, Sellebjerg F (December 2006). "CD4(+) memory T cells with high CD26 surface expression are enriched for Th1 markers and correlate with clinical severity of multiple sclerosis". J. Neuroimmunol. 181 (1-2): 157–64. doi:10.1016/j.jneuroim.2006.09.006. PMID 17081623. http://linkinghub.elsevier.com/retrieve/pii/S0165-5728(06)00372-9.
- ^ Ratts RB, Karandikar NJ, Hussain RZ, et al. (September 2006). "Phenotypic characterization of autoreactive T cells in multiple sclerosis". J. Neuroimmunol. 178 (1-2): 100–10. doi:10.1016/j.jneuroim.2006.06.010. PMID 16901549. http://linkinghub.elsevier.com/retrieve/pii/S0165-5728(06)00226-8.
- ^ Haegele KF, Stueckle CA, Malin JP, Sindern E (February 2007). "Increase of CD8+ T-effector memory cells in peripheral blood of patients with relapsing-remitting multiple sclerosis compared to healthy controls". J. Neuroimmunol. 183 (1-2): 168–74. doi:10.1016/j.jneuroim.2006.09.008. PMID 17084910. http://linkinghub.elsevier.com/retrieve/pii/S0165-5728(06)00376-6.
- ^ Jilek S, Schluep M, Rossetti AO, et al. (April 2007). "CSF enrichment of highly differentiated CD8+ T cells in early multiple sclerosis". Clin. Immunol. 123 (1): 105–13. doi:10.1016/j.clim.2006.11.004. PMID 17188575. http://linkinghub.elsevier.com/retrieve/pii/S1521-6616(06)00946-6.
- ^ Miyazaki Y, Iwabuchi K, Kikuchi S, et al. (September 2008). "Expansion of CD4+CD28- T cells producing high levels of interferon-{gamma} in peripheral blood of patients with multiple sclerosis". Mult. Scler. 14 (8): 1044–55. doi:10.1177/1352458508092809. PMID 18573819. http://msj.sagepub.com/cgi/pmidlookup?view=long&pmid=18573819.
- ^ Lünemann JD, Jelcić I, Roberts S, et al. (August 2008). "EBNA1-specific T cells from patients with multiple sclerosis cross react with myelin antigens and co-produce IFN-gamma and IL-2". J. Exp. Med. 205 (8): 1763–73. doi:10.1084/jem.20072397. PMC 2525578. PMID 18663124. http://www.jem.org/cgi/pmidlookup?view=long&pmid=18663124.
- ^ Hauser SL, Waubant E, Arnold DL, et al. (February 2008). "B-cell depletion with rituximab in relapsing-remitting multiple sclerosis". N Engl J Med. 358 (7): 676–88. doi:10.1056/NEJMoa0706383. PMID 18272891.
- ^ Cause of nerve fiber damage in multiple sclerosis identified
- ^ Pascual AM, Martínez-Bisbal MC, Boscá I, et al. (2007). "Axonal loss is progressive and partly dissociated from lesion load in early multiple sclerosis". Neurology 69 (1): 63–7. doi:10.1212/01.wnl.0000265054.08610.12. PMID 17606882.
- ^ Wolswijk G (15 January 1998). "Chronic stage multiple sclerosis lesions contain a relatively quiescent population of oligodendrocyte precursor cells". J Neurosci. 18 (2): 601–9. PMID 9425002. http://www.jneurosci.org/cgi/pmidlookup?view=long&pmid=9425002.
Eponymous medical signs · nervous system CNS Head, generalBattle's sign · Broca aphasia · Kernig's sign · Macewen's sign · Myerson's sign · Stroop test · Wada test · Dix-Hallpike test · Hirano bodyOtherPNS CombinationLower limbUpper limbOther torso/limbsUpper limbLower limbAbadie's sign of tabes dorsalis · Gowers' sign · Hoover's sign · Lasègue's sign · Trendelenburg's signTorsoGeneralTodd's paresis · Jolly's testMental/behavioral Multiple sclerosis and other demyelinating diseases of CNS (G35–G37, 340–341) Signs and symptoms Ataxia · Depression · Diplopia · Dysarthria · Dysphagia · Fatigue · Incontinence · Neurological fatigue · Nystagmus · Optic neuritis · Pain · Uhthoff's phenomenon · Dawson's fingersDiagnosis and evolution following Investigation Treatment Borderline forms Acute disseminated encephalomyelitis · Balo concentric sclerosis · Neuromyelitis optica · Marburg multiple sclerosis · Schilder's disease · Tumefactive multiple sclerosis
(Guillain-Barré syndrome and CIDP are PNS)Other Categories:- Symptoms and signs: Nervous system
- Multiple sclerosis
Wikimedia Foundation. 2010.