- Central pontine myelinolysis
-
Central pontine myelinolysis Classification and external resources 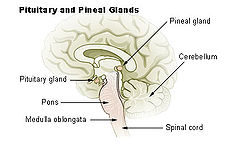
Pons labeled at bottom leftICD-10 G37.2 DiseasesDB 2198 MedlinePlus 000775 eMedicine neuro/50 MeSH D017590 Central pontine myelinolysis is neurological disease caused by severe damage of the myelin sheath of nerve cells in the brainstem, more precisely in the area termed the pons, predominately of iatrogenic etiology. It is characterized by acute paralysis, dysphagia (difficulty swallowing), and dysarthria (difficulty speaking), and other neurological symptoms.
It can also occur outside the pons.[1] The term "osmotic demyelination syndrome" is similar to "central pontine myelinolysis", but also includes areas outside the pons.[2]
Central pontine myelinolysis is a complication of treatment of patients with profound, life-threatening hyponatremia (low sodium). It occurs as a consequence of a rapid rise in serum tonicity following treatment in individuals with chronic, severe hyponatraemia who have made intracellular adaptations to the prevailing hypotonicity. Hyponatremia should be corrected at a rate of no more than 8-10 mmol/L of sodium per day to prevent central pontine myelinolysis.
Contents
Pathophysiology
The currently accepted theory states that the brain cells adjust their osmolarities by changing levels of certain osmolytes like inositol, betaine, and glutamine. In hyponatremia the levels of these osmolytes fall, preventing entry of free-water into cells. The reverse is true for hypernatremia. So rapid correction of sodium in hyponatremia would cause the extracellular fluid to be relatively hypertonic. Free water would then move out of the cells. This leads to a central pontine myelinolysis, manifesting as the paralysis.
The demyelination of the axons (nerve fibers in the brain) damages them.[3]
In the context of chronic low plasma sodium, the brain's cells (neurons and glia) adapt by taking in a small amount of water; the net effect is to move water out of the interstitium and equilibrate (or nearly so) the intracellular and extracellular tonicities. The chronic hyponatremia is thus compensated.
With correction of the hyponatremia with intravenous fluids, the intra- and extra-cellular tonicities are again changed, this time in the opposite direction. With the use of intravenous hypertonic saline, the correction can be too quick, not allowing enough time for the brain's cells to adjust to the new tonicity. With a rise in extracellular tonicity, the cells compensate by losing a small amount of water. This loss will continue until the intra- and extra-cellular tonicities are equal. If hypertonic therapy continues or is too rapid, the extracellular tonicity will continue to drive water out of the brain's cells, leading to cellular dysfunction and the condition of central pontine myelinolysis.
Rapid correction of hypernatremia causes water to move into cells, leading to multiple cerebral hemorrhages, equally catastrophic as osmotic demyelination.
Causes
The most common cause is the rapid correction of low blood sodium levels (hyponatremia).[4]
It has been observed following hematopoietic stem cell transplantation.[5]
patients can be affected by:
- underlying severe liver disease
- liver transplant patients
- severe burns
- malnutrition
- anorexia
- severe electrolyte disorders
- AIDS
It can be associated with hyperemesis gravidarum.[6]
Diagnosis
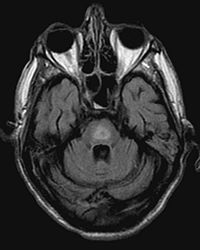
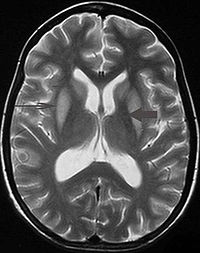
It can be difficult to identify using conventional imaging techniques. Imaging by MRI demonstrates an area of high signal return on T2 weighted images.
Symptoms
Frequently observed symptoms in this disorder are acute para- or quadraparesis, dysphagia, dysarthria, diplopia, loss of consciousness, and other neurological symptoms associated with brainstem damage. The patient may experience locked-in syndrome where cognitive function is intact, but all muscles are paralyzed with the exception of eye blinking. These result from a rapid myelinolysis of the corticobulbar and corticospinal tracts in the brainstem.
Prevention and treatment
To prevent CPM via the most common cause, overly rapid correction of hyponatremia, the hyponatremia should be corrected at a rate not in excess of 10 mmol/L/24hr or 0.5 mEq/L/Hr; thus diligently avoiding hypernatremia. Details concerning the etiology and correction of electrolyte disorders are discussed extensively in general medicine texts. Alcoholic patients should receive vitamin supplementation and a formal evaluation of their nutritional status.[7][8]
Once demyelination has begun, there is no specific treatment. Care is supportive, with the goal of preventing complications like aspiration pneumonia or deep vein thrombosis. Alcoholics are usually given vitamins to correct for other deficiencies.
Research has led to improved outcomes.[9] Animal studies suggest inositol reduces the severity of osmotic demyelination syndrome if given prior to rapid correction of chronic hyponatraemia.[10] Further study is required prior to its application in humans for this indication.
Prognosis
The prognosis is overall poor. While some patients die, most survive and of the survivors, approximately one-third recover; one-third are disabled but are able to live independently; one-third are severely disabled.[11] Permanent disabilities range from minor tremors and ataxia to signs of severe brain damage, such as spastic quadriparesis and locked-in syndrome.[12] Some improvements may be seen over the course of the first several months after the condition stabilizes.
The extent of recovery depends on how many axons were damaged.[3]
References
- ^ Gocht A, Colmant HJ (1987). "Central pontine and extrapontine myelinolysis: a report of 58 cases". Clin. Neuropathol. 6 (6): 262–70. PMID 3322623.
- ^ Lampl C, Yazdi K (2002). "Central pontine myelinolysis". Eur. Neurol. 47 (1): 3–10. doi:10.1159/000047939. PMID 11803185. Archived from the original on 2010-11-18. http://content.karger.com/produktedb/produkte.asp?typ=fulltext&file=ene47003.
- ^ a b Medana IM, Esiri MM (March 2003). "Axonal damage: a key predictor of outcome in human CNS diseases". Brain 126 (Pt 3): 515–30. doi:10.1093/brain/awg061. PMID 12566274. http://brain.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12566274.
- ^ Bernsen HJ, Prick MJ (September 1999). "Improvement of central pontine myelinolysis as demonstrated by repeated magnetic resonance imaging in a patient without evidence of hyponatremia". Acta Neurol Belg 99 (3): 189–93. PMID 10544728.
- ^ Lim KH, Kim S, Lee YS, et al. (April 2008). "Central pontine myelinolysis in a patient with acute lymphoblastic leukemia after hematopoietic stem cell transplantation: a case report". J. Korean Med. Sci. 23 (2): 324–7. doi:10.3346/jkms.2008.23.2.324. PMC 2526450. PMID 18437020. http://jkms.org/contents/jkms.php?pubyear=2008&vol=23&fpage=324.[dead link]
- ^ Central pontine myelinolysis induced by hyperemesis gravidarum
- ^ Kleinschmidt-DeMasters BK, Norenberg MD. Rapid correction of hyponatremia causes demyelination: relation to central pontine myelinolysis. Science. 1981;211(4486):1068-70. PMID 7466381
- ^ Laureno R. Experimental pontine and extrapontine myelinolysis. Trans Am Neurol Assoc. 1980;105:354-8. PMID 7348981
- ^ Brown WD (December 2000). "Osmotic demyelination disorders: central pontine and extrapontine myelinolysis". Curr. Opin. Neurol. 13 (6): 691–7. doi:10.1097/00019052-200012000-00014. PMID 11148672. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1350-7540&volume=13&issue=6&spage=691.
- ^ Silver SM, Schroeder BM, Sterns RH, Rojiani AM (2006). "Myoinositol administration improves survival and reduces myelinolysis after rapid correction of chronic hyponatremia in rats". J Neuropathol Exp Neurol 65 (1): 37–44. doi:10.1097/01.jnen.0000195938.02292.39. PMID 16410747.
- ^ Abbott R, Silber E, Felber J, Ekpo E (October 2005). "Osmotic demyelination syndrome". BMJ 331 (7520): 829–30. doi:10.1136/bmj.331.7520.829. PMC 1246086. PMID 16210283. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1246086.
- ^ http://www.emedicine.com/NEURO/topic50.htm
External links
- MedPix Images of Osmotic Myelinolysis
Categories:- Demyelinating diseases of CNS
- Electrolyte disturbances
Wikimedia Foundation. 2010.