- Syringomyelia
-
Syringomyelia Classification and external resources 
An idiopathic syrinx. See the thin light grey shape inside the spinal cord, placed at centre in the bottom half of the above image.ICD-10 G95.0, Q06.4 ICD-9 336.0 742.53 OMIM 272480 186700 DiseasesDB 12769 MedlinePlus 001398 eMedicine neuro/359 MeSH D013595 Syringomyelia (
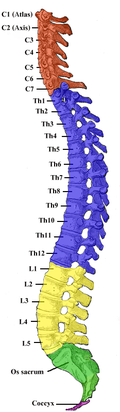
 /sɪˌrɪŋɡɵmaɪˈiːliə/) is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in pain, paralysis, weakness,[1] and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. The disorder generally leads to a cape-like loss of pain and temperature sensation along the back and arms. Each patient experiences a different combination of symptoms. These symptoms typically vary depending on the extent and, often more critically, to the location of the syrinx within the spinal cord.
/sɪˌrɪŋɡɵmaɪˈiːliə/) is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in pain, paralysis, weakness,[1] and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. The disorder generally leads to a cape-like loss of pain and temperature sensation along the back and arms. Each patient experiences a different combination of symptoms. These symptoms typically vary depending on the extent and, often more critically, to the location of the syrinx within the spinal cord.Syringomyelia has a prevalence estimated at 8.4 cases per 100,000 people,[2] with symptoms usually beginning in young adulthood. Signs of the disorder tend to develop slowly, although sudden onset may occur with coughing, straining, or myelopathy.
Contents
Pathogenesis
Cerebrospinal fluid normally flows in a pulsatile manner throughout the subarachnoid space which envelops the spinal cord and brain, transporting nutrients and waste products. The cerebrospinal fluid also serves to cushion the brain. Excess cerebrospinal fluid in the central canal of the spinal cord is called hydromyelia. This term refers to increased cerebrospinal fluid that is contained within the ependyma of the central canal. When fluid dissects into the surrounding white matter forming a cystic cavity or syrinx, the term syringomyelia is applied. As these conditions coexist in the majority of cases, the term syringohydromyelia is applied. However, most physicians use the terms interchangeably.
The pulsatile movement of the cerebrospinal fluid within the subarachnoid space is a result of the phase difference in influx and outflow of blood within the cranial vault. The total fluid pulsation per cardiac cycle is approximately 1 cc in a healthy adult. Since the brain is contained within the nearly rigid cranial cavity, the cerebrospinal fluid pulsation moves into the more compliant spinal canal having nearly zero net flow during each cardiac cycle.
It has been observed that obstruction of the cerebrospinal fluid pulsation in the subarachnoid space can result in syrinx formation. A number of pathological conditions can cause an obstruction of the normal cerebrospinal fluid pulsation. These include Chiari malformation, spinal arachnoiditis, scoliosis, spinal vertebrae misalignment, spinal tumors, spina bifida, and others. The reasons that blockage of the cerebrospinal fluid pulsation within the subarachnoid space can result in syrinx formation are not known. Moreover, it is unclear if syrinx fluid originates from bulk movement of cerebrospinal fluid into the spinal cord, from bulk transmural movement of blood fluids through the spinal vasculature into the syrinx, or from a combination of both. Once a syrinx has formed, pressure differences along the spine have been proposed to be one mechanism causing fluid movement within the cyst, possibly resulting in damage to the spinal cord.
Different Origins
Generally, there are two forms of syringomyelia: congenital and acquired. (In addition, one form of the disorder involves a part of the brain called the brainstem. The brainstem controls many of our vital functions, such as respiration and heartbeat. When syrinxes affect the brainstem, the condition is called syringobulbia.)
Congenital
The first major form relates to an abnormality of the brain called an Arnold-Chiari malformation. This is the most common cause of syringomyelia, where the anatomic abnormality causes the lower part of the cerebellum to protrude from its normal location in the back of the head into the cervical or neck portion of the spinal canal. A syrinx may then develop in the cervical region of the spinal cord. Because of the relationship that was once thought to exist between the brain and spinal cord in this type of syringomyelia, physicians sometimes refer to it as communicating syringomyelia. Here, symptoms usually begin between the ages of 25 and 40 and may worsen with straining or any activity that causes cerebrospinal fluid pressure to fluctuate suddenly. Some patients, however, may have long periods of stability. Some patients with this form of the disorder also have hydrocephalus, in which cerebrospinal fluid accumulates in the skull, or a condition called arachnoiditis, in which a covering of the spinal cord—the arachnoid membrane—is inflamed.
Some cases of syringomyelia are familial, although this is rare.
Acquired
The second major form of syringomyelia occurs as a complication of trauma, meningitis, hemorrhage, a tumor, or arachnoiditis. Here, the syrinx or cyst develops in a segment of the spinal cord damaged by one of these conditions. The syrinx then starts to expand. This is sometimes referred to as noncommunicating syringomyelia. Symptoms may appear months or even years after the initial injury, starting with pain, weakness, and sensory impairment originating at the site of trauma.
The primary symptom of post-traumatic syringomyelia (often referred to using the abbreviation of PTS)[3] is pain, which may spread upward from the site of injury. Symptoms, such as pain, numbness, weakness, and disruption in temperature sensation, may be limited to one side of the body. Syringomyelia can also adversely affect sweating, sexual function, and, later, bladder and bowel control. A typical cause of PTS would be a car accident or similar trauma involving a whip-lash injury.
What can make PTS difficult to diagnose is the fact that symptoms can often first appear long after the actual cause of the syrinx occurred, e.g. a car accident occurring and then the patient first experiencing PTS symptoms such as pain, loss of sensation, reduced ability on the skin to feel varying degrees of hot and cold, a number of months after car accident.
Symptoms
Syringomyelia causes a wide variety of neuropathic symptoms due to damage of the spinal cord. Patients may experience severe chronic pain, abnormal sensations and loss of sensation particularly in the hands. Some patients experience paralysis or paresis temporarily or permanently. A syrinx may also cause disruptions in the parasympathetic and sympathetic nervous systems, leading to abnormal body temperature or sweating, bowel control issues, or other problems. If the syrinx is higher up in the spinal cord or affecting the brainstem as in syringobulbia, vocal cord paralysis, ipsilateral tongue wasting, trigeminal nerve sensory loss, and other signs may occur.[4] Rarely, bladder stones can occur in the onset of weakness in the lower extremities.[5] Classically, syringomyelia spares the dorsal column/medial lemniscus of the spinal cord, leaving pressure, vibration, touch and proprioception intact in the upper extremities. Neuropathic arthropathy, also known as a Charcot joint, can occur, particularly in the shoulders, in patients with syringomyelia. The loss of sensory fibers to the joint is theorized to lead to damage of the joint over time.[6]
Diagnosis
Physicians now use magnetic resonance imaging (MRI) to diagnose syringomyelia. The MRI radiographer takes images of body anatomy, such as the brain and spinal cord, in vivid detail. This test will show the syrinx in the spine or any other conditions, such as the presence of a tumor. MRI is safe, painless, and informative and has greatly improved the diagnosis of syringomyelia.
The physician may order additional tests to help confirm the diagnosis. One of these is called electromyography (EMG), which measures muscle weakness. The doctor may also wish to test cerebrospinal fluid pressure levels and to analyze the cerebrospinal fluid by performing a lumbar puncture. In addition, computed axial tomography (CT) scans of a patient's head may reveal the presence of tumors and other abnormalities such as hydrocephalus.
Like MRI and CT scans, another test, called a myelogram, uses radiographs and requires a contrast medium to be injected into the subarachnoid space. Since the introduction of MRI this test is rarely necessary to diagnose syringomyelia.
The possible causes are trauma, tumors and congenital defects. It is most usually observed in the part of the spinal cord corresponding to the neck area. Symptoms are due to spinal cord damage and are: pain, decreased sensation of touch, weakness and loss of muscle tissue. The diagnosis is confirmed with a spinal CT, myelogram or MRI of the spinal cord. The cavity may be reduced by surgical decompression.
Furthermore, evidence also suggests that impact injuries to the thorax area highly correlate with the occurrence of a cervical-located syrinx.
Treatment
Surgery
The first step after diagnosis is finding a neurosurgeon who is experienced in the treatment of syringomyelia. Surgery is the only viable treatment for syringomyelia. Not all patients will advance to the stage where surgery is needed. Evaluation of the condition is often difficult because syringomyelia can remain stationary for long periods of time, and in some cases progress rapidly.
Surgery of the spinal cord has certain, characteristic risks associated with it and the benefits of a surgical procedure on the spine have to be weighed against the possible complications associated with any procedure. Surgical treatment is aimed at correcting the condition that allowed the syrinx to form. It is vital to bear in mind that the drainage of a syrinx does not necessarily mean the elimination of the syrinx-related symptoms, but rather is aimed at stopping progression. In cases involving an Arnold-Chiari malformation, the main goal of surgery is to provide more space for the cerebellum at the base of the skull and upper cervical spine without entering the brain or spinal cord. This often results in flattening or disappearance of the primary syrinx or cavity, over time, as the normal flow of cerebrospinal fluid is restored. If a tumor is causing syringomyelia, removal of the tumor is the treatment of choice and almost always eliminates the syrinx.
Surgery results in stabilization or modest improvement in symptoms for most patients. Delay in treatment may result in irreversible spinal cord injury. Recurrence of syringomyelia after surgery may make additional operations necessary; these may not be completely successful over the long term.
In some patients it may also be necessary to drain the syrinx, which can be accomplished using a catheter, drainage tubes, and valves. This system is also known as a shunt. Shunts are used in both the communicating and noncommunicating forms of the disorder. First, the surgeon must locate the syrinx. Then, the shunt is placed into it with the other end draining cerebrospinal fluid (CSF) into a cavity, usually the abdomen. This type of shunt is called a ventriculoperitoneal shunt and is particularly useful in cases involving hydrocephalus. By draining syrinx fluid, a shunt can arrest the progression of symptoms and relieve pain, headache, and tightness. Without correction, symptoms generally continue.
The decision to use a shunt requires extensive discussion between doctor and patient, as this procedure carries with it greater risk of injury to the spinal cord, infection, blockage, or hemorrhage and may not necessarily work for all patients. Draining the syrinx more quickly does not produce better outcomes, but a shunt may be required if the fluid in the syrinx is otherwise unable to drain.
In the case of trauma-related syringomyelia, the surgeon operates at the level of the initial injury. The syrinx collapses at surgery but a tube or shunt is usually necessary to prevent re-expansion.
Other
Surgery is not always recommended for syringomyelia patients. For many patients, the main treatment is analgesia. Physicians specializing in pain management can develop a medication and treatment plan to alleviate pain. One medication for "classical" back pain such as a weak or strong opioid (e.g. tramadol and Oxycontin respectively) combined with a medication to combat any neuropathic pain symptoms such as shooting and stabbing pains (e.g. Neurontin or Lyrica). In one pain management plan, an around-the-clock opiate such as fentanyl patches or Oxycontin are used in conjunction with a fast-acting opiate. However, to date no clinical trials have been published on the efficacy of these drugs in central neuropathic pain in this disorder. Trigger point injections for related muscle spasms and facet block injections may be beneficial. Long-term treatment of chronic pain should be monitored with blood tests to assess any adverse effects of the medication on the liver, with the dosages being then changed accordingly, depending on the outcome.
Drugs have no curative value as a treatment for syringomyelia. Radiation is used rarely and is of little benefit except in the presence of a tumor. In these cases, it can halt the extension of a cavity and may help to alleviate pain.
In the absence of symptoms, syringomyelia is usually not treated. In addition, a physician may recommend not treating the condition in patients of advanced age or in cases where there is no progression of symptoms. Whether treated or not, many patients will be told to avoid activities that involve straining.
Since the natural history of syringomyelia is poorly understood, a conservative approach may be recommended. When surgery is not yet advised, patients should be carefully monitored by a neurologist or neurosurgeon. Periodic MRI's and physical evaluations should be scheduled at the recommendation of a qualified physician.
Research
The precise causes of syringomyelia are still unknown. Scientists at the National Institute of Neurological Disorders and Stroke in Bethesda, Maryland, and at grantee institutions across the country continue to explore the mechanisms that lead to the formation of syrinxes in the spinal cord. For instance, Institute investigators have found that as the heart beats, the syrinx fluid is abruptly forced downward. They have also demonstrated a block to the free flow of cerebrospinal fluid that normally occurs in and out of the head during each heartbeat. Duke University is conducting research to see if syringomyelia might be genetic.[7]
Surgical techniques are also being refined by the neurosurgical research community. In one treatment approach currently being evaluated, neurosurgeons perform a decompressive procedure where the dura mater, a tough membrane covering the cerebellum and spinal cord, is enlarged with a graft. Like altering a suit of clothing, this procedure expands the area around the cerebellum and spinal cord, thus improving the flow of cerebrospinal fluid and eliminating the syrinx.
It is also important to understand the role of birth defects in the development of hindbrain malformations that can lead to syringomyelia. Learning when these defects occur during the development of the fetus can help us understand this and similar disorders, and may lead to preventive treatment that can stop the formation of many birth abnormalities. Dietary supplements of folic acid during pregnancy have already been found to reduce the number of cases of certain birth defects.
Diagnostic technology is another area for continued research. Already, MRI has enabled scientists to see conditions in the spine, including syringomyelia, even before symptoms appear. A new technology, known as dynamic MRI, allows investigators to view spinal fluid pulsating within the syrinx. CT scans allow physicians to see abnormalities in the brain, and other diagnostic tests have also improved greatly with the availability of new, non-toxic, contrast dyes.
See also
- Syringobulbia
- Central cord syndrome
- Dissociated sensory loss
- Ependymoma tumors
- Scoliosis is sometimes caused by syringomyelia.[8]
- Otto Kahler was a neurologist from the last 1800s who published the first complete description of syringomyelia.
- Bobby Jones, a famous golfer, was diagnosed with tumor-related syringomyelia in 1948.
- Brown-Sequard Syndrome
References
- ^ "Neurosurgical considerations in posttraumatic syringomyelia - Home Study Program". AORN Journal. January 2003. http://findarticles.com/p/articles/mi_m0FSL/is_1_77/ai_97058864. Retrieved 2009-02-12.
- ^ Brewis M, Poskanzer DC, Rolland C, et al., "Neurological disease in an English city". Acta Neurologica Scand Suppl 24:1--89, 1966.
- ^ Schurch B, Wichmann W, Rossier AB (January 1996). "Post-traumatic syringomyelia (cystic myelopathy): a prospective study of 449 patients with spinal cord injury". J. Neurol. Neurosurg. Psychiatr. 60 (1): 61–7. doi:10.1136/jnnp.60.1.61. PMC 486191. PMID 8558154. http://jnnp.bmj.com/cgi/pmidlookup?view=long&pmid=8558154.
- ^ Greenberg, David A, et al.: Clinical Neurology. 5th ed. Feb 9, 2002.
- ^ Nishida, Takayasu, et al. "A large bladder stone caused by syringomyelia". Japanese Journal of Clinical Urology, Vol.60, No. 6, pp 413-415, 2006. ISSN:0385-2393.
- ^ "Neuropathic Arthropathy of the Shoulder (Charcot Shoulder): Clinical Commentary" Medscape. Accessed 9 January 2011.
- ^ "Information about a Genetic Research Study for Chiari Type I Malformation (CMI) with or without Syringomyelia."
- ^ Yeom JS, Lee CK, Park KW, et al. (2007). "Scoliosis associated with syringomyelia: analysis of MRI and curve progression". Eur Spine J 16 (10): 1629–35. doi:10.1007/s00586-007-0472-1. PMC 2078323. PMID 17701226. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2078323.
External links
- Mayo Clinic's page
- Living With SM and CM Community Site
- Washington University School of Medicine - Link provided courtesy of Christopher S. Burton Syringomyelia Foundation's Research Team
Organizations
- American Syringomyelia Alliance Project (ASAP)
- Chiari & Syringomyelia Foundation (CSF)
- Christopher S. Burton Syringomyelia Foundation
- The Ann Conroy Trust (ACT)
- Irish ANTS (Syringomyelia Self Help Group)
- Syringomyelia Info
Congenital malformations and deformations of nervous system (Q00–Q07, 740–742) Brain Anencephaly (Acephaly, Acrania, Acalvaria, Iniencephaly) · Encephalocele · Arnold–Chiari malformationOtherCNS cyst (Porencephaly, Schizencephaly)Spinal cord OtherCategories:- Neurocutaneous conditions
- Rare diseases
- Congenital disorders of nervous system
- Spinal cord disorders
Wikimedia Foundation. 2010.