- Infertility
-
Infertility Classification and external resources ICD-10 N46, N97.0 ICD-9 606, 628 DiseasesDB 21627 MedlinePlus 001191 eMedicine med/3535 med/1167 MeSH D007246 Infertility primarily refers to the biological inability of a person to contribute to conception. Infertility may also refer to the state of a woman who is unable to carry a pregnancy to full term. There are many biological causes of infertility, some which may be bypassed with medical intervention.[1]
Women who are fertile experience a natural period of fertility before and during ovulation, and they are naturally infertile during the rest of the menstrual cycle. Fertility awareness methods are used to discern when these changes occur by tracking changes in cervical mucus or basal body temperature.
Contents
Definition
Definitions of infertility differ, with demographers tending to define infertility as childlessness in a population of women of reproductive age, while the epidemiological definition is based on "trying for" or "time to" a pregnancy, generally in a population of women exposed to a probability of conception.[2]
One definition of infertility that is frequently used by reproductive endocrinologists, the doctors specializing in infertility, to consider a couple eligible for treatment if:
- a woman under 35 has not conceived after 12 months of contraceptive-free intercourse. Twelve months is the lower reference limit for Time to Pregnancy (TTP) by the World Health Organization.[3]
- a woman over 35 has not conceived after 6 months of contraceptive-free sexual intercourse.
These time intervals would seem to be reversed; this is an area where public policy trumps science. The idea is that for women beyond age 35, every month counts and if made to wait another 6 months to prove the necessity of medical intervention, the problem could become worse. The corollary to this is that, by definition, failure to conceive in women under 35 isn't regarded with the same urgency as it is in those over 35.
Alternatively, the NICE guidelines define infertility as failure to conceive after regular unprotected sexual intercourse for 2 years in the absence of known reproductive pathology.[4]
A couple that has tried unsuccessfully to have a child after a certain period of time (often a short period, but definitions vary) is sometimes said to be subfertile, meaning less fertile than a typical couple. Both infertility (see above for definitions) and subfertility are defined as the inability to conceive after a certain period of time (the length of which vary), so often the two terms overlap.
Primary vs. secondary infertility
Couples with primary infertility have never been able to conceive,[5] while, on the other hand, secondary infertility is difficulty conceiving after already having conceived (and either carried the pregnancy to term or had a miscarriage). Secondary infertility is not present if there has been a change of partners (this follows tautologically from the convention of speaking of couples, rather than individuals, as being infertile; if there is a change of partners, then a new couple is created, with its own chances to be infertile.)
Prevalence
- Generally, worldwide it is estimated that one in seven couples have problems conceiving, with the incidence similar in most countries independent of the level of the country's development.[citation needed]
- Fertility problems affect one in seven couples in the UK. Most couples (about 84 out of every 100) who have regular sexual intercourse (that is, every 2 to 3 days) and who do not use contraception will get pregnant within a year. About 92 out of 100 couples who are trying to get pregnant do so within 2 years.[6]
- Women become less fertile as they get older. For women aged 35, about 94 out of every 100 who have regular unprotected sexual intercourse will get pregnant after 3 years of trying. For women aged 38, however, only 77 out of every 100 will do so. The effect of age upon men's fertility is less clear.[6]
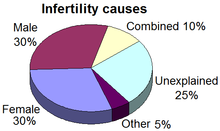
- In people going forward for IVF in the UK, roughly half of fertility problems with a diagnosed cause are due to problems with the man, and about half due to problems with the woman. However, about one in five cases of infertility has no clear diagnosed cause.[7]
- In Britain, male factor infertility accounts for 25% of infertile couples, while 25% remain unexplained. 50% are female causes with 25% being due to anovulation and 25% tubal problems/other.[8]
- In Sweden, approximately 10% of couples are infertile.[9] In approximately one third of these cases the man is the factor, in one third the woman is the factor, and in the remaining third the infertility is a product of factors on both parts.
Causes
This section deals with unintentional causes of sterility. For more information about surgical techniques for preventing procreation, see Sterilization (surgical procedure).
Causes in either sex
Factors that can cause male as well as female infertility are:
- Genetic factors
- A Robertsonian translocation in either partner may cause recurrent spontaneous abortions or complete infertility.
- General factors
- Diabetes mellitus, thyroid disorders, adrenal disease
- Hypothalamic-pituitary factors
- Hyperprolactinemia
- Hypopituitarism
- The presence of anti-thyroid antibodies is associated with an increased risk of unexplained subfertility with an odds ratio of 1.5 and 95% confidence interval of 1.1–2.0.[11]
- Environmental factors
German scientists have reported that a virus called Adeno-associated virus might have a role in male infertility,[14] though it is otherwise not harmful.[15] Mutation that alters human DNA adversely can cause infertility, the human body thus preventing the tainted DNA from being passed on[citation needed].
Specific female causes
The following causes of infertility may only be found in females.
For a woman to conceive, certain things have to happen: intercourse must take place around the time when an egg is released from her ovary; the systems that produce eggs and sperm have to be working at optimum levels; and her hormones must be balanced.[16]
Some women are infertile because their ovaries do not mature and release eggs. In this case synthetic FSH by injection or Clomid (Clomiphene citrate) via a pill can be given to stimulate follicles to mature in the ovaries.
Problems affecting women include endometriosis or damage to the fallopian tubes (which may have been caused by infections such as chlamydia).
Other factors that can affect a woman's chances of conceiving include being over- or underweight, or her age as female fertility declines sharply after the age of 35. Sometimes it can be a combination of factors, and sometimes a clear cause is never established.
Common causes of infertility of females include:
- ovulation problems
- tubal blockage
- age-related factors
- uterine problems
- previous tubal ligation
- endometriosis
Specific male causes
The main cause of male infertility is low semen quality.
Combined infertility
In some cases, both the man and woman may be infertile or sub-fertile, and the couple's infertility arises from the combination of these conditions. In other cases, the cause is suspected to be immunological or genetic; it may be that each partner is independently fertile but the couple cannot conceive together without assistance.
Unexplained infertility
Main article: Unexplained infertilityIn the US, up to 20% of infertile couples have unexplained infertility.[17] In these cases abnormalities are likely to be present but not detected by current methods. Possible problems could be that the egg is not released at the optimum time for fertilization, that it may not enter the fallopian tube, sperm may not be able to reach the egg, fertilization may fail to occur, transport of the zygote may be disturbed, or implantation fails. It is increasingly recognized that egg quality is of critical importance and women of advanced maternal age have eggs of reduced capacity for normal and successful fertilization. Also, polymorphisms in folate pathway genes could be one reason for fertility complications in some women with unexplained infertility.[18]
Assessment
Main article: Fertility testingIf both partners are young and healthy and have been trying to conceive for 12 months to one year without success, a visit to the family doctor could help to highlight potential medical problems earlier rather than later. The doctor may also be able to suggest lifestyle changes to increase the chances of conceiving.[19]
Women over the age of 35 should see their family doctor after six months as fertility tests can take some time to complete, and age may affect the treatment options that are open in that case.
A family doctor will take a medical history and give a physical examination. They can also carry out some basic tests on both partners to see if there is an identifiable reason for not having achieved a pregnancy yet. If necessary, they can refer patients to a fertility clinic or a local hospital for more specialized tests. The results of these tests will help determine which is the best fertility treatment.
Treatment
Treatment methods for infertility may be grouped as medical or complementary and alternative treatments. Some methods may be used in concert with other methods.
At-home conception kit
In 2007 the FDA cleared the first at home tier one medical conception device to aid in conception. The key to the kit are cervical caps for conception. This at home [cervical cap] insemination method allows all the semen to be placed up against the cervical os for six hours allowing all available sperm to be placed directly on the cervical os. For low sperm count, low sperm motility, or a tilted cervix using a cervical cap will aid in conception. This is a prescriptive medical device.[20]
At-home assessment
Prior to undergoing expensive fertility procedures many women and couples will turn to online sources to determine their estimate chances of success. A take-home baby assessment can provide a best guess estimate compared with women who have succeeded with in vitro fertilization, based on variables such as maternal age duration of infertility and number of prior pregnancies.[21]
Medical treatments
Medical treatment of infertility generally involves the use of fertility medication, medical device, surgery, or a combination of the following. If the sperm are of good quality and the mechanics of the woman's reproductive structures are good (patent fallopian tubes, no adhesions or scarring), physicians may start by prescribing a course of ovarian stimulating medication. The physician may also suggest using a conception cap cervical cap, which the patient uses at home by placing the sperm inside the cap and putting the conception device on the cervix, or intrauterine insemination (IUI), in which the doctor introduces sperm into the uterus during ovulation, via a catheter. In these methods, fertilization occurs inside the body.
If conservative medical treatments fail to achieve a full term pregnancy, the physician may suggest the patient undergo in vitro fertilization (IVF). IVF and related techniques (ICSI, ZIFT, GIFT) are called assisted reproductive technology (ART) techniques.
ART techniques generally start with stimulating the ovaries to increase egg production. After stimulation, the physician surgically extracts one or more eggs from the ovary, and unites them with sperm in a laboratory setting, with the intent of producing one or more embryos. Fertilization takes place outside the body, and the fertilized egg is reinserted into the woman's reproductive tract, in a procedure called embryo transfer.
Other medical techniques are e.g. tuboplasty, assisted hatching, and Preimplantation genetic diagnosis.
Complementary and alternative treatments
Three complementary or alternative female infertility treatments have been scientifically tested, with results published in peer-reviewed medical journals.
- Group psychological intervention: A 2000 Harvard Medical School study examined the effects of group psychological intervention on infertile women (trying to conceive a duration of one to two years). The two intervention groups—a support group and a cognitive behavior group—had statistically significant higher pregnancy rates than the control group.[22]
- Acupuncture: Acupuncture performed 25 minutes before and after IVF embryo transfer increased IVF pregnancy rates in a German study published in 2002.[23] In a similar study conducted by The University of South Australia in 2006, there was no statistically significant difference in fertility between the group which received acupuncture and the control group.[24] Although definitive results of the effects of acupuncture on embryo transfer remain a topic of discussion, study authors state that it appears to be a safe - although not necessarily effective - adjunct to IVF.[24][25]
- Manual physical therapy: The Wurn Technique, a manual manipulative physical therapy treatment, was shown in peer reviewed publications to improve natural and IVF pregnancy rates in infertile women in a 2004 study,[26] and to open and return function to blocked fallopian tubes in a 2008 study.[27] The therapy was designed to address adhesions restricting function and mobility of the reproductive organs.[26][27]
Tourism
Fertility tourism is the practice of traveling to another country for fertility treatments.[28] It may be regarded as a form of medical tourism. The main reasons for fertility tourism are legal regulation of the sought procedure in the home country, or lower price. In-vitro fertilization and donor insemination are major procedures involved.
Ethics
There are several ethical issues associated with infertility and its treatment.
- High-cost treatments are out of financial reach for some couples.
- Debate over whether health insurance companies should be forced to cover infertility treatment.
- Allocation of medical resources that could be used elsewhere
- The legal status of embryos fertilized in vitro and not transferred in vivo. (See also Beginning of pregnancy controversy).
- Pro-life opposition to the destruction of embryos not transferred in vivo.
- IVF and other fertility treatments have resulted in an increase in multiple births, provoking ethical analysis because of the link between multiple pregnancies, premature birth, and a host of health problems.
- Religious leaders' opinions on fertility treatments.
- Infertility caused by DNA defects on the Y chromosome is passed on from father to son. If natural selection is the primary error correction mechanism that prevents random mutations on the Y chromosome, then fertility treatments for men with abnormal sperm (in particular ICSI) only defer the underlying problem to the next male generation.
Many countries have special frameworks for dealing with the ethical and social issues around fertility treatment.
- One of the best known is the HFEA – The UK's regulator for fertility treatment and embryo research. This was set up on 1 August 1991 following a detailed commission of enquiry led by Mary Warnock in the 1980s
- A similar model to the HFEA has been adopted by the rest of the countries in the European Union. Each country has its own body or bodies responsible for the inspection and licencing of fertility treatment under the EU Tissues and Cells directive [29]
Psychological impact
The consequences of infertility are manifold and can include societal repercussions and personal suffering. Advances in assisted reproductive technologies, such as IVF, can offer hope to many couples where treatment is available, although barriers exist in terms of medical coverage and affordability. The medicalization of infertility has unwittingly led to a disregard for the emotional responses that couples experience, which include distress, loss of control, stigmatization, and a disruption in the developmental trajectory of adulthood.[32]
Infertility may have profound psychological effects. Partners may become more anxious to conceive, ironically increasing sexual dysfunction.[33] Marital discord often develops in infertile couples, especially when they are under pressure to make medical decisions. Women trying to conceive often have clinical depression rates similar to women who have heart disease or cancer.[34] Even couples undertaking IVF face considerable stress.[35]
Emotional stress and marital difficulties are greater in couples where the infertility lies with the man.[36]
Social impact
In many cultures, inability to conceive bears a stigma. In closed social groups, a degree of rejection (or a sense of being rejected by the couple) may cause considerable anxiety and disappointment. Some respond by actively avoiding the issue altogether; middle-class men are the most likely to respond in this way.[37]
In an effort to end the shame and secrecy of infertility, Redbook in October 2011 launched a video campaign, The Truth About Trying, to start an open conversation about infertility, which strikes one in eight women in the United States. In a survey of couples having difficulty conceiving, conducted by the pharmaceutical company Merck, 61 percent of respondents hid their infertility from family and friends. [38] Nearly half didn't even tell their mothers. The message of those speaking out: It's not always easy to get pregnant, and there's no shame in that.
There are legal ramifications as well. Infertility has begun to gain more exposure to legal domains. An estimated 4 million workers in the U.S. used the Family and Medical Leave Act (FMLA) in 2004 to care for a child, parent or spouse, or because of their own personal illness. Many treatments for infertility, including diagnostic tests, surgery and therapy for depression, can qualify one for FMLA leave.
Fictional representation
Perhaps except for infertility in science fiction, films and other fiction depicting emotional struggles of assisted reproductive technology have had an upswing first in the latter part of the 2000s decade, although the techniques have been available for decades.[39] Yet, the amount of people that can relate to it by personal experience in one way or another is ever growing, and the variety of trials and struggles is huge.[39]
Any individual examples are referred to individual subarticles of assisted reproductive technology
See also
- Advanced maternal age
- Childlessness
- Conception device
- Inherited sterility in insects
- Medical ethics
- Oncofertility, fertility in cancer patients
- Surrogate marriage
References
- ^ Makar RS, Toth TL (2002). "The evaluation of infertility". Am J Clin Pathol. 117 Suppl: S95–103. PMID 14569805.
- ^ Gurunath, S.; Pandian, Z.; Anderson, R. A.; Bhattacharya, S. (2011). "Defining infertility--a systematic review of prevalence studies". Human Reproduction Update 17 (5): 575. doi:10.1093/humupd/dmr015.
- ^ Cooper TG, Noonan E, von Eckardstein S, et al. (2010). "World Health Organization reference values for human semen characteristics". Hum. Reprod. Update 16 (3): 231–45. doi:10.1093/humupd/dmp048. PMID 19934213.
- ^ [1] Fertility: Assessment and Treatment for People with Fertility Problems. London: RCOG Press. 2004. ISBN 1-900364-97-2.
- ^ MedlinePlus Encyclopedia Infertility
- ^ a b NICE fertility guidance
- ^ HFEA Chart on reasons for infertility
- ^ Khan, Khalid; Janesh K. Gupta; Gary Mires (2005). Core clinical cases in obstetrics and gynaecology: a problem-solving approach. London: Hodder Arnold. pp. 152. ISBN 0-340-81672-4.
- ^ Sahlgrenska University Hospital. (translated from the Swedish sentence: "Cirka 10% av alla par har problem med ofrivillig barnlöshet.")
- ^ a b Regulated fertility services: a commissioning aid - June 2009, from the Department of Health UK
- ^ Van Den Boogaard, E.; Vissenberg, R.; Land, J. A.; Van Wely, M.; Van Der Post, J. A. M.; Goddijn, M.; Bisschop, P. H. (2011). "Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy: A systematic review". Human Reproduction Update 17 (5): 605–619. doi:10.1093/humupd/dmr024. PMID 21622978.
- ^ Mendiola J, Torres-Cantero AM, Moreno-Grau JM, et al. (Jun 2008). "Exposure to environmental toxins in males seeking infertility treatment: a case-controlled study". Reprod Biomed Online 16 (6): 842–50. doi:10.1016/S1472-6483(10)60151-4. PMID 18549695. http://openurl.ingenta.com/content/nlm?genre=article&issn=1472-6483&volume=16&issue=6&spage=842&aulast=Mendiola.
- ^ Smith EM, Hammonds-Ehlers M, Clark MK, Kirchner HL, Fuortes L (Feb 1997). "Occupational exposures and risk of female infertility". J Occup Environ Med. 39 (2): 138–47. doi:10.1097/00043764-199702000-00011. PMID 9048320. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1076-2752&volume=39&issue=2&spage=138.
- ^ http://www.newscientist.com/article.ns?id=dn1483
- ^ "Virus linked to infertility". BBC News. 2001-10-27. http://news.bbc.co.uk/1/hi/health/1620174.stm. Retrieved 2010-04-02.
- ^ About infertility & fertility problems
- ^ Unexplained Infertility Background, Tests and Treatment Options Advanced Fertility Center of Chicago
- ^ Altmäe, S.; Stavreus-Evers, A.; Ruiz, J.; Laanpere, M.; Syvänen, T.; Yngve, A.; Salumets, A.; Nilsson, T. (2010). "Variations in folate pathway genes are associated with unexplained female infertility". Fertility and sterility 94 (1): 130–137. doi:10.1016/j.fertnstert.2009.02.025. PMID 19324355.
- ^ Infertility Help: When & where to get help for fertility treatment
- ^ http://www.newsrx.com/pr_details.php?type=1&id=2904
- ^ http://www.formyodds.com
- ^ Domar AD, Clapp D, Slawsby EA, Dusek J, Kessel B, Freizinger M (Apr 2000). "Impact of group psychological interventions on pregnancy rates in infertile women". Fertil Steril. 73 (4): 805–11. doi:10.1016/S0015-0282(99)00493-8. PMID 10731544. http://linkinghub.elsevier.com/retrieve/pii/S0015-0282(99)00493-8.
- ^ Paulus WE, Zhang M, Strehler E, El-Danasouri I, Sterzik K (Apr 2002). "Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy". Fertil. Steril. 77 (4): 721–4. doi:10.1016/S0015-0282(01)03273-3. PMID 11937123. http://linkinghub.elsevier.com/retrieve/pii/S0015028201032733.
- ^ a b Smith C, Coyle M, Norman RJ (May 2006). "Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer". Fertil Steril. 85 (5): 1352–8. doi:10.1016/j.fertnstert.2005.12.015. PMID 16600225.
- ^ Stener-Victorin E, Humaidan P (Dec 2006). "Use of acupuncture in female infertility and a summary of recent acupuncture studies related to embryo transfer". Acupunct Med 24 (4): 157–63. doi:10.1136/aim.24.4.157. PMID 17264833. http://www.acupunctureinmedicine.org.uk/linkout.php?article=24_157.[dead link]
- ^ a b Wurn BF, Wurn LJ, King CR, et al. (2004). "Treating female infertility and improving IVF pregnancy rates with a manual physical therapy technique". MedGenMed 6 (2): 51. PMC 1395760. PMID 15266276. http://www.medscape.com/viewarticle/480429.
- ^ a b Wurn BF, Wurn LJ, King CR, et al. (2008). "Treating fallopian tube occlusion with a manual pelvic physical therapy". Altern Ther Health Med 14 (1): 18–23. PMID 18251317.
- ^ wordspy.com
- ^ http://europa.eu/scadplus/leg/en/cha/c11573.htm EU Tissues and Cells directive
- ^ Assisted Human Reproduction Canada
- ^ ITA
- ^ Cousineau TM, Domar AD. (2007). "Psychological impact of infertility". Best Pract Res Clin Obstet Gynaecol. 21 (2): 293–308. doi:10.1016/j.bpobgyn.2006.12.003. PMID 17241818.
- ^ Donor insemination Edited by C.L.R. Barratt and I.D. Cooke. Cambridge (England): Cambridge University Press, 1993. 231 pages., page 13, citing Berger (1980)
- ^ Domar AD, Zuttermeister PC, Friedman R (1993). "The psychological impact of infertility: a comparison with patients with other medical conditions". J Psychosom Obstet Gynaecol 14 Suppl: 45–52. PMID 8142988.
- ^ Beutel M, Kupfer J, Kirchmeyer P, et al. (Jan 1999). "Treatment-related stresses and depression in couples undergoing assisted reproductive treatment by IVF or ICSI". Andrologia 31 (1): 27–35. doi:10.1046/j.1439-0272.1999.00231.x. PMID 9949886. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0303-4569&date=1999&volume=31&issue=1&spage=27.
- ^ Donor insemination Edited by C.L.R. Barratt and I.D. Cooke. Cambridge (England): Cambridge University Press, 1993. 231 pages., page 13, in turn citing Connolly, Edelmann & Cooke 1987
- ^ Schmidt L, Christensen U, Holstein BE (Apr 2005). "The social epidemiology of coping with infertility". Hum Reprod. 20 (4): 1044–52. doi:10.1093/humrep/deh687. PMID 15608029.
- ^ "The invisible pain of Infertility", Redbook, October 2011
- ^ a b chicagotribune.com Heartache of infertility shared on stage, screen By Colleen Mastony, Tribune reporter. June 21, 2009
Further reading
- Fertility: Assessment and Treatment for People with Fertility Problems. London: RCOG Press. 2004. ISBN 1-900364-97-2.
- Pamela Mahoney Tsigdinos (2009). Silent Sorority: A Barren Woman Gets Busy, Angry, Lost and Found. USA: BookSurge Publishing. pp. 218. ISBN 1-439231-56-7.
External links
- RCOG clinical guidelines for infertility (concise guidelines)
- Fertility: Assessment and Treatment for People with Fertility Problems, 2004 (extensive guidelines)
- Fertility treatment and clinics in the UK
- GeneReviews/NCBI/NIH/UW entry on CATSPER-Related Male Infertility
- CBC Digital Archives – Fighting Female Infertility
- InterNational Council on Infertility Information Dissemination
- Infertility not just a Female Problem
- Assisted Reproduction in Judaism
- Facing Life Without Children When It Isn’t by Choice
- Patient Voices – Infertility
- World Congress on Controversies in Obstetrics, Gynecology & Infertility (COGI)
Family planning and reproductive health Rights Education Planning Reproductive life plan · Childfree · Parenting (Childbirth, Adoption, Foster care) · Birth control · Safe sexHealth Pregnancy Medicine Disorder By country Related navboxes {{Birth control methods}} · {{Pregnancy}} · {{Sex}} · {{sexual abuse}} · {{STD/STI}} · {{Assisted reproductive technology}}
Female diseases of the pelvis and genitals (N70–N99, 614–629) Internal AdnexaOophoritis · Ovarian cyst (Follicular cyst of ovary, Corpus luteum cyst, Theca lutein cyst) · Endometriosis of ovary · Ovarian hyperstimulation syndrome · Ovarian torsion · Ovarian apoplexy · Mittelschmerz · Female infertility (Anovulation, Poor ovarian reserve)Cervicitis · Cervical polyp · Nabothian cyst · Cervical incompetence · Female infertility (Cervical stenosis) · Cervical dysplasiaGeneralVaginitis (Bacterial vaginosis, Atrophic vaginitis, Candidal vulvovaginitis) · Leukorrhea/Vaginal discharge · Hematocolpos/HydrocolposOther/generalExternal Categories:- Andrology
- Fertility medicine
- Infertility
- Fertility
Wikimedia Foundation. 2010.