- Thyroid
Infobox Anatomy
Name = Thyroid
Latin = glandula thyroidea
GraySubject = 272
GrayPage = 1269

Caption = Endocrine system
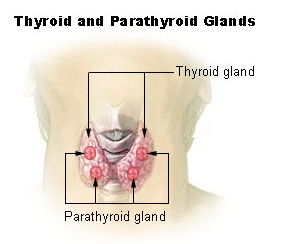
Caption2 = Thyroid and parathyroid.
Precursor = 4thBranchial pouch
System = endocinal jubachina system
Artery =superior thyroid artery ,inferior thyroid artery ,thyreoidea ima
Vein =superior thyroid vein ,middle thyroid vein ,inferior thyroid vein
Nerve =middle cervical ganglion ,inferior cervical ganglion
Lymph =
MeshName = Thyroid+Gland
MeshNumber = A06.407.900
DorlandsPre = g_06
DorlandsSuf = 12392768The thyroid is one of the largest
endocrine gland s in the body. This gland is found in theneck inferior to (below) thethyroid cartilage (also known as theAdam's apple in men) and at approximately the same level as thecricoid cartilage . The thyroid controls how quickly the body burnsenergy , makesproteins , and how sensitive the body should be to otherhormones .The thyroid participates in these processes by producing thyroid hormones, principally
thyroxine (T4) andtriiodothyronine (T3). These hormones regulate the rate ofmetabolism and affect the growth and rate of function of many other systems in the body.Iodine is an essential component of both T3 and T4. The thyroid also produces the hormonecalcitonin , which plays a role incalcium homeostasis .The thyroid is controlled by the
hypothalamus andpituitary . The gland gets its name from the Greek word for "door", after the shape of the related thyroid cartilage.Hyperthyroidism (overactive thyroid) andhypothyroidism (underactive thyroid) are the most common problems of the thyroid gland.Anatomy
The thyroid gland is a butterfly-shaped organ and is composed of two cone-like lobes or wings: "lobus dexter" (right lobe) and "lobus sinister" (left lobe), connected with the isthmus. The organ is situated on the anterior side of the neck, lying against and around the
larynx and trachea, reaching posteriorly theoesophagus andcarotid sheath . It starts cranially at the oblique line on thethyroid cartilage (just below the laryngeal prominence orAdam's apple ) and extends inferiorly to the fourth to sixthtracheal ring Fact|date=January 2008. It is difficult to demarcate the gland's upper and lower border with vertebral levels as it moves position in relation to these during swallowing.The thyroid gland is covered by a fibrous sheath, the "capsula glandulae thyroidea", composed of an internal and external layer. The external layer is anteriorly continuous with the "lamina pretrachealis fasciae cervicalis" and posteriorolaterally continuous with the
carotid sheath . The gland is covered anteriorly withinfrahyoid muscles and laterally with thesternocleidomastoid muscle . Posteriorly, the gland is fixed to thecricoid and tracheal cartilage andcricopharyngeus muscle by a thickening of the fascia to form theposterior suspensory ligament of Berry [cite journal | author = Yalçin B., Ozan H. | year = 2006 | month = feb | title = Detailed investigation of the relationship between the inferior laryngeal nerve including laryngeal branches and ligament of Berry | journal = Journal of the American College of Surgeons | volume = 202 | issue = 2 | pages = 291–6 | pmid = 16427555 | doi = 10.1016/j.jamcollsurg.2005.09.025 ] [Citation
last1 = Lemaire | first1 = David | title = eMedicine - Thyroid anatomy | date =2005-05-27 | year = 2005 | url = http://www.emedicine.com/ent/topic532.htm | accessdate = 2008-01-19 ] . In variable extent,Zuckerkandl's tubercle , a pyramidal extension of the thyroid lobe, is present at the most posterior side of the lobecite journal |author=Yalçin B, Poyrazoglu Y, Ozan H |title=Relationship between Zuckerkandl's tubercle and the inferior laryngeal nerve including the laryngeal branches |journal=Surg. Today |volume=37 |issue=2 |pages=109–13 |year=2007 |pmid=17243027 |doi=10.1007/s00595-006-3346-y] cite journal |author=Mirilas P, Skandalakis JE |title=Zuckerkandl's tubercle: Hannibal ad Portas |journal=J. Am. Coll. Surg |volume=196 |issue=5 |pages=796–801 |year=2003 |pmid=12742214 |doi=10.1016/S1072-7515(02)01831-8 |url=http://linkinghub.elsevier.com/retrieve/pii/S1072-7515(02)01831-8] . In this region therecurrent laryngeal nerve and the inferior thyroid artery pass next to or in the ligament and tubercle. Between the two layers of the capsule and on the posterior side of the lobes there are on each side twoparathyroid gland s.The
thyroid isthmus is variable in presence and size, and can encompass a cranially extending pyramid lobe ("lobus pyramidalis "or" processus pyramidalis"), remnant of thethyroglossal duct . The thyroid is one of the larger endocrine glands, weighing 2-3 grams in neonates and 18-60 grams in adults, and is increased in pregnancyFact|date=January 2008.The thyroid is supplied with arterial blood from the
superior thyroid artery , a branch of theexternal carotid artery , and theinferior thyroid artery , a branch of thethyrocervical trunk , and sometimes by thethyroid ima artery , branching directly from the aortic arch. The venous blood is drained viasuperior thyroid vein s, draining in theinternal jugular vein , and viainferior thyroid vein s, draining via the "plexus thyroideus impar" in the leftbrachiocephalic vein .Lymphatic drainage passes frequently the lateral deep cervical lymph nodes and the pre- and parathracheal lymph nodes. The gland is supplied bysympathetic nerve input from thesuperior cervical ganglion and thecervicothoracic ganglion of thesympathetic trunk Fact|date=January 2008, and byparasympathetic nerve input from thesuperior laryngeal nerve and therecurrent laryngeal nerve .Embryological development
In the fetus, at 3-4 weeks of gestation, the thyroid gland appears as an epithelial proliferation in the floor of the pharynx at the base of the tongue between the
tuberculum impar and thecopula linguae at a point latter indicated by the foramen cecum. Subsequently the thyroid descends in front of the pharyngeal gut as a bilobed diverticulum through thethyroglossal duct . Over the next few weeks, it migrates to the base of the neck. During migration, the thyroid remains connected to the tongue by a narrow canal, thethyroglossal duct .Follicles of the thyroid begin to make colloid in the 11th week and thyroxine by the 18th week.Histology
At the microscopic level, there are three primary features of the thyroid:
Physiology
The primary function of the thyroid is production of the hormones
thyroxine (T4),triiodothyronine (T3), andcalcitonin . Up to 80% of the T4 is converted to T3 by peripheral organs such as theliver ,kidney andspleen . T3 is about ten times more active than T4. [http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=endocrin.chapter.235 The thyroid gland] in "Endocrinology: An Integrated Approach" by Stephen Nussey and Saffron Whitehead (2001) Published by BIOS Scientific Publishers Ltd. ISBN 1-85996-252-1 .]T3 and T4 production and action
Thyroxine (T4) is synthesised by the follicular cells from freetyrosine and on thetyrosine residues of the protein calledthyroglobulin (TG).Iodine is captured with the "iodine trap" by thehydrogen peroxide generated by the enzymethyroid peroxidase (TPO)cite journal | author=Ekholm R, Bjorkman U | title=Glutathione peroxidase degrades intracellular hydrogen peroxide and thereby inhibits intracellular protein iodination in thyroid epithelium | journal=Endocrinology | volume=138 | issue=7 | year=1997 | pages=2871–2878 | doi= 10.1210/en.138.7.2871|pmid=9202230] and linked to the 3' and 5' sites of the benzene ring of the tyrosine residues on TG, and on free tyrosine. Upon stimulation by thethyroid-stimulating hormone (TSH), the follicular cells reabsorb TG and proteolytically cleave the iodinated tyrosines from TG, forming T4 and T3 (in T3, one iodine is absent compared to T4), and releasing them into theblood . Deiodinase enzymes convert T4 to T3.cite journal | author=Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR | title=Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases | journal=Endocr Rev | volume=23 | issue=1 | year=2002 | pages=38–89 | doi= 10.1210/er.23.1.38|pmid=11844744] Thyroid hormone that is secreted from the gland is about 90% T4 and about 10% T3.Cells of the brain are a major target for the
thyroid hormone s T3 and T4.Thyroid hormone s play a particularly crucial role in brain maturation during fetal development.cite journal | author=Kester MH, Martinez de Mena R, Obregon MJ, Marinkovic D, Howatson A, Visser TJ, Hume R, Morreale de Escobar G | title=Iodothyronine levels in the human developing brain: major regulatory roles of iodothyronine deiodinases in different areas | journal= J Clin Endocrinol Metab| volume=89 | issue=7 | year=2004 | pages=3117–3128 | doi= 10.1210/jc.2003-031832 |pmid=15240580 ] A transport protein ( [http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=gene&cmd=Retrieve&dopt=full_report&list_uids=53919 OATP1C1] ) has been identified that seems to be important for T4 transport across theblood brain barrier .Jansen J, Friesema ECH, Milici C, Visser TJ (2005). Thyroid hormone transporters in health and disease. "Thyroid" 15;757-768. PMID 16131319.] A second transport protein ( [http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=300095 MCT8] ) is important for T3 transport across brain cell membranes.In the blood, T4 and T3 are partially bound to
thyroxine-binding globulin ,transthyretin and albumin. Only a very small fraction of the circulating hormone is free (unbound) - T4 0.03% and T3 0.3%. Only the free fraction has hormonal activity. As with thesteroid hormone s and retinoic acid, thyroid hormones cross thecell membrane and bind tointracellular receptor s (α1, α2, β1 and β2), which act alone, in pairs or together with theretinoid X-receptor astranscription factor s to modulateDNA transcription [http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/thyroid/receptors.html] .T3 and T4 regulation
The production of
thyroxine andtriiodothyronine is regulated bythyroid-stimulating hormone (TSH), released by theanterior pituitary (that is in turn released as a result of TRH release by the hypothalamus). The thyroid andthyrotrope s form a negative feedback loop: TSH production is suppressed when the T4 levels are high, and vice versa. The TSH production itself is modulated bythyrotropin-releasing hormone (TRH), which is produced by thehypothalamus and secreted at an increased rate in situations such as cold (in which an accelerated metabolism would generate more heat). TSH production is blunted bysomatostatin (SRIH), rising levels ofglucocorticoid s andsex hormones (estrogen andtestosterone ), and excessively high blood iodide concentration.Calcitonin
An additional hormone produced by the thyroid contributes to the regulation of blood calcium levels.
Parafollicular cells producecalcitonin in response tohypercalcemia . Calcitonin stimulates movement of calcium intobone , in opposition to the effects ofparathyroid hormone (PTH). However,calcitonin seems far less essential than PTH, ascalcium metabolism remains clinically normal after removal of the thyroid, but not theparathyroids .ignificance of iodine
In areas of the world where
iodine (essential for the production ofthyroxine , which contains four iodine atoms) is lacking in the diet, the thyroid gland can be considerably enlarged, resulting in the swollen necks of endemicgoitre .Thyroxine is critical to the regulation ofmetabolism and growth throughout the animal kingdom. Amongamphibia ns, for example, administering a thyroid-blocking agent such aspropylthiouracil (PTU) can preventtadpole s from metamorphosing into frogs; conversely, administeringthyroxine will trigger metamorphosis.In humans, children born with
thyroid hormone deficiency will have physical growth and development problems, and brain development can also be severely impaired, in the condition referred to ascretinism . Newborn children in many developed countries are now routinely tested forthyroid hormone deficiency as part ofnewborn screening by analysis of a drop of blood. Children withthyroid hormone deficiency are treated by supplementation with synthetic thyroxine, which enables them to grow and develop normally.Because of the thyroid's selective uptake and concentration of what is a fairly rare element, it is sensitive to the effects of various radioactive
isotope s of iodine produced bynuclear fission . In the event of large accidental releases of such material into the environment, the uptake of radioactive iodine isotopes by the thyroid can, in theory, be blocked by saturating the uptake mechanism with a large surplus of non-radioactive iodine, taken in the form of potassium iodide tablets. While biological researchers making compounds labelled with iodine isotopes do this, in the wider world such preventive measures are usually not stockpiled before an accident, nor are they distributed adequately afterward. One consequence of the Chernobyl disaster was an increase inthyroid cancer s in children in the years following the accident. [ [http://news.bbc.co.uk/hi/english/sci/tech/newsid_1319000/1319386.stm BBC NEWS | Science/Nature | Chernobyl children show DNA changes ] ]The use of
iodised salt is an efficient way to add iodine to the diet. It has eliminated endemiccretinism in most developed countries, and some governments have made the iodination of flour mandatory. Potassium iodide and Sodium iodide are the most active forms of supplemental iodine.Diseases
Hyper- and hypofunction
Depending on the prescribed school of thought, affects between 2% and 20% of the population. [http://thyroid.about.com/od/gettestedanddiagnosed/a/tshtestwars.htm] in "Endocrinology: An Integrated Approach" by Mary Shomon (2006) Published by About.com]
*Hypothyroidism (underactivity)
**Hashimoto's thyroiditis /thyroiditis
**Ord's thyroiditis
** Postoperative hypothyroidism
**Postpartum thyroiditis
**Silent thyroiditis
** Acute thyroiditis
** Iatrogenic hypothyroidism
**Thyroid hormone resistance
**Euthyroid sick syndrome
*Hyperthyroidism (overactivity)
** Thyroid storm
**Graves' disease
**Toxic thyroid nodule
**Toxic nodular struma (Plummer's disease)
** Hashitoxicosis
** Iatrogenic hyperthyroidism
**De Quervain's thyroiditis (inflammation starting as hyperthyroidism, can end as hypothyroidism)Anatomical problems
*
Goitre
**Endemic goitre
**Diffuse goitre
**Multinodular goitre
* Lingual thyroid
* Thyroglossal duct cystTumors
*
Thyroid adenoma
*Thyroid cancer
** Papillary
** Follicular
** Medullary
** Anaplastic
*Lymphoma s andmetastasis from elsewhere (rare)Deficiencies
*
Cretinism Medication linked to thyroid disease includes
amiodarone ,lithium salt s, some types ofinterferon and IL-2.Diagnosis
Blood tests
* The measurement of thyroid-stimulating hormone (TSH) levels is often used by doctors as a screening test. Elevated TSH levels can signify an inadequate
thyroid hormone production, while suppressed levels can point at excessive unregulated production of hormone.
* If TSH is abnormal, decreased levels ofthyroid hormones T4 and T3 may be present; T4 and T3 levels may be determined with blood tests to confirm that their levels are decreased.
* Autoantibodies may be detected in various disease states (anti-TG, anti-TPO, TSH receptor stimulating antibodies).
* There are two cancer markers for thyroid derived cancers.Thyroglobulin (TG) for well differentiated papillary or follicular adenocarcinoma, and the rare medullary thyroid cancer hascalcitonin as the marker.
* Very infrequently, TBG andtransthyretin levels may be abnormal; these are not routinely tested.
*To differentiate between different types of hypothyroidism, a specific test may be used. Thyroid-releasing hormone (TRH) is injected into the body through a vein. This hormone is naturally secreted by the hypothalamus and stimulates the pituitary gland. The pituitary responds by releasing thyroid -stimulating hormone (TSH). Large amounts of externally administered TRH can suppress the subsequent release of TSH. This amount of release-suppression is exaggerated in primary hypothyroidism, major depression, cocaine dependence, amphetamine dependence and chronic phencyclidine abuse. There is a failure to suppress in the manic phase of bipolar disorder. [cite journal |author=Giannini AJ, Malone DA, Loiselle RH, Price WA |title=Blunting of TSH response to TRH in chronic cocaine and phencyclidine abusers |journal=J Clin Psychiatry |volume=48 |issue=1 |pages=25–6 |year=1987 |pmid=3100509 |doi= |url=]Ultrasound
Nodules of the thyroid may or may not be
cancer .Medical ultrasonography can help determine their nature because some of the characteristics of benign and malignant nodules differ. The main characteristics of a thyroid nodule on high frequency thyroid ultrasound are as follows:Ultrasonography is not always able to separate benign from malignant nodules with complete certainty. In suspicious cases, a tissue sample is often obtained by biopsy for microscopic examination.
Radioiodine scanning and uptake
Thyroid
scintigraphy , imaging of the thyroid with the aid of radioactive iodine, usuallyiodine-123 (123I), is performed in thenuclear medicine department of a hospital or clinic. Radioiodine collects in the thyroid gland before being excreted in the urine. While in the thyroid the radioactive emissions can be detected by a camera, producing a rough image of the shape (a "radiodine scan") and tissue activity (a "radioiodine uptake") of the thyroid gland.A normal radioiodine scan shows even uptake and activity throughout the gland. Irregularity can reflect an abnormally shaped or abnormally located gland, or it can indicate that a portion of the gland is overactive or underactive, different from the rest. For example, a nodule that is overactive ("hot") to the point of suppressing the activity of the rest of the gland is usually a
thyrotoxic adenoma , a surgically curable form of hyperthyroidism that is hardly ever malignant. In contrast, finding that a substantial section of the thyroid is inactive ("cold") may indicate an area of non-functioning tissue such as thyroid cancer.The amount of radioactivity can be counted as an indicator of the metabolic activity of the gland. A normal quantitation of radioiodine uptake demonstrates that about 8 to 35% of the administered dose can be detected in the thyroid 24 hours later. Overactivity or underactivity of the gland as may occur with hypothyroidism or hyperthyroidism is usually reflected in decreased or increased radioiodine uptake. Different patterns may occur with different causes of hypo- or hyperthyroidism.
Biopsy
A medical
biopsy refers to the obtaining of a tissue sample for examination under the microscope or other testing, usually to distinguish cancer from noncancerous conditions. Thyroid tissue may be obtained for biopsy byfine needle aspiration or bysurgery .Needle aspiration has the advantage of being a brief, safe, outpatient procedure that is safer and less expensive than surgery and does not leave a visible scar. Needle biopsies became widely used in the 1980s, but it was recognized that accuracy of identification of cancer was good but not perfect. The accuracy of the diagnosis depends on obtaining tissue from all of the suspicious areas of an abnormal thyroid gland. The reliability of needle aspiration is increased when sampling can be guided by ultrasound, and over the last 15 years, this has become the preferred method for thyroid biopsy in North America.
Treatment
Medical treatment
Levothyroxine is astereoisomer of thyroxine which is degraded much slower and can be administered once daily in patients with hypothyroidism.Graves' disease may be treated with the
thioamide drugspropylthiouracil ,carbimazole ormethimazole , or rarely withLugol's solution . Hyperthyroidism as well as thyroid tumors may be treated withradioactive iodine .Percutaneous Ethanol Injections, PEI, for therapy of recurrent thyroid cysts, and metastatic thyroid cancer lymph nodes, as an alternative to the usual surgical method.
urgery
Thyroid surgery is performed for a variety of reasons. A nodule or lobe of the thyroid is sometimes removed for
biopsy or for the presence of an autonomously functioning adenoma causinghyperthyroidism . A large majority of the thyroid may be removed, a "subtotal thyroidectomy", to treat the hyperthyroidism ofGraves' disease , or to remove agoitre that is unsightly or impinges on vital structures.A complete
thyroidectomy of the entire thyroid, including associatedlymph nodes , is the preferred treatment forthyroid cancer . Removal of the bulk of the thyroid gland usually produceshypothyroidism , unless the person takesthyroid hormone replacement. Consequently, individuals who have undergone a total thyroidectomy are typically placed on thyroid hormone replacement for the remainder of their lives. Higher than normal doses are often administered to prevent recurrence.If the thyroid gland must be removed surgically, care must be taken to avoid damage to adjacent structures, the
parathyroid gland s and therecurrent laryngeal nerve . Both are susceptible to accidental removal and/or injury during thyroid surgery. The parathyroid glands produceparathyroid hormone (PTH), a hormone needed to maintain adequate amounts of calcium in the blood. Removal results inhypoparathyroidism and a need for supplemental calcium andvitamin D each day. In the event the blood supply to any one of the parathyroid glands is endangered through surgery, the parathyroid gland(s) involved may be re-implanted in surrounding muscle tissue. The recurrent laryngeal nerves provide motor control for all external muscles of thelarynx except for thecricothyroid muscle , also runs along the posterior thyroid. Accidental laceration of either of the two or both recurrent laryngeal nerves may cause paralysis of thevocal cords and their associated muscles, changing the voice quality.Radioiodine therapy
Large goiters that cause symptoms, but do not harbor cancer, after evaluation, and biopsy of suspicious nodules can be treated by an alternative therapy with radioiodine. The iodine uptake can be high in countries with iodine deficiency, but low in iodine sufficient countries. The 1999 release of rhTSH thyrogen in the USA, can boost the uptakes to 50-60% allowing the therapy with iodine 131. The gland shrinks by 50-60%, but can cause hypothyroidism, and rarely pain syndrome cause by radiation thyroiditis that is short lived and treated by steroids.
History
There are several findings that evidence a great interest for thyroid disorders just in the Medieval Medical School of
Salerno (XII Century). Rogerius Salernitanus, the Salernitan surgeon and author of "Post mundi fabricam" (around 1180) was considered at that time the surgical text par excellence all over Europe. In the chapter "De bocio" of his magnum opus he describes several pharmacological and surgical cures, some of which nowadays are reappraised quite scientifically effective. [cite journal |author=Bifulco M, Cavallo P |title=Thyroidology in the medieval medical school of salerno |journal=Thyroid |volume=17 |issue=1 |pages=39–40 |year=2007 |pmid=17274747 |doi=10.1089/thy.2006.0277 |url=]In modern times, the thyroid was first identified by the anatomist Thomas Wharton (whose name is also
eponym ised inWharton's duct of the submandibular gland) in 1656. [WhoNamedIt|doctor|2046|Thomas Wharton]Thyroid hormone (or "thyroxin") was identified only in the 19th century.
=Additionalee also
*
Thymus
*Academy of Clinical Thyroidologists References
External links
* [http://www.thyroid.org American Thyroid Association] (Thyroid Information and professional organization)
* "Thyroid Gland"
* " [http://www.liebertonline.com/doi/pdf/10.1089/thy.2006.16.ft-1 "New Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer"] from the American Thyroid Association Taskforce.
* [http://www.thyroidmanager.org Thyroid Disease Manager] (free online textbook)
* [http://www.nucmedinfo.com/Pages/thyroid.html Thyroid Disease] (Nuclear Medicine Information)
* [http://www.allthyroid.org The Thyroid Foundation of America] (Education about Thyroid Disease)
Wikimedia Foundation. 2010.
