- Oocyte cryopreservation
-
Human oocyte cryopreservation (egg freezing) is a novel technology in which a woman’s eggs (oocytes) are extracted, frozen and stored. Later, when she is ready to become pregnant, the eggs can be thawed, fertilized, and transferred to the uterus as embryos.
Contents
History
Cryopreservation itself has always played a central role in assisted reproductive technology. With the first cryopreservation of sperm in 1953 and of embryos thirty years later, these techniques have become routine. Dr Christopher Chen of Australia reported the world’s first pregnancy in 1986 using previously frozen oocytes.[1] This report stood alone for several years followed by studies reporting success rates using frozen eggs to be much lower than those of traditional in vitro fertilization (IVF) techniques using fresh oocytes. Then recently, two articles published in the journal, Fertility and Sterility, reported pregnancy rates using frozen oocytes that were comparable to those of cryopreserved embryos and even fresh embryos.[2][3] These newer reports affirm that oocyte cryopreservation technology is advancing.
Indications
Oocyte cryopreservation is aimed at three particular groups of women: those diagnosed with cancer who have not yet begun chemotherapy or radiotherapy; those undergoing treatment with assisted reproductive technologies who do not consider embryo freezing an option; and those who would like to preserve their future ability to have children, either because they do not yet have a partner, or for other personal or medical reasons.
Over 50,000 reproductive-age women are diagnosed with cancer each year in the United States.[4] Chemotherapy and radiotherapy are toxic for oocytes, leaving few, if any, viable eggs. Egg freezing offers women with cancer the chance to preserve their eggs so that they can have children in the future.
Oocyte cryopreservation is an important option for individuals undergoing IVF who object, either for religious or ethical reasons, to the practice of freezing embryos. Having the option to fertilize only as many eggs as will be utilized in the IVF process, and then freeze any remaining unfertilized eggs can be a positive solution. In this way, there are no excess embryos created, and there need be no disposition of unused frozen embryos, a practice which can create complex choices for certain individuals.
Egg freezing can also be beneficial for women who, for the purpose of education, career or other reasons, desire to postpone childbearing. Freezing eggs at an early age may ensure a chance for a future pregnancy.
Additionally, women with a family history of early menopause have an interest in fertility preservation. With egg freezing, they will have a frozen store of eggs, in the likelihood that their eggs are depleted at an early age.
Method
The egg retrieval process for oocyte cryopreservation is the same as that for in vitro fertilization. This includes one to several weeks of hormone injections that stimulate ovaries to ripen multiple eggs. When the eggs are mature, a medication to trigger ovulation is given and the eggs are removed from the body using an ultrasound-guided needle through the vagina. The procedure is usually conducted under sedation. The eggs are immediately frozen.
The egg is the largest cell in the human body and contains a great amount of water. When the egg is frozen, the ice crystals that form can destroy the integrity of the cell. To prevent this, the egg must be dehydrated prior to freezing. This is done using cryoprotectants which replace the water within the cell and inhibit the formation of ice crystals.
Eggs (oocytes) are frozen using either a controlled-rate, slow-cooling method or a newer flash-freezing process known as vitrification. The slow-cooling method is the most practiced of embryo freezing techniques. Vitrification is much faster but requires higher concentrations of cryoprotectants to be added. The result of vitrification is a solid glass-like cell, free of ice crystals. There are differing schools of thought on which freezing method is theoretically superior for oocytes but large amounts of comparative data on the two methods is lacking at this time. With regard to slow freezing of embryos, a study involving 23 countries showed almost 42,000 'slow frozen' (as opposed to 'vitrified') human embryo transfers were performed during 2001 in Europe (Andersen et al. 2005). In addition, it is estimated that between 300,000 and 500,000 successful human births have resulted worldwide from the transfer of previously ‘slow frozen’ embryos performed from the mid-1970s to 2006.
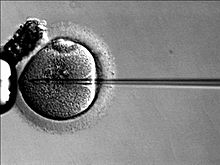
Once frozen, the zona pellucida, or shell of the egg hardens. Thus, currently, when eggs are thawed, a special fertilization procedure is performed by an embryologist whereby sperm is injected directly into the egg with a needle rather than allowing sperm to penetrate naturally by placing it around the egg in a dish. This injection technique is called ICSI (Intracytoplasmic Sperm Injection) and is also used in IVF.
Success rates
The percentage of transferred cycles is somewhat lower in frozen cycles compared with fresh cycles (approx. 80% and 90%, respectively).[5]
Two recent studies showed that the rate of birth defects and chromosomal defects when using cryopreserved oocytes is consistent with that of natural conception.[6][7]
Recent modifications in protocol regarding cryoprotectant composition, temperature and storage methods have had a large impact on the technology, and while it is still considered an experimental procedure, it is quickly becoming an option for women. Slow freezing traditionally has been the most commonly used method to cryopreserve oocytes, and is the method that has resulted in the most babies born from frozen oocytes worldwide. Ultra-rapid freezing or vitrification represents a potential alternative freezing method.
In the fall of 2009, The American Society for Reproductive Medicine (ASRM) issued an opinion on oocyte cryopreservation concluding that the science holds “great promise for applications in oocyte donation and fertility preservation” because recent laboratory modifications have resulted in improved oocyte survival, fertilization, and pregnancy rates from frozen-thawed oocytes in IVF.[8] The ASRM noted that from the limited research performed to date, there does not appear to be an increase in chromosomal abnormalities, birth defects, or developmental deficits in the children born from cryopreserved oocytes. The ASRM recommends that, pending further research, oocyte cryopreservation should be introduced into clinical practice on an investigational basis and under the guidance of an Institutional Review Board (IRB). As with any new technology, safety and efficacy must be evaluated and demonstrated through continued research.
Cost
The cost of egg freezing, (including the embryo transfer) is comparable to that of IVF and ranges from $12,000 to $20,000. Egg storage can be several hundred dollars or more per year.
See also
- Semen cryopreservation
- In vitro fertilization
References
- ^ Chen C. (1986) "Pregnancy after human oocyte cryopreservation". Lancet 1 (8486): 884-886. Retrieved on April 24, 2007
- ^ Jain, J. et al. (2005) "Oocyte cryopreservation". Fertility and Sterility 86 (4): 1037-1046. Retrieved on April 24, 2007
- ^ Grifo J and Noyes N. (2010) Delivery rate using cyropreserved oocytes is comparable to conventional in vitro fertilization using fresh oocytes: potential fertility preservation for female cancer patients. Fertility and Sterility 93:391-396.
- ^ American Cancer Society (2001) Cancer facts and figures 2001. Atlanta: American Cancer Society. Retrieved on April 24, 2007.
- ^ Magli MC, Lappi M, Ferraretti AP, Capoti A, Alessandra Ruberti, Gianaroli L (March 2009). "Impact of oocyte cryopreservation on embryo development". Fertil. Steril. 93 (2): 510–516. doi:10.1016/j.fertnstert.2009.01.148. PMID 19342025.
- ^ Noyes N, Porcu E, Borini A. (2009) With more than 900 babies born, live birth outcomes following oocyte cryopreservation do not appear different from those occurring after conventional IVF. Reprod Biomed Online 18:769-776.
- ^ CNN April 16, 2007 . Retrieved on April 24, 2007
- ^ ASRM Practice Committee. (2009) ASRM Practice Committee response to Rybak and Lieman: elective self-donation of oocytes. Fertil Steril 92:1513-514.
External links
- How egg freezing works, HFEA website
- World Association of Reproductive Medicine
- American Society for Reproductive Medicine
- Fertility and Sterility – The Official Journal of the American Society for Reproductive Medicine
- National Cancer Institute – Sexuality and Reproductive Issues
- Adventures in Egg Freezing – Informative blog by woman going through the elective egg freezing process
- My Egg Freezing Adventure! - Blog by a 35-year-old woman freezing her eggs in 2011 to preserve her fertility, after considering alternatives such as having a child on her own
- Harrison, K. et al. April 2, 2007. "Oocyte cryopreservation as an adjunct to the assisted reproductive technologies". The Medical Journal of Australia 186 (7): 379. A letter to the editor, in which the authors state that "oocyte cryopreservation may at last be coming of age." Retrieved on April 24, 2007.
- Gook, Debra A. and Edgar, David H. December, 1999. "Cryopreservation of the human female gamete: current and future issues". Oxford Journals 14 (12): 2938-2940. One of several important papers by Australian researcher, Debra Gook. Retrieved on April 24, 2007.
Categories:
Wikimedia Foundation. 2010.