- Ovarian follicle
-
Ovarian follicle 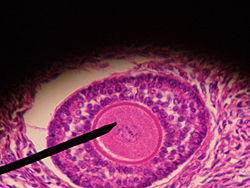
Human ovarian follicle Latin folliculi ovarici primarii, folliculi ovarici vesiculosi Gray's subject #266 1256 Precursor cortical cords MeSH Ovarian+Follicle Ovarian follicles are the basic units of female reproductive biology, each of which is composed of roughly spherical aggregations of cells found in the ovary. They contain a single oocyte (immature ovum or egg). These structures are periodically initiated to grow and develop, culminating in ovulation of usually a single competent oocyte in humans. These eggs/ova are only developed once every menstrual cycle (e.g. once a month in humans).
Contents
Structure
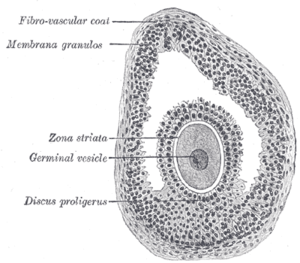
The cells of the ovarian follicle are the oocyte, granulosa cells and the cells of the internal and external theca layers.
Oocyte
Each month, one of the ovaries releases a mature egg, known as an oocyte. A follicle is an anatomical structure in which the primary oocyte develops. The nucleus of such an oocyte is called a germinal vesicle [1] (see picture).
Granulosa
Granulosa cells within the follicle surround the oocyte; their numbers increase directly in response to heightened levels of circulating gonadotropins or decrease in response to testosterone. They also produce peptides involved in ovarian hormone synthesis regulation. Follicle-stimulating hormone (FSH) induces granulosa cells to express luteinizing hormone (LH) receptors on their surfaces; when circulating LH binds to these receptors, proliferation stops.[2]
Thecal
The granulosa cells, in turn, are enclosed in a thin layer of extracellular matrix – the follicular basement membrane or basal lamina (fibro-vascular coat in picture). Outside the basal lamina, the layers theca interna and theca externa are found.
Development
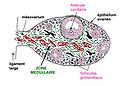
Main article: FolliculogenesisPrimordial follicles are indiscernible to the naked eye. However, these eventually develop into primary, secondary and tertiary vesicular follicles. Tertiary vesicular follicles (also called "mature vesicular follicles" or "ripe vesicular follicles") are sometimes called Graafian follicles (after Regnier de Graaf).
In humans, oocytes are established in the ovary before birth and may lie dormant awaiting initiation for up to 50 years.[3]
After rupturing, the follicle is turned into a corpus luteum.
Development of oocytes in ovarian follicles
Main article: OogenesisIn a larger perspective, the whole folliculogenesis from primordial to preovulatory follicle is located in the stage of meiosis I of ootidogenesis in oogenesis.
The embryonic development doesn't differ from the male one, but follows the common path before gametogenesis. Once gametogonia enter the gonadal ridge, however, they attempt to associate with these somatic cells. Development proceeds and the gametogonia turns into oogonia, which become fully surrounded by a layer of cells (pre-granulosa cells).
The Oogonia multiply by dividing mitotically; this proliferation ends when the oogonia enter meiosis. The amount of time that oogonia multiply by mitosis is not species specific. In the human fetus, cells undergoing mitosis are seen until the second and third trimester of pregnancy.[4][5] After beginning the meiotic process, the oogonia (now called primary oocytes) can no longer replicate. Therefore the total number of gametes is established at this time. Once the primary oocytes stop dividing the cells enter a prolonged ‘resting phase’. This ‘resting phase’ or dictyate stage can last anywhere up to fifty years in the human.
For several primary oocytes that undergoes meiosis, only one functional oocyte is produced. The other two or three cells produced are called polar bodies. Polar bodies have no function and eventually deteriorate.
The primary oocyte turns into a secondary oocyte in mature ovarian follicles. Unlike the sperm, the egg is arrested in the secondary stage of meiosis until fertilization.
Upon fertilization by sperm, the secondary oocyte continues the second part of meiosis and becomes a zygote.
Pathology
Any ovarian follicle that is larger than about two centimeters is termed an ovarian cyst.
Ovarian function may be measured by gynecologic ultrasonography of follicular volume. Nowadays, ovarian follicle volumes can be measured rapidly and automatically from three-dimensionally reconstructed ultrasound images.[6]
Rupture of the follicle can result in abdominal pain (mittelschmerz) and is to be considered in the differential diagnosis in women of childbearing age.[7]
Cryopreservation and culture
Follicles can develop from ovarian tissue after cryopreservation. Cryopreservation of ovarian tissue is of interest to women who want to preserve their reproductive function beyond the natural limit, or whose reproductive potential is threatened by cancer therapy,[8] for example in hematologic malignancies or breast cancer.[9]
For in vitro culture of follicles, there are various techniques to optimize the growth of follicles, including the use of defined media, growth factors and three-dimensional extracellular matrix support.[10] Molecular methods and immunoassay can evaluate stage of maturation and guide adequate differentiation.[10]
References
- ^ Biology-online
- ^ Katz: Comprehensive Gynecology, 5th ed.
- ^ McGee E. A., Hsueh A. J. (2000). "Initial and cyclic recruitment of ovarian follicles". Endocrine Reviews 21 (2): 200–14. doi:10.1210/er.21.2.200. PMID 10782364.
- ^ Baker, T. G. (1982). Oogenesis and ovulation. In "Book 1: Germ cells and fertilization" (C. R. Austin and R. V. Short, Eds.), pp. 17-45. Cambridge University Press, Cambridge.
- ^ Byskov, A. G., and Hoyer, P. E. (1988). Embryology of mammalian gonads and ducts. In "The physiology of reproduction" (E. Knobil and J. Neill, Eds.), pp. 265-302. Raven Press, Ltd, New York.
- ^ Salama S, Arbo E, Lamazou F, Levailllant JM, Frydman R, Fanchin R (April 2010). "Reproducibility and reliability of automated volumetric measurement of single preovulatory follicles using SonoAVC". Fertil. Steril. 93 (6): 2069–73. doi:10.1016/j.fertnstert.2008.12.115. PMID 19342038.
- ^ http://www.merck.com/mmpe/sec02/ch011/ch011b.html
- ^ Isachenko V, Lapidus I, Isachenko E, et al. (2009). "Human ovarian tissue vitrification versus conventional freezing: morphological, endocrinological, and molecular biological evaluation.". Reproduction 138 (2): 319–27. doi:10.1530/REP-09-0039. PMID 19439559.
- ^ Oktay K, Oktem O (November 2008). "Ovarian cryopreservation and transplantation for fertility preservation for medical indications: report of an ongoing experience". Fertil. Steril. 93 (3): 762–8. doi:10.1016/j.fertnstert.2008.10.006. PMID 19013568.
- ^ a b Smitz J, Dolmans MM, Donnez J, et al. (February 2010). "Current achievements and future research directions in ovarian tissue culture, in vitro follicle development and transplantation: implications for fertility preservation". Hum Reprod Update 16 (4): 395–414. doi:10.1093/humupd/dmp056. PMC 2880913. PMID 20124287. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2880913.
Additional images
External links
- SUNY Labs 43:05-0105 - "The Female Pelvis: The Ovary"
- Histology at BU 14803loa
- Slide at fda.gov
- Images at okstate.edu
- Life cycle at gfmer.ch
Female reproductive system (TA A09.1–2, TH H3.07.01, GA 11.1254) Internal AdnexaFolliclescorpus (hemorrhagicum, luteum, albicans) · Theca of follicle (externa, interna) · Follicular antrum (Follicular fluid) · Corona radiata · Zona pellucida · Membrana granulosa · Perivitelline spaceOtherProper of ovary · Suspensory of ovarycorpus/body (Uterine cavity, Fundus) · cervix/neck (External orifice, Canal of the cervix, Internal orifice, Supravaginal portion of cervix, Vaginal portion of cervix, Cervical ectropion) · Uterine hornsGeneralExternal Mons pubis · Labia majora (Anterior commissure, Posterior commissure) · Pudendal cleft · Labia minora (Frenulum of labia minora, Frenulum of clitoris) · Vulval vestibule · Interlabial sulci · Bulb of vestibule · Vaginal orifice
vestibular glands/ducts (Bartholin's glands/Bartholin's ducts, Skene's glands/Skene's ducts)Other Categories:- Female reproductive system
Wikimedia Foundation. 2010.