- Extracellular matrix
-
Extracellular matrix 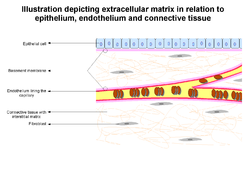
Illustration depicting extracellular matrix (basement membrane and interstitial matrix) in relation to epithelium, endothelium and connective tissue Latin matrix extracellularis Code TH H2.00.03.0.02001 In biology, the extracellular matrix (ECM) is the extracellular part of animal tissue that usually provides structural support to the animal cells in addition to performing various other important functions. The extracellular matrix is the defining feature of connective tissue in animals.
Extracellular matrix includes the interstitial matrix and the basement membrane.[1] Interstitial matrix is present between various animal cells (i.e., in the intercellular spaces). Gels of polysaccharides and fibrous proteins fill the interstitial space and act as a compression buffer against the stress placed on the ECM.[2] Basement membranes are sheet-like depositions of ECM on which various epithelial cells rest.
Contents
Role and importance
Due to its diverse nature and composition, the ECM can serve many functions, such as providing support, segregating tissues from one another, and regulating intercellular communication. The ECM regulates a cell's dynamic behavior. In addition, it sequesters a wide range of cellular growth factors, and acts as a local depot for them.[1] Changes in physiological conditions can trigger protease activities that cause local release of such depots. This allows the rapid and local growth factor-mediated activation of cellular functions, without de novo synthesis.
Formation of the extracellular matrix is essential for processes like growth, wound healing and fibrosis. An understanding of ECM structure and composition also helps in comprehending the complex dynamics of tumor invasion and metastasis in cancer biology[1] as metastasis often involves the destruction of extracellular matrix[3] by enzymes such as serine and threonine proteases and matrix metalloproteinases.[1]
Molecular components
Components of the ECM are produced intracellularly by resident cells, and secreted into the ECM via exocytosis.[4] Once secreted they then aggregate with the existing matrix. The ECM is composed of an interlocking mesh of fibrous proteins and glycosaminoglycans (GAGs).
Proteoglycans
GAGs are carbohydrate polymers and are usually attached to extracellular matrix proteins to form proteoglycans (hyaluronic acid is a notable exception, see below). Proteoglycans have a net negative charge that attracts positively charged sodium ions (Na+) which attracts water molecules via osmosis, keeping the ECM and resident cells hydrated. Proteoglycans may also help to trap and store growth factors within the ECM.
Described below are the different types of proteoglycan found within the extracellular matrix.
Heparan sulfate
Heparan sulfate (HS) is a linear polysaccharide found in all animal tissues. It occurs as a proteoglycan (PG) in which two or three HS chains are attached in close proximity to cell surface or extracellular matrix proteins.[5][6] It is in this form that HS binds to a variety of protein ligands and regulates a wide variety of biological activities, including developmental processes, angiogenesis, blood coagulation and tumour metastasis.
In the extracellular matrix, especially basement membranes, the multi-domain proteins perlecan, agrin and collagen XVIII are the main proteins to which heparan sulfate is attached.
Chondroitin sulfate
Chondroitin sulfates contribute to the tensile strength of cartilage, tendons, ligaments and walls of the aorta. They have also been known to affect neuroplasticity.[7]
Keratan sulfate
Keratan sulfates have a variable sulfate content and unlike many other GAGs, do not contain uronic acid. They are present in the cornea, cartilage, bones and the horns of animals.
Non-proteoglycan polysaccharide
Hyaluronic acid
Hyaluronic acid (or "hyaluronan") is a polysaccharide consisting of alternative residues of D-glucuronic acid and N-acetylglucosamine, and unlike other GAGs is not found as a proteoglycan. Hyaluronic acid in the extracellular space confers upon tissues the ability to resist compression by providing a counteracting turgor (swelling) force by absorbing significant amounts of water. Hyaluronic acid is thus found in abundance in the ECM of load-bearing joints. It is also a chief component of the interstitial gel. Hyaluronic acid is found on the inner surface of the cell membrane and is translocated out of the cell during biosynthesis.[8]
Hyaluronic acid acts as an environmental cue that regulates cell behavior during embryonic development, healing processes, inflammation and tumor development. It interacts with a specific transmembrane receptor, CD44.[9]
Fibers
Collagen
Collagens are, in most animals, the most abundant protein in the ECM. In fact, collagen is the most abundant protein in the human body[10][11] and accounts for 90% of bone matrix protein content.[12] Collagens are present in the ECM as fibrillar proteins and give structural support to resident cells. Collagen is exocytosed in precursor form (procollagen), which is then cleaved by procollagen proteases to allow extracellular assembly. Diseases such as osteogenesis imperfecta and epidermolysis bullosa are linked with genetic defects in collagen-encoding genes.[4] The collagen can be divided into several families according to the types of structure they form:
- Fibrillar (Type I,II,III,V,XI)
- Facit (Type IX,XII,XIV)
- Short chain (Type VIII,X)
- Basement membrane (Type IV)
- Other (Type VI,VII, XIII)
Elastin
Elastins, in contrast to collagens, give elasticity to tissues, allowing them to stretch when needed and then return to their original state. This is useful in blood vessels, the lungs, in skin, and the ligamentum nuchae, and these tissues contain high amounts of elastins. Elastins are synthesized by fibroblasts and smooth muscle cells. Elastins are highly insoluble, and tropoelastins are secreted inside a chaperone molecule, which releases the precursor molecule upon contact with a fiber of mature elastin. Tropoelastins are then deaminated to become incorporated into the elastin strand. Diseases such as cutis laxa and Williams syndrome are associated with deficient or absent elastin fibers in the ECM.[4]
Other
Fibronectin
Fibronectins are proteins that connect cells with collagen fibers in the ECM, allowing cells to move through the ECM. Fibronectins bind collagen and cell surface integrins, causing a reorganization of the cell's cytoskeleton and facilitating cell movement. Fibronectins are secreted by cells in an unfolded, inactive form. Binding to integrins unfolds fibronectin molecules, allowing them to form dimers so that they can function properly. Fibronectins also help at the site of tissue injury by binding to platelets during blood clotting and facilitating cell movement to the affected area during wound healing.[4]
Laminin
Laminins are proteins found in the basal laminae of virtually all animals. Rather than forming collagen-like fibers, laminins form networks of web-like structures that resist tensile forces in the basal lamina. They also assist in cell adhesion. Laminins bind other ECM components such as collagens, nidogens, and entactins.[4]
Cell adhesion to the ECM
Many cells bind to components of the extracellular matrix. Cell adhesion can occur in two ways; by focal adhesions, connecting the ECM to actin filaments of the cell, and hemidesmosomes, connecting the ECM to intermediate filaments such as keratin. This cell-to-ECM adhesion is regulated by specific cell surface cellular adhesion molecules (CAM) known as integrins. Integrins are cell surface proteins that bind cells to ECM structures, such as fibronectin and laminin, and also to integrin proteins on the surface of other cells.
Fibronectins bind to ECM macromolecules and facilitate their binding to transmembrane integrins. The attachment of fibronectin to the extracellular domain initiates intracellular signaling pathways as well as association with the cellular cytoskeleton via a set of adaptor molecules such as actin.[2]
Cell types involved in ECM formation
There are many cell types that contribute to the development of the various types of extracellular matrix found in plethora of tissue types. The local components of ECM determine the properties of the connective tissue.
Fibroblasts are the most common cell type in connective tissue ECM, in which they synthesize, maintain and provide a structural framework; fibroblasts secrete the precursor components of the ECM, including the ground substance. Chondrocytes are found in cartilage and produce the cartilagenous matrix. Osteoblasts are responsible for bone formation.
Extracellular matrix in plants
Plant cells are tessellated to form tissues. The cell wall is the relatively rigid structure surrounding the plant cell. The cell wall provides lateral strength to resist osmotic turgor pressure, but is flexible enough to allow cell growth when needed; it also serves as a medium for intercellular communication. The cell wall comprises multiple laminate layers of cellulose microfibrils embedded in a matrix of glycoproteins such as hemicellulose, pectin, and extensin. The components of the glycoprotein matrix help cell walls of adjacent plant cells to bind to each other. The selective permeability of the cell wall is chiefly governed by pectins in the glycoprotein matrix. Plasmodesmata (singular: plasmodesma) are pores that traverse the cell walls of adjacent plant cells. These channels are tightly regulated and selectively allow molecules of specific sizes to pass between cells.[8]
Medical Applications
Extracellular Matrix cells have been found to cause regrowth and healing of tissue. In human fetuses, for example, the extracellular matrix works with stem cells to grow and regrow all parts of the human body, and fetuses can regrow anything that gets damaged in the womb. Scientists have long believed that the matrix stops functioning after full development. It has been used in the past to help horses heal torn ligaments, but it is being researched further as a device for tissue regeneration in humans.[citation needed]
In terms of injury repair and tissue engineering, the extracellular matrix serves two main purposes. First, it prevents the immune system from triggering from the injury and responding with inflammation and scar tissue. Next, it facilitates the surrounding cells to repair the tissue instead of forming scar tissue.[citation needed]
For medical applications, the cells required are usually extracted from pig bladders, an easily accessible and relatively unused source. It is currently being used regularly to treat ulcers by closing the hole in the tissue that lines the stomach, but further research is currently being done by many universities as well as the U.S. Government for wounded soldier applications. As of early 2007, testing was being carried out on a military base in Texas. Scientists are using a powdered form on Iraq War veterans whose hands were damaged in the war.[13]
Not all ECM devices come from the bladder. Extracellular matrix coming from pig intestine has been used to repair "atrial septal defects" (ASD) and "patent foramen ovale" (PFO). After one year 95% of the collagen ECM in these patches is replaced by the normal soft tissue of the heart.[14]
References
- ^ a b c d Kumar; Abbas; Fausto. Robbins and Cotran: Pathologic Basis of Disease (7th ed.). Philadelphia: Elsevier. ISBN 0721601871.
- ^ a b Alberts B, Bray D, Hopin K, Johnson A, Lewis J, Raff M, Roberts K, Walter P (2004). "Tissues and Cancer". Essential cell biology. New York and London: Garland Science. ISBN 0-8153-3481-8.
- ^ Liotta LA, Tryggvason K, Garbisa S, Hart I, Foltz CM, Shafie S (1980). "Metastatic potential correlates with enzymatic degradation of basement membrane collagen". Nature 284 (5751): 67–8. doi:10.1038/284067a0. PMID 6243750. http://www.nature.com/nature/journal/v284/n5751/abs/284067a0.html.
- ^ a b c d e Plopper G (2007). The extracellular matrix and cell adhesion, in Cells (eds Lewin B, Cassimeris L, Lingappa V, Plopper G). Sudbury, MA: Jones and Bartlett. ISBN 0-7637-3905-7.
- ^ Gallagher, J.T., Lyon, M. (2000). "Molecular structure of Heparan Sulfate and interactions with growth factors and morphogens". In Iozzo, M, V.. Proteoglycans: structure, biology and molecular interactions. Marcel Dekker Inc. New York, New York. pp. 27–59.
- ^ Iozzo, R. V. (1998). "Matrix proteoglycans: from molecular design to cellular function". Annu. Rev. Biochem. 67: 609–652. doi:10.1146/annurev.biochem.67.1.609. PMID 9759499.
- ^ Hensch TK (2005). "Critical period mechanisms in developing visual cortex". Curr. Top. Dev. Biol. 69: 215–37. doi:10.1016/S0070-2153(05)69008-4. PMID 16243601. http://linkinghub.elsevier.com/retrieve/pii/S0070-2153(05)69008-4.
- ^ a b Lodish H, Berk A, Matsudaira P, Kaiser CA, Krieger M, Scott MP, Zipursky SL, Darnell J. "Integrating Cells Into Tissues". Molecular Cell Biology (5th ed.). New York: WH Freeman and Company. pp. 197–234.
- ^ Peach RJ, Hollenbaugh D, Stamenkovic I, Aruffo A (July 1993). "Identification of hyaluronic acid binding sites in the extracellular domain of CD44". J. Cell Biol. 122 (1): 257–64. doi:10.1083/jcb.122.1.257. PMC 2119597. PMID 8314845. http://www.jcb.org/cgi/pmidlookup?view=long&pmid=8314845.
- ^ Di Lullo GA, Sweeney SM, Korkko J, Ala-Kokko L, San Antonio JD (2002). "Mapping the ligand-binding sites and disease-associated mutations on the most abundant protein in the human, type I collagen". J. Biol. Chem. 277 (6): 4223–31. doi:10.1074/jbc.M110709200. PMID 11704682.
- ^ Karsenty G, Park RW (1995). "Regulation of type I collagen genes expression". Int. Rev. Immunol. 12 (2–4): 177–85. doi:10.3109/08830189509056711. PMID 7650420.
- ^ Kern B, Shen J, Starbuck M, Karsenty G (2001). "Cbfa1 contributes to the osteoblast-specific expression of type I collagen genes". J. Biol. Chem. 276 (10): 7101–7. doi:10.1074/jbc.M006215200. PMID 11106645.
- ^ HowStuffWorks, Humans Can Regrow Fingers? In 2009, the St. Francis Heart Center announced the use of the extracellular matrix technology in repair surgery.
- ^ "First Ever Implantation of Bioabsorbable Biostar Device at DHZB". DHZB NEWS. December 2007. http://www.dhzb.de/international_services/dhzb_aktuell/detail/ansicht/pressedetail/290/. Retrieved 2008-08-05. "The almost transparent collagen matrix consists of medically purified pig intestine, which is broken down by the scavenger cells (macrophages) of the immune system. After about 1 year the collagen has been almost completely (90-95%) replaced by normal body tissue: only the tiny metal framework remains. An entirely absorbable implant is currently under development."
External links
- MeSH Extracellular+matrix
- ANAT3231 Lecture 08 Extracellular Matrix - Lecture about extracellular matrix from UNSW Cell Biology website.
- Extracellular matrix: review of its roles in acute and chronic wounds
- Usage of Extracellular Matrix from pigs to regrow human extremities
- "The Extracellular Matrix of Animals", from Chapter 19 of The Molecular Biology of the Cell, 4th edition, Alberts et al.
- Biology, John W. Kimball. An online Biology textbook.
- [1], The man who grew a finger, By Matthew Price, BBC news
- Sound Medicine - Heart Tissue Regeneration - July 19 interview discussing ECM and its uses in cardiac tissue repair (requires MP3 playback).
- Growing Body Parts - A December 2009 report by 60 Minutes
Histology: connective tissue (TH H2.00.03) Composition ResidentExtracellular
matrix
(noncellular)Collagen fibers
Reticular fibers: COL3A1
Elastic fibers: Elastin · Fibrillin (FBN1, FBN2, FBN3) · EMILIN1
ElauninClassification LooseRelated see also Template:Soft tissue tumors and sarcomas
Extracellular matrix Fibril formingOtherFACIT: type IX (COL9A1, COL9A2, COL9A3) · type XII (COL12A1) · COL14A1 · COL16A1 · COL19A1 · COL20A1 · COL21A1 · COL22A1
basement membrane: type IV (COL4A1, COL4A2, COL4A3, COL4A4, COL4A5, COL4A6)
multiplexin: COL15A1 · type XVIII (COL18A1, Endostatin)
transmembrane: COL13A1 · COL17A1 · COL23A1 · COL25A1
other: type VI (COL6A1, COL6A2, COL6A3) · type VII (COL7A1) · type VIII (COL8A1, COL8A2) · type X (COL10A1) · type XI (COL11A1, COL11A2) · COL27A1 · COL28A1 · COL29A1OtherALCAM · Elastin (Tropoelastin) · Vitronectin · FRAS1 · FREM2 · Decorin · FAM20C · ECM1 · Matrix gla protein · Tectorin (TECTA, TECTB)Other see also diseases
B proteins: BY STRUCTURE: membrane, globular (en, ca, an), fibrousCategories:- Tissues
Wikimedia Foundation. 2010.
