- Osteoblast
-
Osteoblast 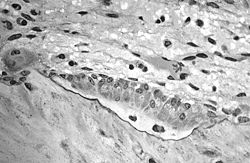
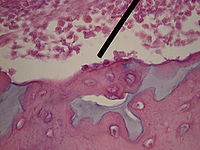
Osteoblasts actively synthesizing osteoid that contains two osteocytes. Latin osteoblastus Code TH H2.00.03.7.00002 Osteoblasts (from the Greek words for "bone" and "germ" or embryonic) are mononucleate cells that are responsible for bone formation; in essence, osteoblasts are specialized fibroblasts that in addition to fibroblastic products, express bone sialoprotein and osteocalcin.[1]
Osteoblasts produce a matrix of osteoid, which is composed mainly of Type I collagen. Osteoblasts are also responsible for mineralization of this matrix. Zinc, copper and sodium are some of the minerals required in this process. Bone is a dynamic tissue that is constantly being reshaped by osteoblasts, in charge of production of matrix and mineral, and osteoclasts, which remodel the tissue. Osteoblast cells tend to decrease with age, affecting the balance of formation and resorption in the bone tissue.[2]
Contents
Osteogenesis
Osteoblasts arise from osteoprogenitor cells located in the deeper layer of periosteum and the bone marrow. Osteoprogenitors are immature progenitor cells that express the master regulatory transcription factor Cbfa1/Runx2.
Osteoprogenitors are induced to differentiate under the influence of growth factors, in particular the bone morphogenetic proteins (BMPs).[3] Aside from BMPs, other growth factors including fibroblast growth factor (FGF),[3] platelet-derived growth factor (PDGF) and transforming growth factor beta (TGF-β) may promote the division of osteoprogenitors and potentially increase osteogenesis.
Once osteoprogenitors start to differentiate into osteoblasts, they begin to express a range of genetic markers including Osterix, Col1,[4] BSP, M-CSF, ALP,[5] osteocalcin,[4] osteopontin, and osteonectin. Although the term osteoblast implies an immature cell type, osteoblasts are in fact the mature bone cells entirely responsible for generating bone tissue in animals and humans.
Morphology and histological staining
Hematoxylin and eosin staining reveals that the cytoplasm of osteoblasts is basophilic due to the presence of a large amount of rough endoplasmic reticulum. A large Golgi apparatus is also present in the centre. The nucleus is spherical and large. Active osteoblasts synthesize, and stain positively for, Type-I collagen and alkaline phosphatase.
Osteoblasts and osteocytes
Osteoblasts that become trapped in the bone matrix and remain isolated in lacunae become osteocytes. They cease to generate osteoid and mineralized matrix, and instead act in a paracrine manner on active osteoblasts. They are believed to respond to mechanosensory stimuli.[6][7]
See also
References
- ^ Salentijn, L. Biology of Mineralized Tissues: Cartilage and Bone, Columbia University College of Dental Medicine post-graduate dental lecture series, 2007
- ^ D’ippolito, Gianluca; Schiller, Paul C.; Ricordi, Camillo; Roos, Bernard A.; Howard, Guy A. (1999). "Age-Related Osteogenic Potential of Mesenchymal Stromal Stem Cells from Human Vertebral Bone Marrow". Journal of Bone and Mineral Research 14 (7): 1115–1122. doi:10.1359/jbmr.1999.14.7.1115. PMID 10404011.
- ^ a b Agata, H; Asahina, I; Yamazaki, Y; Uchida, M; Shinohara, Y; Honda, MJ; Kagami, H; Ueda, M (2007). "Effective bone engineering with periosteum-derived cells.". Journal of dental research 86 (1): 79–83. doi:10.1177/154405910708600113. PMID 17189468.
- ^ a b Ringe, J; Leinhase, I; Stich, S; Loch, A; Neumann, K; Haisch, A; Häupl, T; Manz, R et al. (2008). "Human mastoid periosteum-derived stem cells: promising candidates for skeletal tissue engineering.". Journal of tissue engineering and regenerative medicine 2 (2-3): 136–46. doi:10.1002/term.75. PMID 18383554.
- ^ Szulc, P; Garnero, P; Marchand, F; Duboeuf, F; Delmas, PD (2005). "Biochemical markers of bone formation reflect endosteal bone loss in elderly men--MINOS study.". Bone 36 (1): 13–21. doi:10.1016/j.bone.2004.09.004. PMID 15663998.
- ^ Ehrlich, P. J.; Lanyon, L. E. (2002). "Mechanical Strain and Bone Cell Function: A Review". Osteoporosis International 13 (9): 688–700. doi:10.1007/s001980200095. PMID 12195532.
- ^ You, J.; Yellowley, C. E.; Donahue, H. J.; Zhang, Y.; Chen, Q.; Jacobs, C. R. (2000). "Substrate Deformation Levels Associated With Routine Physical Activity Are Less Stimulatory to Bone Cells Relative to Loading-Induced Oscillatory Fluid Flow". Journal of Biomechanical Engineering 122 (4): 387–394. doi:10.1115/1.1287161. PMID 11036562.
Further reading
- Netter, Frank H. (1987). Musculoskeletal system: anatomy, physiology, and metabolic disorders. Summit, New Jersey: Ciba-Geigy Corporation ISBN 0914168886.
External links
Musculoskeletal system · connective tissue: bone and cartilage (TA A02.0, TH H3.01, GA 2.86–95) Cartilage perichondrium · fibrocartilage callus · metaphysis
cells (chondroblast · chondrocyte)
types (hyaline · elastic · fibrous)Bone CycleTypesRegionsStructureosteon / Haversian system · Haversian canals · Volkmann's canals · connective tissue (endosteum · periosteum) · Sharpey's fibres · enthesis · lacunae · canaliculi · trabeculae · medullary cavity · bone marrowShapesHuman cell types / list derived primarily from mesoderm Paraxial muscle: Myoblast → Myocyte · Myosatellite cell · Tendon cell · Cardiac muscle cell
adipose: Lipoblast → AdipocyteDigestive systemIntermediate Urinary system (RSC)Angioblast → Endothelial cell · Mesangial cell (Intraglomerular, Extraglomerular) · Juxtaglomerular cell · Macula densa cell
Stromal cell → Interstitial cell → Telocytes
Simple epithelial cell → Podocyte · Kidney proximal tubule brush border cellLateral plate/
hemangioblastsee lymphocytessee myeloid cellsCategories:- Skeletal system
- Connective tissue cells
- Human cells
Wikimedia Foundation. 2010.