- Luteinizing hormone
-
Luteinizing hormone beta polypeptide Identifiers Symbol LHB Entrez 3972 HUGO 6584 OMIM 152780 RefSeq NM_000894 UniProt P01229 Other data Locus Chr. 19 q13.3 Luteinizing hormone (LH, also known as lutropin[1]) is a hormone produced by the anterior pituitary gland. In females, an acute rise of LH called the LH surge triggers ovulation[2] and development of the corpus luteum. In males, where LH had also been called interstitial cell-stimulating hormone (ICSH),[3] it stimulates Leydig cell production of testosterone.[4] It acts synergistically with FSH.
Contents
Structure
LH is a heterodimeric glycoprotein. Each monomeric unit is a glycoprotein molecule; one alpha and one beta subunit make the full, functional protein.
Its structure is similar to that of the other glycoprotein hormones, follicle-stimulating hormone (FSH), thyroid-stimulating hormone (TSH), and human chorionic gonadotropin (hCG). The protein dimer contains 2 glycopeptidic subunits, labeled alpha and beta subunits, that are non-covalently associated (i.e., without any disulfide bridge linking them):
- The alpha subunits of LH, FSH, TSH, and hCG are identical, and contain 92 amino acids in human but 96 amino acids in almost all other vertebrate species (glycoprotein hormones do not exist in invertebrates).
The 92-amino acid long LH alpha subunit in humans has the following sequence:
NH2 – Ala – Pro – Asp – Val – Gln – Asp – Cys – Pro – Glu – Cys – Thr – Leu – Gln – Glu – Asn – Pro – Phe – Phe – Ser – Gln – Pro – Gly – Ala – Pro – Ile – Leu – Gln – Cys – Met – Gly – Cys – Cys – Phe – Ser – Arg – Ala – Tyr – Pro – Thr – Pro – Leu – Arg – Ser – Lys – Lys – Thr – Met – Leu – Val – Gln – Lys – Asn – Val – Thr – Ser – Glu – Ser – Thr – Cys – Cys – Val – Ala – Lys – Ser – Tyr – Asn – Arg – Val – Thr – Val – Met – Gly – Gly – Phe – Lys – Val – Glu – Asn – His – Thr – Ala – Cys – His – Cys – Ser – Thr – Cys – Tyr – Tyr – His – Lys – Ser – OH
- Note: The carbohydrate moiety is linked to the asparagine at positions 52 and 78.
- The beta subunits vary. LH has a beta subunit of 120 amino acids (LHB) that confers its specific biologic action and is responsible for the specificity of the interaction with the LH receptor. This beta subunit contains an amino acid sequence that exhibits large homologies with that of the beta subunit of hCG and both stimulate the same receptor. However, the hCG beta subunit contains an additional 24 amino acids, and the two hormones differ in the composition of their sugar moieties.
NH2 – Ser – Arg – Glu – Pro – Leu – Arg – Pro – Trp – Cys – His – Pro – Ile – Asn – Ala – Ile – Leu – Ala – Val – Glu – Lys – Glu – Gly – Cys – Pro – Val – Cys – Ile – Thr – Val – AsnThr – Thr – Ile – Cys – Ala – Gly – Tyr – Cys – Pro – Thr – Met – Met – Arg – Val – Leu – Gln – Ala – Val – Leu – Pro – Pro – Leu – Pro – Gln – Val – Val – Cys – Thr – Tyr – Arg – Asp – Val – Arg – Phe – Glu – Ser – Ile – Arg – Leu – Pro – Gly – Cys – Pro – Arg – Gly – Val – Asp – Pro – Val – Val – Ser – Phe – Pro – Val – Ala – Leu – Ser – Cys – Arg – Cys – Gly – Pro – Cys – Arg – Arg – Ser – Thr – Ser – Asp – Cys – Gly – Gly – Pro – Lys – Asp – His – Pro – Leu – Thr – Cys – Asp – His – Pro – Gln – Leu – Ser – Gly – Leu – Leu – Phe – Leu – OH
The different composition of these oligosaccharides affects bioactivity and speed of degradation. The biologic half-life of LH is 20 minutes, shorter than that of FSH (3–4 hours) and hCG (24 hours).[citation needed]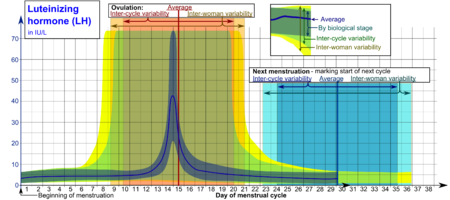 Reference ranges for the blood content of luteinizing hormone (LH) during the menstrual cycle. [5]
Reference ranges for the blood content of luteinizing hormone (LH) during the menstrual cycle. [5]
- The ranges denoted By biological stage may be used in closely monitored menstrual cycles in regard to other markers of its biological progression, with the time scale being compressed or stretched to how much faster or slower, respectively, the cycle progresses compared to an average cycle.
- The ranges denoted Inter-cycle variability are more appropriate to use in non-monitored cycles with only the beginning of menstruation known, but where the woman accurately knows her average cycle lengths and time of ovulation, and that they are somewhat averagely regular, with the time scale being compressed or stretched to how much a woman's average cycle length is shorter or longer, respectively, than the average of the population.
- The ranges denoted Inter-woman variability are more appropriate to use when the average cycle lengths and time of ovulation are unknown, but only the beginning of menstruation is given.Genes
The gene for the alpha subunit is located on chromosome 6q12.21.
The luteinizing hormone beta subunit gene is localized in the LHB/CGB gene cluster on chromosome 19q13.32. In contrast to the alpha gene activity, beta LH subunit gene activity is restricted to the pituitary gonadotropic cells. It is regulated by the gonadotropin-releasing hormone from the hypothalamus. Inhibin, activin, and sex hormones do not affect genetic activity for the beta subunit production of LH.
Activity
In both males and females, LH is essential for reproduction.
- In females, at the time of menstruation, FSH initiates follicular growth, specifically affecting granulosa cells.[6] With the rise in oestrogens, LH receptors are also expressed on the maturing follicle that produces an increasing amount of estradiol. Eventually at the time of the maturation of the follicle, the oestrogen rise leads via the hypothalamic interface to the “positive feed-back” effect, a release of LH over a 24- to 48-hour period. This 'LH surge' triggers ovulation, thereby not only releasing the egg but also initiating the conversion of the residual follicle into a corpus luteum that, in turn, produces progesterone to prepare the endometrium for a possible implantation. LH is necessary to maintain luteal function for the first two weeks. In case of a pregnancy, luteal function will be further maintained by the action of hCG (a hormone very similar to LH) from the newly established pregnancy. LH supports theca cells in the ovary that provide androgens and hormonal precursors for estradiol production.
- In the male, LH acts upon the Leydig cells of the testis and is responsible for the production of testosterone, an androgen that exerts both endocrine activity and intratesticular activity on spermatogenesis.
The release of LH at the pituitary gland is controlled by pulses of gonadotropin-releasing hormone (GnRH) from the hypothalamus. Those pulses, in turn, are subject to the oestrogen feedback from the gonads.
Normal levels
LH levels are normally low during childhood and, in women, high after menopause. As LH is secreted as pulses, it is necessary to follow its concentration over a sufficient period of time to get a proper information about its blood level.
During the reproductive years, typical levels are between 1-20 IU/L. Physiologic high LH levels are seen during the LH surge (v.s.); typically they last 48 hours.
Ovulation predictor kit (LH kit)
The detection of the Luteinising hormone surge indicates impending ovulation. LH can be detected by urinary ovulation predictor kits (OPK, also LH-kit) that are performed, typically daily, around the time ovulation may be expected.[7] The conversion from a negative to a positive reading would suggest that ovulation is about to occur within 24–48 hours, giving women two days to engage in sexual intercourse or artificial insemination with the intentions of conceiving.[8]
Tests may be read manually using a colour-change paper strip, or digitally with the assistance of reading electronics.
Tests for Luteinising hormone may be combined with testing for estradiol in tests such as the Clearblue fertility monitor.[9]
The sensitivity of LH tests are measured in milli international unit, with tests commonly available in the range 10-40 m.i.u.[citation needed]
As sperm can stay viable in the woman for several days, LH tests are not recommended for contraceptive practices, as the LH surge typically occurs after the beginning of the fertile window. [note: photo shows "negative" results in the top strip, i.e., no LH surge, and "positive" results in the bottom strip. *This information needs editing. An LH surge will cause the test line (on the left) to be darker in colour than the strip on the right (depending on the brand you buy; follow package insert instructions for interpreting results). Women with PCOS may have LH in their urine throughout their cycle, causing their tests to appear coloured throughout the cycle as displayed in the bottom strip. ]
Disease states
Relative elevations
In children with precocious puberty of pituitary or central origin, LH and FSH levels may be in the reproductive range instead of the low levels typical for their age.
During the reproductive years, relatively elevated LH is frequently seen in patients with the polycystic ovary syndrome; however, it would be unusual for them to have LH levels outside of the normal reproductive range.
High LH levels
Persistently high LH levels are indicative of situations where the normal restricting feedback from the gonad is absent, leading to a pituitary production of both LH and FSH. While this is typical in the menopause, it is abnormal in the reproductive years. There it may be a sign of:
- Premature menopause
- Gonadal dysgenesis, Turner syndrome
- Castration
- Swyer syndrome
- Polycystic Ovary Syndrome
- Certain forms of Congenital adrenal hyperplasia
- Testicular failure
Deficient LH activity
Diminished secretion of LH can result in failure of gonadal function (hypogonadism). This condition is typically manifest in males as failure in production of normal numbers of sperm. In females, amenorrhea is commonly observed. Conditions with very low LH secretions are:
- Kallmann syndrome
- Hypothalamic suppression
- Hypopituitarism
- Eating disorder
- Female athlete triad
- Hyperprolactinemia
- Gonadotropin deficiency
- Gonadal suppression therapy
- GnRH antagonist
- GnRH agonist (downregulation)
Availability
LH is available mixed with FSH in the form of Pergonal, and other forms of urinary gonadotropins . More purified forms of urinary gonadotropins may reduce the LH portion in relation to FSH. Recombinant LH is available as lutropin alfa (Luveris).[10] [11] [12]All these medications have to be given parenterally. They are commonly used in infertility therapy to stimulate follicular development, the notable one being in IVF therapy.
Often, hCG medication is used as an LH substitute because it activates the same receptor. Medically used hCG is derived from urine of pregnant women, is less costly, and has a longer half-life than LH.
References
- ^ lutropin at eMedicine Dictionary
- ^ Physiology at MCG 5/5ch9/s5ch9_5
- ^ Louvet J, Harman S, Ross G (1975). "Effects of human chorionic gonadotropin, human interstitial cell stimulating hormone and human follicle-stimulating hormone on ovarian weights in estrogen-primed hypophysectomized immature female rats". Endocrinology 96 (5): 1179–86. doi:10.1210/endo-96-5-1179. PMID 1122882.
- ^ Physiology at MCG 5/5ch8/s5ch8_5
- ^ References and further description of values are given in image page in Wikimedia Commons at Commons:File:Luteinizing hormone (LH) during menstrual cycle.png.
- ^ Gonadotropins: Luteinizing and Follicle Stimulating Hormones at colostate.edu
- ^ Nielsen M, Barton S, Hatasaka H, Stanford J (2001). "Comparison of several one-step home urinary luteinizing hormone detection test kits to OvuQuick". Fertil Steril 76 (2): 384–7. doi:10.1016/S0015-0282(01)01881-7. PMID 11476792.
- ^ Ovulation Predictor Kit information at pinelandpress.com
- ^ "Clearblue website". http://www.clearblue.com/uk/HCP/faq.php. Retrieved 2009-08-11.
- ^ Luveris information
- ^ Luveris®; http://www.emdserono.com/cmg.emdserono_us/en/images/Luveris_tcm115_19351.pdf
- ^ Luveritis, Administration and storage info, http://www.txfertility.com/forms/Luveris%20instructions.pdf
External links
Endocrine system: hormones (Peptide hormones · Steroid hormones) Endocrine
glandsTestis: testosterone · AMH · inhibin
Ovary: estradiol · progesterone · activin and inhibin · relaxin (pregnancy)
Placenta: hCG · HPL · estrogen · progesteroneIslet-Acinar
AxisNon-end.
glandsThymus: Thymosin (Thymosin α1, Thymosin beta) · Thymopoietin · Thymulin
Digestive system: Stomach: gastrin · ghrelin · Duodenum: CCK · GIP · secretin · motilin · VIP · Ileum: enteroglucagon · peptide YY · Liver/other: Insulin-like growth factor (IGF-1, IGF-2)
Adipose tissue: leptin · adiponectin · resistin
Kidney: JGA (renin) · peritubular cells (EPO) · calcitriol · prostaglandin
Heart: Natriuretic peptide (ANP, BNP)Categories:- Genes on chromosome 19
- Recombinant proteins
- Glycoproteins
- Peptide hormones
- Sex hormones
- Human hormones
- Hormones of the hypothalamus-pituitary-gonad axis
- Anterior pituitary hormones
Wikimedia Foundation. 2010.

