- Cortisol
-
Cortisol 
Systematic (IUPAC) name (11β)-11,17,21-trihydroxypregn-4-ene-3,20-dione Clinical data Pregnancy cat. C Legal status Rx Only (U.S.) (excluding 1-2% strength topical) Routes Oral tablets, intravenously, topical Identifiers CAS number 50-23-7 
ATC code H02AB09 (and others) PubChem CID 5754 DrugBank DB07886 ChemSpider 5551 
UNII WI4X0X7BPJ 
KEGG D00088 
ChEBI CHEBI:17650 
ChEMBL CHEMBL389621 
Chemical data Formula C21H30O5 Mol. mass 362.460 SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Cortisol (hydrocortisone) is a steroid hormone, or glucocorticoid, produced by the adrenal gland.[1] It is released in response to stress and a low level of blood glucocorticoids. Its primary functions are to increase blood sugar through gluconeogenesis; suppress the immune system; and aid in fat, protein and carbohydrate metabolism.[2] It also decreases bone formation. During pregnancy, increased production of cortisol between weeks 30-32 initiates production of fetal lung surfactant to promote maturation of the lungs. Various synthetic forms of cortisol are used to treat a variety of diseases.
Contents
Physiology
Production and release
Cortisol is produced by the adrenal gland in the zona fasciculata, the second of three layers comprising the outer adrenal cortex. This release is controlled by the hypothalamus, a part of the brain. The secretion of corticotropin-releasing hormone (CRH) by the hypothalamus triggers anterior pituitary secretion of adrenocorticotropic hormone (ACTH). ACTH is carried by the blood to the adrenal cortex, where it triggers glucocorticoid secretion.
Main functions in the body
- increasing blood sugar through gluconeogenesis
- suppressing the immune system
- aiding in fat, protein, and carbohydrate metabolism
It suppresses the immune system by "muting" the white blood cells
Another function is to decrease bone formation. Cortisol is used to treat diseases such as Addison’s disease, inflammatory and rheumatoid diseases, and allergies. Low-potency hydrocortisone, available over the counter in some countries, is used to treat skin problems such as rashes, eczema and others.
Cortisol prevents the release of substances in the body that cause inflammation. It stimulates gluconeogenesis (the breakdown of protein and fat to provide metabolites that can be converted to glucose in the liver) and it activates anti-stress and anti-inflammatory pathways.[3]
Patterns
The amount of cortisol present in the blood undergoes diurnal variation; the level peaks in the early morning (approximately 8 am) and reaches its lowest level at about midnight-4 am, or three to five hours after the onset of sleep. Information about the light/dark cycle is transmitted from the retina to the paired suprachiasmatic nuclei in the hypothalamus. This pattern is not present at birth; estimates of when it begins vary from two weeks to nine months of age.[4]
Changed patterns of serum cortisol levels have been observed in connection with abnormal ACTH levels, clinical depression, psychological stress, and physiological stressors such as hypoglycemia, illness, fever, trauma, surgery, fear, pain, physical exertion, or temperature extremes. Cortisol levels may also differ for individuals with autism or Asperger's syndrome.[5]
There is also significant individual variation, although a given person tends to have consistent rhythms.
Normal levels
Reference ranges for blood plasma content of free cortisol Time Lower limit Upper limit Unit 09:00 am 140[6] 700[6] nmol/L 5[7] 25[7] μg/dL Midnight 80[6] 350[6] nmol/L 2.9[7] 13[7] μg/dL Using the molecular weight of 362.460 g/mole, the conversion factor from µg/dl to nmol/L is approximately 27.6; thus, 10 µg/dl is approximately equal to 276 nmol/L.
Reference ranges for urinalysis of free cortisol Lower limit Upper limit Unit 28[8] or 30[9] 280[8] or 490[9] nmol/24h 10[10] or 11[11] 100[10] or 176[11] µg/24h A urinary value smaller than 200 nmol/24h (72 µg/24h[11]) strongly indicates absence of Cushing's syndrome.[9]
Effects
Cortisol is released in response to stress, acting to restore homeostasis. However, prolonged cortisol secretion (which may be due to chronic stress or the excessive secretion seen in Cushing's syndrome) results in significant physiological changes.[12]
- Insulin
Cortisol counteracts insulin, contributes to hyperglycemia-causing hepatic gluconeogenesis[13] and inhibits the peripheral utilization of glucose (insulin resistance) [13] by decreasing the translocation of glucose transporters (especially GLUT4) to the cell membrane.[14][15] However, cortisol increases glycogen synthesis (glycogenesis) in the liver.[16] The permissive effect of cortisol on insulin action in liver glycogenesis is observed in hepatocyte culture in the laboratory, although the mechanism for this is unknown.
- Collagen
In laboratory rats, cortisol-induced collagen loss in the skin is ten times greater than in any other tissue.[17][18] Cortisol (as opticortinol) may inversely inhibit IgA precursor cells in the intestines of calves.[19] Cortisol also inhibits IgA in serum, as it does IgM; however, it is not shown to inhibit IgE.[20]
- Gastric and renal secretion
Cortisol stimulates gastric-acid secretion.[21] Cortisol's only direct effect on the hydrogen ion excretion of the kidneys is to stimulate the excretion of ammonium ions by deactivating the renal glutaminase enzyme.[22] Net chloride secretion in the intestines is inversely decreased by cortisol in vitro (methylprednisolone).[23][disambiguation needed
 ]
]- Sodium
Cortisol inhibits sodium loss through the small intestine of mammals.[24] Sodium depletion, however, does not affect cortisol levels[25] so cortisol cannot be used to regulate serum sodium. Cortisol's original purpose may have been sodium transport. This hypothesis is supported by the fact that freshwater fish utilize cortisol to stimulate sodium inward, while saltwater fish have a cortisol-based system for expelling excess sodium.[26]
- Potassium
A sodium load augments the intense potassium excretion by cortisol; corticosterone is comparable to cortisol in this case.[27] In order for potassium to move out of the cell, cortisol moves an equal number of sodium ions into the cell.[28] This should make pH regulation much easier (unlike the normal potassium-deficiency situation, in which two sodium ions move in for each three potassium ions that move out—closer to the deoxycorticosterone effect). Nevertheless, cortisol consistently causes serum alkalosis; in a deficiency, serum pH does not change. The purpose of this may be to reduce serum pH to an optimum value for some immune enzymes during infection, when cortisol declines. Potassium is also blocked from loss in the kidneys by a decline in cortisol (9 alpha fluorohydrocortisone).[29]
- Water
Cortisol acts as a diuretic hormone, controlling one-half of intestinal diuresis;[24] it has also been shown to control kidney diuresis in dogs. The decline in water excretion following a decline in cortisol (dexamethasone) in dogs is probably due to inverse stimulation of antidiuretic hormone (ADH or arginine vasopressin), which is not overridden by water loading.[30] Humans and other animals also use this mechanism.[31]
- Copper
Cortisol stimulates many copper enzymes (often to 50% of their total potential), probably to increase copper availability for immune purposes.[32] This includes lysyl oxidase, an enzyme which is used to cross-link collagen and elastin.[33] Especially valuable for immune response is cortisol's stimulation of the superoxide dismutase,[34] since this copper enzyme is almost certainly used by the body to permit superoxides to poison bacteria. Cortisol causes an inverse four- or fivefold decrease of metallothionein (a copper storage protein) in mice;[35] however, rodents do not synthesize cortisol themselves. This may be to furnish more copper for ceruloplasmin synthesis or to release free copper. Cortisol has an opposite effect on aminoisobuteric acid than on the other amino acids.[36] If alpha-aminoisobuteric acid is used to transport copper through the cell wall, this anomaly might be explained.
- Immune system
Cortisol can weaken the activity of the immune system. Cortisol prevents proliferation of T-cells by rendering the interleukin-2 producer T-cells unresponsive to interleukin-1 (IL-1), and unable to produce the T-cell growth factor.[37] Cortisol also has a negative-feedback effect on interleukin-1.[38] IL-1 must be especially useful in combating some diseases; however, endotoxic bacteria have gained an advantage by forcing the hypothalamus to increase cortisol levels (forcing the secretion of CRH hormone, thus antagonizing IL-1). The suppressor cells are not affected by glucosteroid response-modifying factor (GRMF),[39] so the effective setpoint for the immune cells may be even higher than the setpoint for physiological processes (reflecting leukocyte redistribution to lymph nodes, bone marrow, and skin). Rapid administration of corticosterone (the endogenous Type I and Type II receptor agonist) or RU28362 (a specific Type II receptor agonist) to adrenalectomized animals induced changes in leukocyte distribution. Natural killer cells are not affected by cortisol.[40]
- Bone metabolism
Cortisol reduces bone formation, favoring long-term development of osteoporosis. It transports potassium out of cells in exchange for an equal number of sodium ions (see above).[41] This can trigger the hyperkalemia of metabolic shock from surgery. Cortisol also reduces calcium absorption in the intestine.[42]
- Memory
Cortisol works with epinephrine (adrenaline) to create memories of short-term emotional events; this is the proposed mechanism for storage of flash bulb memories, and may originate as a means to remember what to avoid in the future. However, long-term exposure to cortisol damages cells in the hippocampus;[43] this damage results in impaired learning. Furthermore, it has been shown that cortisol inhibits memory retrieval of already stored information.[44][45]
- Additional effects
- Increases blood pressure by increasing the sensitivity of the vasculature to epinephrine and norepinephrine; in the absence of cortisol, widespread vasodilation occurs[citation needed]
- Inhibits secretion of corticotropin-releasing hormone (CRH), resulting in feedback inhibition of ACTH (Adrenocorticotropic hormone or corticotropin) secretion. Some researchers believe that this normal feedback system may become dysregulated when animals are exposed to chronic stress[citation needed]
- Causes the kidneys to produce hypotonic urine[citation needed]
- Shuts down the reproductive system, resulting in an increased chance of miscarriage and (in some cases) temporary infertility. Fertility returns after cortisol levels return to normal[46]
- Has anti-inflammatory properties, reducing histamine secretion and stabilizing lysosomal membranes. Stabilization of lysosomal membranes prevents their rupture, preventing damage to healthy tissues[citation needed]
- Stimulates hepatic detoxification by inducing tryptophan oxygenase (reducing serotonin levels in the brain), glutamine synthase (reducing glutamate and ammonia levels in the brain), cytochrome P-450 hemoprotein (mobilizing arachidonic acid), and metallothionein (reducing heavy metals in the body)[citation needed]
- In addition to cortisol's effects in binding to the glucocorticoid receptor, because of its molecular similarity to aldosterone it also binds to the mineralocorticoid receptor. Aldosterone and cortisol have a similar affinity for the mineralocorticoid receptor; however, glucocorticoids circulate at roughly 100 times the level of mineralocorticoids. An enzyme exists in mineralocorticoid target tissues to prevent overstimulation by glucocorticoids and allow selective mineralocorticoid action. This enzyme—11-beta hydroxysteroid dehydrogenase type II (Protein:HSD11B2)—catalyzes the deactivation of glucocorticoids to 11-dehydro metabolites[citation needed]
- There are potential links between cortisol, appetite and obesity.[47]
Binding
Most serum cortisol (all but about 4%) is bound to proteins, including corticosteroid binding globulin (CBG) and serum albumin. Free cortisol passes easily through cellular membranes, where they bind intracellular cortisol receptors.[48]
Regulation
The primary control of cortisol is the pituitary gland peptide, adrenocorticotropic hormone (ACTH). ACTH probably controls cortisol by controlling the movement of calcium into the cortisol-secreting target cells.[49] ACTH is in turn controlled by the hypothalamic peptide corticotropin releasing hormone (CRH), which is under nervous control. CRH acts synergistically with arginine vasopressin, angiotensin II, and epinephrine.[50] When activated macrophages start to secrete interleukin-1 (IL-1), which synergistically with CRH increases ACTH,[38] T-cells also secrete glucosteroid response modifying factor (GRMF or GAF) as well as IL-1; both increase the amount of cortisol required to inhibit almost all the immune cells.[39] Immune cells then assume their own regulation, but at a higher cortisol setpoint. The increase in cortisol in diarrheic calves is minimal over healthy calves, however, and falls over time.[51] The cells do not lose all their fight-or-flight override because of interleukin-1's synergism with CRH. Cortisol even has a negative feedback effect on interleukin-1[38]—especially useful for those diseases which gain an advantage by forcing the hypothalamus to secrete too much CRH, such as those caused by endotoxic bacteria. The suppressor immune cells are not affected by GRMF,[39] so the immune cells' effective setpoint may be even higher than the setpoint for physiological processes. GRMF (known as GAF in this reference) primarily affects the liver (rather than the kidneys) for some physiological processes.[52]
High potassium media (which stimulates aldosterone secretion in vitro) also stimulate cortisol secretion from the fasciculata zone of canine adrenals [53]—unlike corticosterone, upon which potassium has no effect.[54] Potassium loading also increases ACTH and cortisol in humans.[55] This is probably the reason why potassium deficiency causes cortisol to decline (as mentioned) and causes a decrease in conversion of 11-deoxycortisol to cortisol.[56] This may also have a role in rheumatoid-arthritis pain; cell potassium is always low in RA.[57]
Factors generally reducing cortisol levels
- Magnesium supplementation decreases serum cortisol levels after aerobic exercise,[58][59] but not after resistance training.[60]
- Omega 3 fatty acids have a dose-dependent effect [61] in slightly reducing cortisol release influenced by mental stress,[62] suppressing the synthesis of interleukin-1 and -6 and enhancing the synthesis of interleukin-2; the former promotes higher CRH release. Omega 6 fatty acids, on the other hand, have an inverse effect on interleukin synthesis.[citation needed]
- Music therapy can reduce cortisol levels in certain situations.[63]
- Massage therapy can reduce cortisol.[64]
- Laughing, and the experience of humour, can lower cortisol levels.[65]
- Crying can reduce cortisol levels. William H. Frey II, a biochemist at the University of Minnesota, proposed that people feel "better" after crying, due to the elimination of hormones associated with stress, specifically adrenocorticotropic hormone.[66] This, paired with increased mucosal secretion during crying, could lead to a theory that crying is a mechanism developed in humans to dispose of this stress hormone when levels grow too high.
- Soy-derived phosphatidylserine interacts with cortisol; the correct dose, however, is unclear.[67][68]
- Vitamin C blunts cortisol release in response to mental and physical stressors.[69]
- Black tea may hasten recovery from a high-cortisol condition.[70][71]
- Regular dancing to Argentine tango has been shown to lead to significant decreases in salivary cortisol concentrations.[72]
- Sexual intercourse. [73]
Factors generally increasing cortisol levels
- Caffeine may increase cortisol levels.[74]
- Sleep deprivation.[75]
- Intense (high VO2 max) or prolonged physical exercise stimulates cortisol release to increase gluconeogenesis and maintain blood glucose.[76] Proper nutrition[77] and high-level conditioning[78] can help stabilize cortisol release.
- The Val/Val variation of the BDNF gene in men, and the Val/Met variation in women, are associated with increased salivary cortisol in a stressful situation.[79]
- Hypoestrogenism and melatonin supplementation increase cortisol levels in postmenopausal women.[80]
- Burnout is associated with higher cortisol levels.[81]
- Severe trauma or stressful events can elevate cortisol levels in the blood for prolonged periods.[82]
- Subcutaneous adipose tissue regenerates cortisol from cortisone.[83]
- Anorexia nervosa may be associated with increased cortisol levels.[84]
- The serotonin receptor gene 5HTR2C is associated with increased cortisol production in men.[85]
- Some formulations of combined oral contraceptive pills increase cortisol levels in young women who perform whole-body-resistance exercise training.[86]
- Commuting increases cortisol levels relative to the length of the trip, its predictability and the amount of effort involved.[87]
- Stimuli associated with sexual intercourse can increase cortisol levels in Gilts (a young female pig that has not produced her first litter) .[88]
Clinical chemistry
- Hypercortisolism: Excessive levels of cortisol in the blood. (See Cushing's syndrome.)
- Hypocortisolism (adrenal insufficiency): Insufficient levels of cortisol in the blood.
The relationship between cortisol and ACTH, and some consequent conditions, are as follows:
THE DISORDERS OF CORTISOL SECRETION Plasma ACTH ↓ ↑ Plasma Cortisol ↑ Primary hypercortisolism (Cushing's syndrome) Secondary hypercortisolism (pituitary or ectopic tumor, Cushing's disease, pseudo-Cushing's syndrome) ↓ Secondary hypocortisolism (pituitary tumor, Sheehan's syndrome) Primary hypocortisolism (Addison's disease, Nelson's syndrome) A 2010 study has found that serum cortisol predicts increased cardiovascular mortality in patients with acute coronary syndrome.[89][90]
Pharmacology
Hydrocortisone is the pharmaceutical term for cortisol used in oral administration, intravenous injection or topical application. It is used as an immunosuppressive drug, given by injection in the treatment of severe allergic reactions such as anaphylaxis and angioedema, in place of prednisolone in patients who need steroid treatment but cannot take oral medication, and perioperatively in patients on longterm steroid treatment to prevent Addisonian crisis. It may be used topically for allergic rashes, eczema, psoriasis and certain other inflammatory skin conditions. It may also be injected into inflamed joints resulting from diseases such as gout.
Compared to hydrocortisone, prednisolone is about four times as strong and dexamethasone about forty times as strong, in their anti-inflammatory effect.[citation needed] For side effects, see corticosteroid and prednisolone.
Hydrocortisone creams and ointments are available in most countries without prescription in strengths ranging from 0.05% to 2.5% (depending on local regulations) with stronger forms available by prescription only. Covering the skin after application increases the absorption and effect. Such enhancement is sometimes prescribed, but otherwise should be avoided to prevent overdose and systemic impact.
Advertising for the dietary supplement CortiSlim originally (and falsely) claimed that it contributed to weight loss by blocking cortisol. The manufacturer was fined $12 million by the Federal Trade Commission in 2007 for false advertising, and no longer claims in their marketing that CortiSlim is a cortisol antagonist.[91]
Biochemistry
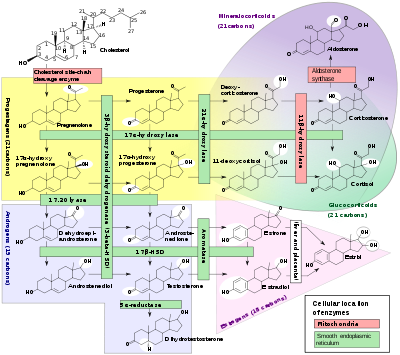
Biosynthesis
Cortisol is synthesized from cholesterol. Synthesis takes place in the zona fasciculata of the adrenal cortex. (The name cortisol is derived from cortex.) While the adrenal cortex also produces aldosterone (in the zona glomerulosa) and some sex hormones (in the zona reticularis), cortisol is its main secretion. The medulla of the adrenal gland lies under the cortex, mainly secreting the catecholamines adrenaline (epinephrine) and noradrenaline (norepinephrine) under sympathetic stimulation.
The synthesis of cortisol in the adrenal gland is stimulated by the anterior lobe of the pituitary gland with adrenocorticotropic hormone (ACTH); ACTH production is in turn stimulated by corticotropin-releasing hormone (CRH), which is released by the hypothalamus. ACTH increases the concentration of cholesterol in the inner mitochondrial membrane, via regulation of the STAR (steroidogenic acute regulatory) protein. It also stimulates the main rate-limiting step in cortisol synthesis, in which cholesterol is converted to pregnenolone and catalyzed by Cytochrome P450SCC (side chain cleavage enzyme).[92]
Metabolism
Cortisol is metabolized by the 11-beta hydroxysteroid dehydrogenase system (11-beta HSD), which consists of two enzymes: 11-beta HSD1 and 11-beta HSD2.
- 11-beta HSD1 utilizes the cofactor NADPH to convert biologically-inert cortisone to biologically-active cortisol
- 11-beta HSD2 utilizes the cofactor NAD+ to convert cortisol to cortisone
Overall, the net effect is that 11-beta HSD1 serves to increase the local concentrations of biologically-active cortisol in a given tissue; 11-beta HSD2 serves to decrease local concentrations of biologically-active cortisol.
Cortisol is also metabolized into 5-alpha tetrahydrocortisol (5-alpha THF) and 5-beta tetrahydrocortisol (5-beta THF), reactions for which 5-alpha reductase and 5-beta reductase are the rate-limiting factors respectively. 5-beta reductase is also the rate-limiting factor in the conversion of cortisone to tetrahydrocortisone (THE).
An alteration in 11-beta HSD1 has been suggested to play a role in the pathogenesis of obesity, hypertension, and insulin resistance known as metabolic syndrome.[93]
An alteration in 11-beta HSD2 has been implicated in essential hypertension and is known to lead to the syndrome of apparent mineralocorticoid excess (SAME).[citation needed]
External links
References
- ^ http://themedicalbiochemistrypage.org/images/adrenalsteroidsynthesis.jpg
- ^ First Aid USMLE Step 1 2009, Tao Le et al.
- ^ hydrocortisoneshots.com
- ^ de Weerth C, Zijl R, Buitelaar J (2003). "Development of cortisol circadian rhythm in infancy". Early Hum Dev 73 (1-2): 39–52. doi:10.1016/S0378-3782(03)00074-4. PMID 12932892.
- ^ "Asperger's stress hormone 'link'". BBC News. 2009-04-02. http://news.bbc.co.uk/2/hi/health/7976489.stm. Retrieved 2010-04-30.
- ^ a b c d Biochemistry Reference Ranges at Good Hope Hospital Retrieved on Nov 8, 2009
- ^ a b c d Derived from molar values using molar mass of 362 g/mol
- ^ a b Converted from µg/24h, using molar mass of 362.460 g/mol
- ^ a b c Görges, R.; Knappe, G.; Gerl, H.; Ventz, M.; Stahl, F. (1999). "Diagnosis of Cushing's syndrome: Re-evaluation of midnight plasma cortisol vs urinary free cortisol and low-dose dexamethasone suppression test in a large patient group". Journal of endocrinological investigation 22 (4): 241–249. PMID 10342356.
- ^ a b MedlinePlus > Cortisol - urine. Update Date: 11/23/2009. Updated by: Ari S. Eckman. Also reviewed by David Zieve.
- ^ a b c Converted from nmol/24h, using molar mass of 362.460 g/mol
- ^ "Cortisol and Stress: How Cortisol Affects Your Body, and How To Stay Healthy in the Face of Stress". Stress.about.com. http://stress.about.com/od/stresshealth/a/cortisol.htm. Retrieved 2010-06-14.
- ^ a b USMLE Step 1 Secrets. 2003. p. 63.
- ^ King, Michael W. (2005). Lange Q&A USMLE Step 1 (Sixth ed.). New York: McGraw-Hill, Medical Pub. Division. p. 82. ISBN 0071445781.
- ^ Piroli, G. G.; Grillo, C. A.; Reznikov, L. R.; Adams, S.; McEwen, B. S.; Charron, M. J.; Reagan, L. P. (2007). "Corticosterone Impairs Insulin-Stimulated Translocation of GLUT4 in the Rat Hippocampus". Neuroendocrinology 85 (2): 71–80. doi:10.1159/000101694. PMID 17426391.
- ^ Baynes, J., Dominiczak, M., Medical Biochemistry. Elsevier Limited; Third Edition (2009). ISBN 978-0-323-05371-6.
- ^ Houck JC, Sharma VK, Patel YM, Gladner JA. Induction of collagenolytic and proteolytic activities by anti-inflammatoes this by inhibiting collagen formation, decreasing amino acid uptake by muscle, and inhibiting protein synthesis..
- ^ Manchester, K.L., “Sites of Hormonal Regulation of Protein Metabolism. p. 229”, Mammalian Protein [Munro, H.N., Ed.]. Academic Press, New York. On p273.
- ^ Husband AJ, Brandon MR, Lascelles AK (October 1973). "The effect of corticosteroid on absorption and endogenous production of immunoglobulins in calves". Aust J Exp Biol Med Sci 51 (5): 707–10. doi:10.1038/icb.1973.67. PMID 4207041.
- ^ Posey WC, Nelson HS, Branch B, Pearlman DS (December 1978). "The effects of acute corticosteroid therapy for asthma on serum immunoglobulin levels". J. Allergy Clin. Immunol. 62 (6): 340–8. doi:10.1016/0091-6749(78)90134-3. PMID 712020.
- ^ Soffer, L.J.; Dorfman, R.I.; Gabrilove, J.L,. “The Human Adrenal Gland”. Febiger, Phil.
- ^ Kokshchuk, G.I.; Pakhmurnyi, B.A. (1979) “Role of Glucocorticoids in Regulation of the Acid-Excreting Function of the Kidneys”. Fiziol. Z H SSR I.M.I.M. Sechenova 65: 751,.
- ^ Tai YH, Decker RA, Marnane WG, Charney AN, Donowitz M (May 1981). "Effects of methylprednisolone on electrolyte transport by in vitro rat ileum". Am. J. Physiol. 240 (5): G365–70. PMID 6112881.
- ^ a b Sandle GI, Keir MJ, Record CO (1981). "The effect of hydrocortisone on the transport of water, sodium, and glucose in the jejunum. Perfusion studies in normal subjects and patients with coeliac disease". Scand. J. Gastroenterol. 16 (5): 667–71. doi:10.3109/00365528109182028. PMID 7323700.
- ^ Mason PA, Fraser R, Morton JJ, Semple PF, Wilson A (August 1977). "The effect of sodium deprivation and of angiotensin II infusion on the peripheral plasma concentrations of 18-hydroxycorticosterone, aldosterone and other corticosteroids in man". J. Steroid Biochem. 8 (8): 799–804. doi:10.1016/0022-4731(77)90086-3. PMID 592808.
- ^ Gorbman, A.; Dickhoff, W.W.; Vigna, S.R.; Clark, N.B.; Muller, A.F,. “Comparative Endocrinology”. John Wiley and Sons, New York.
- ^ Muller AF Oconnor CM, ed. (1958) “An International Symposium on Aldosterone”, page 58. Little Brown & Co.
- ^ KNIGHT RP, KORNFELD DS, GLASER GH, BONDY PK (February 1955). "Effects of intravenous hydrocortisone on electrolytes of serum and urine in man". J. Clin. Endocrinol. Metab. 15 (2): 176–81. doi:10.1210/jcem-15-2-176. PMID 13233328.
- ^ BARGER AC, BERLIN RD, TULENKO JF (June 1958). "Infusion of aldosterone, 9-alpha-fluorohydrocortisone and antidiuretic hormone into the renal artery of normal and adrenalectomized, unanesthetized dogs: effect on electrolyte and water excretion". Endocrinology 62 (6): 804–15. doi:10.1210/endo-62-6-804. PMID 13548099.
- ^ Boykin J, DeTorrenté A, Erickson A, Robertson G, Schrier RW (October 1978). "Role of plasma vasopressin in impaired water excretion of glucocorticoid deficiency". J. Clin. Invest. 62 (4): 738–44. doi:10.1172/JCI109184. PMC 371824. PMID 701472. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=371824.
- ^ Dingman, J.F.; Gonzalez-Auvert Ahmed, A.B.J.; Akinura, A. (1965) “Antidiuretic Hormone in Adrenal Insufficiency”. Journal of Clinical Investigation 44: 1041,.
- ^ Weber, C.E (1984). “Copper Response to Rheumatoid Arthritis”. Medical Hypotheses 15: 333-348, on p337,.
- ^ Weber, C.E. (1984) “Copper Response to Rheumatoid Arthritis”. Medical Hypotheses 15: 333,.on p334.
- ^ Flohe, L.; Beckman, R.; Giertz, H.; Loschen, G. “Oxygen Centered Free Radicals as Mediators of Inflammation. p. 405”, Oxidative Stress (Sies H, ed) Academic Press, New York.
- ^ Piletz JE, Herschman HR (June 1983). "Hepatic metallothionein synthesis in neonatal Mottled-Brindled mutant mice". Biochem. Genet. 21 (5-6): 465–75. doi:10.1007/BF00484439. PMID 6870774.
- ^ Chambers, J.W.; Georg, R.H. and Bass, A.D. (1965) “Effect of Hydrocortisone and Insulin on Uptake of Alpha Aminoisobutyric Acid by Isolated Perfused Rat Liver”. Mol. Pharmacol. 1: 66,.
- ^ Palacios R., Sugawara I. (1982). "Hydrocortisone abrogates proliferation of T cells in autologous mixed lymphocyte reaction by rendering the interleukin-2 Producer T cells unresponsive to interleukin-1 and unable to synthesize the T-cell growth factor". Scand J Immunol 15 (1): 25–31. doi:10.1111/j.1365-3083.1982.tb00618.x. PMID 6461917.
- ^ a b c Besedovsky, H.O.; Del Rey, A.; Sorkin, E. (1984) "Integration of Activated Immune Cell Products in Immune Endocrine Feedback Circuits." p. 200 in Leukocytes and Host Defense Vol. 5 [Oppenheim, J.J.; Jacobs, D.M., eds]. Alan R. Liss, New York,.
- ^ a b c Fairchild SS, Shannon K, Kwan E, Mishell RI (February 1984). "T cell-derived glucosteroid response-modifying factor (GRMFT): a unique lymphokine made by normal T lymphocytes and a T cell hybridoma". J. Immunol. 132 (2): 821–7. PMID 6228602.
- ^ Onsrud M, Thorsby E (1981). "Influence of in vivo hydrocortisone on some human blood lymphocyte subpopulations. I. Effect on natural killer cell activity". Scand. J. Immunol. 13 (6): 573–9. PMID 7313552.
- ^ Knight, R.P., Jr. Kornfield, D.S. Glaser, G.H. Bondy, P.K. (1955). "Effects of intravenous hydrocortisone on electrolytes of serum and urine in man". J Clin Endocrinol Metab 15 (2): 176–81. doi:10.1210/jcem-15-2-176. PMID 13233328.
- ^ Shultz TD, Bollman S, Kumar R (June 1982). "Decreased intestinal calcium absorption in vivo and normal brush border membrane vesicle calcium uptake in cortisol-treated chickens: evidence for dissociation of calcium absorption from brush border vesicle uptake". Proc. Natl. Acad. Sci. U.S.A. 79 (11): 3542–6. doi:10.1073/pnas.79.11.3542. PMC 346457. PMID 6954501. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=346457.
- ^ Mc Auley MM, Kenny RA, Kirkwood TT, Wilkinson DD, Jones JJ, Miller VM (March 2009). "A Mathematical Model of aging-related and cortisol induced hippocampal dysfunction". BMC Neurosci 10 (1): 26. doi:10.1186/1471-2202-10-26. PMC 2680862. PMID 19320982. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2680862.
- ^ de Quervain, D et al., Stress and glucocorticoids impair retrieval of long-term spatial memory. Nature, 394, 787-790 (1998)
- ^ de Quervain, D et al., Acute cortisone administration impairs retrieval of long-term declarative memory in humans. Nature Neuroscience, 3, 313-314 (2000)
- ^ An Introduction to Behavioral Endocrinology, Randy J Nelson, 3rd edition, Sinauer
- ^ "Stress Cortisol Connection". Unm.edu. http://www.unm.edu/~lkravitz/Article%20folder/stresscortisol.html. Retrieved 2010-06-14.
- ^ Boron and Boulpaep, Medical physiology 2009
- ^ Davies E., Keyon C.J., Fraser R. (1985). "The role of calcium ions in the mechanism of ACTH stimulation of cortisol synthesis". Steroids 45: 557. PMID 3012830.
- ^ Plotsky PM, Otto S, Sapolsky RM (September 1986). "Inhibition of immunoreactive corticotropin-releasing factor secretion into the hypophysial-portal circulation by delayed glucocorticoid feedback". Endocrinology 119 (3): 1126–30. doi:10.1210/endo-119-3-1126. PMID 3015567.
- ^ Dvorak M (1971). "Plasma 17-Hydroxycorticosteroid Levels in Healthy and Diarrheic Calves". British Veterinarian Journal 127: 372.
- ^ Stith RD, McCallum RE (1986). "General effect of endotoxin on glucocorticoid receptors in mammalian tissues". Circ. Shock 18 (4): 301–9. PMID 3084123.
- ^ Mikosha, A.S.; Pushkarov, I.S.; Chelnakova, I.S.; Remennikov, G.Y.A. (1991) “Potassium Aided Regulation of Hormone Biosynthesis in Adrenals of Guinea Pigs Under Action of Dihydropyridines: Possible Mechanisms of Changes in Steroidogenesis Induced by 1,4, Dihydropyridines in Dispersed Adrenocorticytes.” Fiziol. [Kiev] 37: 60,.
- ^ Mendelsohn FA, Mackie C (July 1975). "Relation of intracellular K+ and steroidogenesis in isolated adrenal zona glomerulosa and fasciculata cells". Clin Sci Mol Med 49 (1): 13–26. PMID 168026.
- ^ Ueda Y, Honda M, Tsuchiya M, et al. (April 1982). "Response of plasma ACTH and adrenocortical hormones to potassium loading in essential hypertension". Jpn. Circ. J. 46 (4): 317–22. PMID 6283190.
- ^ Bauman K Muller J 1972 “Effect of potassium on the final status of aldosterone biosynthesis in the rat. I 18-hydroxylation and 18hydroxy dehydrogenation. II beta-hydroxylation.” Acta Endocrin. Copenh. 69; I 701-717, II 718-730.
- ^ LaCelle PL et al. (1964) “An investigation of total body potassium in patients with rheumatoid arthritis.” Proceedings of the Annual Meeting of the American Rheumatism Association, Arthritis and Rheumatism 7; 321.
- ^ Golf, S. H.; Happel, O.; Graef, V.; Seim, K. E. (Nov 1984). "Plasma aldosterone, cortisol and electrolyte concentrations in physical exercise after magnesium supplementation" (Free full text). Journal of clinical chemistry and clinical biochemistry. Zeitschrift fur klinische Chemie und klinische Biochemie 22 (11): 717–721. ISSN 0340-076X. PMID 6527092. http://toxnet.nlm.nih.gov/cgi-bin/sis/search/r?dbs+hsdb:@term+@rn+50-23-7.
- ^ Golf, S. B.; Bender, S.; Grüttner, J. (Sep 1998). "On the significance of magnesium in extreme physical stress". Cardiovascular drugs and therapy / sponsored by the International Society of Cardiovascular Pharmacotherapy. 12 2 (2suppl): 197–202. doi:10.1023/A:1007708918683. ISSN 0920-3206. PMID 9794094.
- ^ Wilborn, D.; Kerksick, M.; Campbell, I.; Taylor, W.; Marcello, M.; Rasmussen, J.; Greenwood, C.; Almada, A. et al. (Dec 2004). "Effects of Zinc Magnesium Aspartate (ZMA) Supplementation on Training Adaptations and Markers of Anabolism and Catabolism" (Free full text). Journal of the International Society of Sports Nutrition 1 (2): 12–20. doi:10.1186/1550-2783-1-2-12. PMC 2129161. PMID 18500945. http://www.jissn.com/content/1/2/12.
- ^ Bhathena, S. B.; Berlin, E.; Judd, J. T.; Kim, Y. C.; Law, J. S.; Bhagavan, H. N.; Ballard-Barbash, R.; Nair, P. P. (1 October 1991). "Effects of omega 3 fatty acids and vitamin E on hormones involved in carbohydrate and lipid metabolism in men" (Free full text). The American journal of clinical nutrition 54 (4): 684–688. ISSN 0002-9165. PMID 1832814. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=1832814.
- ^ Delarue, J. M.; Matzinger, O.; Binnert, C.; Schneiter, P.; Chioléro, R.; Tappy, L. (Jun 2003). "Fish oil prevents the adrenal activation elicited by mental stress in healthy men" (Free full text). Diabetes & metabolism 29 (3): 289–295. doi:10.1016/S1262-3636(07)70039-3. ISSN 1262-3636. PMID 12909818. http://www.masson.fr/masson/MDOI-DM-06-2003-29-3-1262-3636-101019-ART12.
- ^ Uedo, N. I.; Ishikawa, H.; Morimoto, K.; Ishihara, R.; Narahara, H.; Akedo, I.; Ioka, T.; Kaji, I. et al. (Mar 2004). "Reduction in salivary cortisol level by music therapy during colonoscopic examination" (Free full text). Hepato-gastroenterology 51 (56): 451–453. ISSN 0172-6390. PMID 15086180. http://www.nlm.nih.gov/medlineplus/colonoscopy.html.
- ^ Field, T.; Hernandez-Reif, M.; Diego, M.; Schanberg, S.; Kuhn, C. (Oct 2005). "Cortisol decreases and serotonin and dopamine increase following massage therapy". The International journal of neuroscience 115 (10): 1397–1413. doi:10.1080/00207450590956459. ISSN 0020-7454. PMID 16162447.
- ^ Berk et al.. "Cortisol and Catecholamine stress hormone decrease is associated with the behavior of perceptual anticipation of mirthful laughter". The FASEB Journal 22 (1): 946.11. http://www.fasebj.org/cgi/content/meeting_abstract/22/1_MeetingAbstracts/946.11. Retrieved 2010-06-14.
- ^ "Crying; The Mystery of Tears" personal page of Frey WH with quote from his book
- ^ Hellhammer, J.; Fries, E.; Buss, C.; Engert, V.; Tuch, A.; Rutenberg, D.; Hellhammer, D. (Jun 2004). "Effects of soy lecithin phosphatidic acid and phosphatidylserine complex (PAS) on the endocrine and psychological responses to mental stress". Stress (Amsterdam, Netherlands) 7 (2): 119–126. doi:10.1080/10253890410001728379. ISSN 1025-3890. PMID 15512856.
- ^ Starks MA, Starks SL, Kingsley M, Purpura M, Jäger R (2008). "The effects of phosphatidylserine on endocrine response to moderate intensity exercise". J Int Soc Sports Nutr 5: 11. doi:10.1186/1550-2783-5-11. PMC 2503954. PMID 18662395. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2503954.
- ^ Vitamin C: Stress Buster Psychology today
- ^ "Black tea 'soothes away stress'". BBC News. 2006-10-04. http://news.bbc.co.uk/2/hi/health/5405686.stm. Retrieved 2010-04-30.
- ^ "Journal Article". SpringerLink. http://www.springerlink.com/content/m226111566k24u65/. Retrieved 2010-06-14.
- ^ Cynthia Quiroga Murcia, Stephan Bongard, and Gunter Kreutz (July 2009). "Emotional and Neurohumoral Responses to Dancing Tango Argentino - The Effects of Music and Partner". Music and Medicine 1 (1): 14–21. http://mmd.sagepub.com/content/1/1/14.full. Retrieved 2011-08-07.
- ^ Scott, Elizabeth. "Cortisol and Stress: How to Stay Healthy". Cortisol and Your Body. http://stress.about.com/od/stresshealth/a/cortisol.htm.
- ^ Lovallo WR, Farag NH, Vincent AS, Thomas TL, Wilson MF (March 2006). "Cortisol responses to mental stress, exercise, and meals following caffeine intake in men and women". Pharmacol. Biochem. Behav. 83 (3): 441–7. doi:10.1016/j.pbb.2006.03.005. PMC 2249754. PMID 16631247. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2249754.
- ^ "Sleep loss results in an elevation of cortisol levels the next evening". Cat.inist.fr. http://cat.inist.fr/?aModele=afficheN&cpsidt=2068517. Retrieved 2010-06-14.
- ^ Robson PJ, Blannin AK, Walsh NP, Castell LM, Gleeson M (February 1999). "Effects of exercise intensity, duration and recovery on in vitro neutrophil function in male athletes". Int J Sports Med 20 (2): 128–35. doi:10.1055/s-2007-971106. PMID 10190775.
- ^ Gleeson, M. (Mar 2006). "Can nutrition limit exercise-induced immunodepression?". Nutrition reviews 64 (3): 119–131. doi:10.1111/j.1753-4887.2006.tb00195.x. ISSN 0029-6643. PMID 16572599.
- ^ Kraemer WJ, Spiering BA, Volek JS, et al. (January 2009). "Recovery from a national collegiate athletic association division I football game: muscle damage and hormonal status". J Strength Cond Res 23 (1): 2–10. doi:10.1519/JSC.0b013e31819306f2 (inactive 2010-01-03). PMID 19077734.
- ^ Shalev, I.; Lerer, E.; Israel, S.; Uzefovsky, F.; Gritsenko, I.; Mankuta, D.; Ebstein, P.; Kaitz, M. (Apr 2009). "BDNF Val66Met polymorphism is associated with HPA axis reactivity to psychological stress characterized by genotype and gender interactions". Psychoneuroendocrinology 34 (3): 382–388. doi:10.1016/j.psyneuen.2008.09.017. ISSN 0306-4530. PMID 18990498.
- ^ Cagnacci, A.; Soldani, R.; Yen, S. S. C. (Mar 1997). "Melatonin enhances cortisol levels in aged women: reversible by estrogens" (Free full text). Journal of pineal research 22 (2): 81–85. doi:10.1111/j.1600-079X.1997.tb00307.x. ISSN 0742-3098. PMID 9181519. http://toxnet.nlm.nih.gov/cgi-bin/sis/search/r?dbs+hsdb:@term+@rn+50-23-7.
- ^ Wingenfeld, K.; Schulz, M.; Damkroeger, A.; Rose, M.; Driessen, M. (Mar 2009). "Elevated diurnal salivary cortisol in nurses is associated with burnout but not with vital exhaustion". Psychoneuroendocrinology 34 (8): 1144–1151. doi:10.1016/j.psyneuen.2009.02.015. ISSN 0306-4530. PMID 19321266.
- ^ Advanced Nutrition and Human Metabolism. 2008. p. 247.
- ^ "Cortisol Release From Adipose Tissue by 11β-Hydroxysteroid Dehydrogenase Type 1 in Humans". Diabetes.diabetesjournals.org. 2008-10-13. http://diabetes.diabetesjournals.org/cgi/content/abstract/58/1/46. Retrieved 2010-06-14.
- ^ Haas et al., 10.3945/ajcn.2008.26958. "Body composition changes in female adolescents with anorexia nervosa". American Journal of Clinical Nutrition. doi:10.3945/ajcn.2008.26958. http://www.ajcn.org/cgi/content/abstract/ajcn.2008.26958v1. Retrieved 2010-06-14.
- ^ "New Clues about Genetic Influence of Stress on Men’s Health". Dukehealth.org. http://www.dukehealth.org/HealthLibrary/News/new_clues_about_genetic_influence_of_stress_on_men_s_health. Retrieved 2010-06-14.
- ^ "Birth control pills can limit muscle-training gains". Sciencenews.org. http://sciencenews.org/view/generic/id/43210/title/Science_%2B_the_Public__Birth_control_pills_can_limit_muscle-training_gains. Retrieved 2010-06-14.
- ^ "The Impact of Mode and Mode Transfer on Commuter Stress, The Montclair Connection" (PDF). http://www.utrc2.org/research/assets/74/commuterstress2-report1.pdf. Retrieved 2010-06-14.
- ^ Kotwica, G; Franczak A, Okrasa S, Koziorowski M, Kurowicka B. (March 2002). "Effects of mating stimuli and oxytocin on plasma cortisol concentration in gilts.". Reprod Biol. 2 (1): 25–37. PMID 14666160.
- ^ "Serum cortisol predicts increased cardiovascular mortality in patients with acute coronary syndrome". Endocrine-abstracts.org. http://www.endocrine-abstracts.org/ea/0022/ea0022OC4.6.htm. Retrieved 2010-06-14.
- ^ Terzolo, M.; Bovio, S.; Pia, A.; Conton, P.; Reimondo, G.; Dall'asta, C.; Bemporad, D.; Angeli, A. et al. (2005). "Midnight serum cortisol as a marker of increased cardiovascular risk in patients with a clinically inapparent adrenal adenoma". European journal of endocrinology / European Federation of Endocrine Societies 153 (2): 307–315. doi:10.1530/eje.1.01959. PMID 16061838.
- ^ Iwata, Edward (January 5, 2007). "Diet pill sellers fined $25M". USA Today. http://www.usatoday.com/news/washington/2007-01-04-weight-loss-pills_x.htm. Retrieved 2008-10-26.
- ^ Mechanism of ACTH action on adrenal cortical cells Andrew N. Margioris, M.D., and Christos Tsatsanis, Ph.D. Updated: December 4, 2006
- ^ [1] Tomlinson JW, Walker EA, Bujalska IJ, Draper N, Lavery GG, Cooper MS, Hewison M, Stewart PM. 11beta-hydroxysteroid dehydrogenase type 1: a tissue-specific regulator of glucocorticoid response. Endocr Rev. 2004 Oct;25(5):831-66.
Endocrine system: hormones (Peptide hormones · Steroid hormones) Endocrine
glandsTestis: testosterone · AMH · inhibin
Ovary: estradiol · progesterone · activin and inhibin · relaxin (pregnancy)
Placenta: hCG · HPL · estrogen · progesteroneIslet-Acinar
AxisNon-end.
glandsThymus: Thymosin (Thymosin α1, Thymosin beta) · Thymopoietin · Thymulin
Digestive system: Stomach: gastrin · ghrelin · Duodenum: CCK · GIP · secretin · motilin · VIP · Ileum: enteroglucagon · peptide YY · Liver/other: Insulin-like growth factor (IGF-1, IGF-2)
Adipose tissue: leptin · adiponectin · resistin
Kidney: JGA (renin) · peritubular cells (EPO) · calcitriol · prostaglandin
Heart: Natriuretic peptide (ANP, BNP)Cholesterol and steroid metabolic intermediates Mevalonate pathway to HMG-CoAto DMAPPGeranyl-Prephytoene diphosphate · PhytoeneNon-mevalonate pathway To Cholesterol Farnesyl pyrophosphate · Squalene · 2,3-Oxidosqualene · Lanosterol
Lanosterol · Lathosterol · 7-Dehydrocholesterol · Cholesterol
Lanosterol · Zymosterol · 7-Dehydrodesmosterol · Desmosterol · CholesterolSteroid Nonhuman biochemical families: prot · nucl · carb (glpr, alco, glys) · lipd (fata/i, phld, strd, gllp, eico) · amac/i · ncbs/i · ttpy/iAntidiarrheals, intestinal anti-inflammatory/anti-infective agents (A07) Rehydration Intestinal anti-infectives Antibiotics (Neomycin, Nystatin, Natamycin, Streptomycin, Polymyxin B, Paromomycin, Amphotericin B, Kanamycin, Vancomycin, Colistin, Rifaximin)
Sulfonamides (Phthalylsulfathiazole, Sulfaguanidine, Succinylsulfathiazole)
Nitrofuran (Nifuroxazide, Nifurzide)
Arsenical (Acetarsol)
Oxyquinoline (Broxyquinoline)Intestinal adsorbents Antipropulsives (opioids) Opium Tincture (Laudanum) • Codeine • Morphine • Camphorated Opium Tincture (Paregoric)
crosses BBB: Diphenoxylate (Diphenoxylate/atropine) • Difenoxin
does not cross BBB: LoperamideIntestinal anti-inflammatory agents corticosteroids acting locally (Prednisolone, Hydrocortisone, Prednisone, Betamethasone, Tixocortol, Budesonide, Beclometasone)
antiallergic agents, excluding corticosteroids (Cromoglicic acid)
aminosalicylic acid and similar agents (Sulfasalazine, Mesalazine, Olsalazine, Balsalazide)Antidiarrheal micro-organisms Other antidiarrheals Otologicals (S02) Anti-infectives Acetic acid • Aluminium acetotartrate • Boric acid • Chloramphenicol • Chlorhexidine • Ciprofloxacin • Clioquinol • Gentamicin • Hydrogen peroxide • Miconazole • Neomycin • Nitrofurazone • Ofloxacin • Polymyxin B • Rifamycin • TetracyclineCorticosteroids Analgesics and anesthetics M: EAR
anat(e/p)/phys/devp
noco/cong, epon
proc, drug(S2)
Wikimedia Foundation. 2010.