- Psoriasis
-
Psoriasis Classification and external resources 
A person whose back and arms are affected by psoriasisICD-10 L40 ICD-9 696 OMIM 177900 DiseasesDB 10895 MedlinePlus 000434 eMedicine emerg/489 Dermatology:derm/365 plaque
derm/361 guttate
derm/363 nails
derm/366 pustular
Arthritis derm/918
Radiology radio/578
Physical Medicine pmr/120MeSH D011565 Psoriasis (
 /səˈraɪ.əsɨs/) is an autoimmune disease that appears on the skin. It occurs when the immune system mistakes the skin cells as a pathogen, and sends out faulty signals that speed up the growth cycle of skin cells. Psoriasis is not contagious.[1] However, psoriasis has been linked to an increased risk of stroke. [2] There are five types of psoriasis: plaque, guttate, inverse, pustular and erythrodermic. The most common form, plaque psoriasis, is commonly seen as red and white hues of scaly patches appearing on the top first layer of the epidermis (skin). Some patients, though, have no dermatological symptoms.
/səˈraɪ.əsɨs/) is an autoimmune disease that appears on the skin. It occurs when the immune system mistakes the skin cells as a pathogen, and sends out faulty signals that speed up the growth cycle of skin cells. Psoriasis is not contagious.[1] However, psoriasis has been linked to an increased risk of stroke. [2] There are five types of psoriasis: plaque, guttate, inverse, pustular and erythrodermic. The most common form, plaque psoriasis, is commonly seen as red and white hues of scaly patches appearing on the top first layer of the epidermis (skin). Some patients, though, have no dermatological symptoms.In plaque psoriasis, skin rapidly accumulates at these sites, which gives it a silvery-white appearance. Plaques frequently occur on the skin of the elbows and knees, but can affect any area, including the scalp, palms of hands and soles of feet, and genitals. In contrast to eczema, psoriasis is more likely to be found on the outer side of the joint.
The disorder is a chronic recurring condition that varies in severity from minor localized patches to complete body coverage. Fingernails and toenails are frequently affected (psoriatic nail dystrophy) and can be seen as an isolated symptom. Psoriasis can also cause inflammation of the joints, which is known as psoriatic arthritis. Between 10-30% of all people with psoriasis also have psoriatic arthritis.[3][4]
The cause of psoriasis is not fully understood, but it is believed to have a genetic component and local psoriatic changes can be triggered by an injury to the skin known as the Koebner phenomenon,[5] see Koebnerisin. Various environmental factors have been suggested as aggravating to psoriasis, including stress, withdrawal of systemic corticosteroid, as well as other environmental factors, but few have shown statistical significance.[6] There are many treatments available, but because of its chronic recurrent nature, psoriasis is a challenge to treat. Withdrawal of corticosteroids (topical steroid cream) can aggravate the condition due to the 'rebound effect' of corticosteroids but this may be followed by cure.[7]
Contents
Classification
The symptoms of psoriasis can manifest in a variety of forms. Variants include plaque, pustular, guttate and flexural psoriasis. This section describes each type (with ICD-10 code [8]).[9]
Psoriasis is a chronic relapsing disease of the skin that may be classified into nonpustular and pustular types as follows[10]:
Nonpustular
- Psoriasis vulgaris (chronic stationary psoriasis, plaque-like psoriasis)(L40.0) is the most common form of psoriasis. It affects 80 to 90% of people with psoriasis. Plaque psoriasis typically appears as raised areas of inflamed skin covered with silvery white scaly skin. These areas are called plaques.
- Psoriatic erythroderma (erythrodermic psoriasis)(L40.85)involves the widespread inflammation and exfoliation of the skin over most of the body surface. It may be accompanied by severe itching, swelling and pain. It is often the result of an exacerbation of unstable plaque psoriasis, particularly following the abrupt withdrawal of systemic treatment. This form of psoriasis can be fatal, as the extreme inflammation and exfoliation disrupt the body's ability to regulate temperature and for the skin to perform barrier functions.[11]
Pustular
Pustular psoriasis (L40.1-3, L40.82) appears as raised bumps that are filled with noninfectious pus (pustules). The skin under and surrounding the pustules is red and tender. Pustular psoriasis can be localised, commonly to the hands and feet (palmoplantar pustulosis), or generalised with widespread patches occurring randomly on any part of the body. Types include:
- Generalized pustular psoriasis (pustular psoriasis of von Zumbusch)
- Pustulosis palmaris et plantaris (persistent palmoplantar pustulosis, pustular psoriasis of the Barber type, pustular psoriasis of the extremities)
- Annular pustular psoriasis
- Acrodermatitis continua
- Impetigo herpetiformis
Other
Additional types of psoriasis include[12]:
- Inverse psoriasis (flexural psoriasis, inverse psoriasis)(L40.83-4) appears as smooth inflamed patches of skin. It occurs in skin folds, particularly around the genitals (between the thigh and groin), the armpits, under an overweight abdomen (panniculus), and under the breasts (inframammary fold). It is aggravated by friction and sweat, and is vulnerable to fungal infections.
- Seborrheic-like psoriasis
Guttate psoriasis (L40.4) is characterized by numerous small, scaly, red or pink, teardrop-shaped lesions. These numerous spots of psoriasis appear over large areas of the body, primarily the trunk, but also the limbs and scalp. Guttate psoriasis is often preceded by a streptococcal infection, typically streptococcal pharyngitis. The reverse is not true.
Nail psoriasis (L40.86) produces a variety of changes in the appearance of finger and toe nails. These changes include discolouring under the nail plate, pitting of the nails, lines going across the nails, thickening of the skin under the nail, and the loosening (onycholysis) and crumbling of the nail.
Psoriatic arthritis (L40.5) involves joint and connective tissue inflammation. Psoriatic arthritis can affect any joint, but is most common in the joints of the fingers and toes. This can result in a sausage-shaped swelling of the fingers and toes known as dactylitis. Psoriatic arthritis can also affect the hips, knees and spine (spondylitis). About 10–15% of people who have psoriasis also have psoriatic arthritis.
The migratory stomatitis in the oral cavity mucosa and the geographic tongue that confined to the dorsal and lateral aspects of the tongue mucosa, are believed to be oral manifestations of psoriasis, as being histologically identical to cutaneous psoriasis lesions and more prevalent among psoriasis patients[13], although these conditions are quite common in the non-psoriatic population, affecting 1% to 2.5% of the general population.[13]
Signs and symptoms
Quality of life
Severe cases of psoriasis have been shown to affect health-related quality of life to an extent similar to the effects of other chronic diseases, such as depression, hypertension, congestive heart failure or type 2 diabetes.[14] Depending on the severity and location of outbreaks, individuals may experience significant physical discomfort and some disability. Itching and pain can interfere with basic functions, such as self-care, walking, and sleep. Plaques on hands and feet can prevent individuals from working at certain occupations, playing some sports, and caring for family members or a home. Plaques on the scalp can be particularly embarrassing, as flaky plaque in the hair can be mistaken for dandruff. Medical care can be costly and time-consuming, and can interfere with an employment or school schedule.
Individuals with psoriasis may also feel self-conscious about their appearance and have a poor self-image that stems from fear of public rejection and psychosexual concerns.[citation needed] Psychological distress can lead to significant depression and social isolation.
In a 2008 National Psoriasis Foundation survey of 426 psoriasis sufferers, 71 percent reported the disease was a significant problem in everyday life. More than half reported significant feelings of self-consciousness (63 percent) and embarrassment (58 percent). More than one-third said they avoided social activities and limited dating or intimate interactions.[15]
Many tools exist to measure quality of life of patients with psoriasis and other dermatalogical disorders. Clinical research has indicated individuals often experience a diminished quality of life.[16] A 2009 study looked at the impact of psoriasis by using interviews with dermatologists and exploring patients viewpoint. It found that in cases of mild and severe psoriasis, itch contributed most to the diminished health-related quality of life (HRQoL).[17]
According to a study published in 2010 in the Journal of the American Academy of Dermatology, the reliability of a simple six-point Likert scale for self-assessment of pruritus (itching) by patients was validated in patients with moderate to severe plaque psoriasis.[18] This will allow better communication, assessment, as well as staging and management of itching. It could also allow future studies to objectively evaluate the effectiveness of therapy directed towards itching, with consequent improvement in quality of life.[19]
Severity
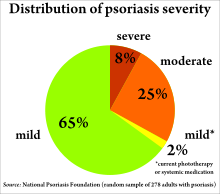
Psoriasis is usually graded as mild (affecting less than 3% of the body), moderate (affecting 3–10% of the body) or severe.[citation needed] Several scales exist for measuring the severity of psoriasis. The degree of severity is generally based on the following factors: the proportion of body surface area affected; disease activity (degree of plaque redness, thickness and scaling); response to previous therapies; and the impact of the disease on the person.
The Psoriasis Area Severity Index (PASI) is the most widely used measurement tool for psoriasis. PASI combines the assessment of the severity of lesions and the area affected into a single score in the range 0 (no disease) to 72 (maximal disease).[20] Nevertheless, the PASI can be too unwieldy to use outside of trials, which has led to attempts to simplify the index for clinical use.[21]
Cause
The cause of psoriasis is not fully understood. There are two main hypotheses about the process that occurs in the development of the disease. The first considers psoriasis as primarily a disorder of excessive growth and reproduction of skin cells. The problem is simply seen as a fault of the epidermis and its keratinocytes. The second hypothesis sees the disease as being an immune-mediated disorder in which the excessive reproduction of skin cells is secondary to factors produced by the immune system. T cells (which normally help protect the body against infection) become active, migrate to the dermis and trigger the release of cytokines (tumor necrosis factor-alpha TNFα, in particular) which cause inflammation and the rapid production of skin cells. It is not known what initiates the activation of the T cells.
The immune-mediated model of psoriasis has been supported by the observation that immunosuppressant medications can clear psoriasis plaques. However, the role of the immune system is not fully understood, and it has recently been reported that an animal model of psoriasis can be triggered in mice lacking T cells.[22] Animal models, however, reveal only a few aspects resembling human psoriasis.
Compromised skin barrier function has a role in psoriasis susceptibility.[23]
Psoriasis is a fairly idiosyncratic disease. The majority of people's experience of psoriasis is one in which it may worsen or improve for no apparent reason. Studies of the factors associated with psoriasis tend to be based on small (usually hospital based) samples of individuals. These studies tend to suffer from representative issues, and an inability to tease out causal associations in the face of other (possibly unknown) intervening factors. Conflicting findings are often reported. Nevertheless, the first outbreak is sometimes reported following stress (physical and mental), skin injury, and streptococcal infection. Conditions that have been reported as accompanying a worsening of the disease include infections, stress, and changes in season and climate. Certain medicines, including lithium salt, beta blockers and the antimalarial drug chloroquine have been reported to trigger or aggravate the disease. Excessive alcohol consumption, smoking and obesity may exacerbate psoriasis or make the management of the condition difficult or perhaps these comorbidities are effects rather than causes.[24][25] Hairspray, some face creams and hand lotions, can also cause an outbreak of psoriasis.[citation needed] In 1975, Stefania Jablonska and collaborators advanced a new theory that special antibodies tend to break through into the lower layers of the skin and set up a complex series of chemical reactions.[26]
Individuals suffering from the advanced effects of the human immunodeficiency virus, or HIV, often exhibit psoriasis.[27] This presents a paradox to researchers, as traditional therapies that reduce T-cell counts generally cause psoriasis to improve. Yet, as CD4-T-cell counts decrease with the progression of HIV, psoriasis worsens.[28] In addition, HIV is typically characterized by a strong Th2 cytokine profile, whereas psoriasis vulgaris is characterized by a strong Th1 secretion pattern.[29] It is hypothesized that the diminished CD4-T-Cell presence causes an overactivation of CD8-T-cells, which are responsible for the exacerbation of psoriasis in HIV positive patients. It is important to remember that most individuals with psoriasis are otherwise healthy, and the presence of HIV accounts for less than 1% of cases. The prevalence of psoriasis in the HIV positive population ranges from 1 to 6 percent, which is about three times higher than the normal population.[30] Psoriasis in AIDS sufferers is often severe, and untreatable with conventional therapy.[31]
Psoriasis occurs more likely in dry skin than oily or well-moisturized skin, and specifically after an external skin injury such as a scratch or cut (see Koebner phenomenon). This is believed to be caused by an infection, in which the infecting organism thrives under dry skin conditions with minimal skin oil, which otherwise protects skin from infections. The case for psoriasis is opposite to the case of athlete's foot, which occurs because of a fungus infection under wet conditions as opposed to dry in psoriasis. This infection induces inflammation, which causes the symptoms commonly associated with psoriasis, such as itching and rapid skin turnover, and leads to drier skin, as the infecting organism absorbs the moisture that would otherwise go to the skin. To prevent dry skin and reduce psoriasis symptoms, it is advised to not use shower scrubs, as they not only damage skin by leaving tiny scratches, but they also scrape off the naturally occurring skin oil. Additionally, moisturizers can be applied to moisturize the skin, and lotions used to promote skin oil gland functions.[citation needed]
Genetics
Psoriasis has a large hereditary component, and many genes are associated with it, but it is not clear how those genes work together. Most of them involve the immune system, particularly the major histocompatibility complex (MHC) and T cells. The main value of genetic studies is they identify molecular mechanisms and pathways for further study and potential drug targets.[32]
Classic genomewide linkage analysis has identified nine locations (loci) on different chromosomes associated with psoriasis. They are called psoriasis susceptibility 1 through 9 (PSORS1 through PSORS9). Within those loci are genes. Many of those genes are on pathways that lead to inflammation. Certain variations (mutations) of those genes are commonly found in psoriasis.[32]
The major determinant is PSORS1, which probably accounts for 35–50% of its heritability. It controls genes that affect the immune system or encode proteins that are found in the skin in greater amounts in psoriasis. PSORS1 is located on chromosome 6 in the MHC, which controls important immune functions. Three genes in the PSORS1 locus have a strong association with psoriasis vulgaris: HLA-C variant HLA-Cw6, which encodes a MHC class I protein; CCHCR1, variant WWC, which encodes a coiled protein that is overexpressed in psoriatic epidermis; and CDSM, variant allele 5, which encodes corneodesmosin, which is expressed in the granular and cornified layers of the epidermis and upregulated in psoriasis.[32]
Genome-wide association scans have identified other genes which are altered to characteristic variants in psoriasis. Some of these genes express inflammatory signal proteins, which affect cells in the immune system that are also involved in psoriasis. Some of these genes are also involved in other autoimmune diseases.[32]
Two major genes under investigation are IL12B on chromosome 5q, which expresses interleukin-12B; and IL23R on chromosome 1p, which expresses the interleukin-23 receptor, and is involved in T cell differentiation. T cells are involved in the inflammatory process that leads to psoriasis.[32]
These genes are on the pathway that ends up upregulating tumor necrosis factor-α and nuclear factor κB, two genes that are involved in inflammation.[32]
Immunology
In psoriasis, immune cells move from the dermis to the epidermis, where they stimulate skin cells (keratinocytes) to proliferate. Psoriasis does not seem to be a true autoimmune disease.[32] In an autoimmune disease, the immune system confuses an outside antigen with a normal body component, and attacks them both. But in psoriasis, the inflammation does not seem to be caused by outside antigens (although DNA does have an immunostimulatory effect). Researchers have identified many of the immune cells involved in psoriasis, and the chemical signals they send to each other to coordinate inflammation. At the end of this process, immune cells, such as dendritic cells and T cells, move from the dermis to the epidermis, secreting chemical signals, such as tumor necrosis factor-α, interleukin-1β, and interleukin-6, which cause inflammation, and interleukin-22, which causes keratinocytes to proliferate.[32]
The immune system consists of an innate immune system, and an adaptive immune system.
In the innate system, immune cells have receptors that have evolved to target specific proteins and other antigens which are commonly found on pathogens. In the adaptive immune system, immune cells respond to proteins and other antigens that they may never have seen before, which are presented to them by other cells. The innate system often passes antigens on to the adaptive system. When the immune system makes a mistake, and identifies a healthy part of the body as a foreign antigen, the immune system attacks that protein, as it does in autoimmunity.
In psoriasis, DNA is an inflammatory stimulus. DNA stimulates the receptors on plasmacytoid dendritic cells, which produce interferon-α, an immune stimulatory signal (cytokine). In psoriasis, keratinocytes produce antimicrobial peptides. In response to dendritic cells and T cells, they also produce cytokines, such as interleukin-1, interleukin-6, and tumor necrosis factor-α, which signals more inflammatory cells to arrive and produces further inflammation.[32]
Dendritic cells bridge the innate and adaptive immune system. They are increased in psoriatic lesions and induce the proliferation of T cells and type 1 helper T cells. Certain dendritic cells can produce tumor necrosis factor-α, which calls more immune cells and stimulates more inflammation. Targeted immunotherapy, and psoralen and ultraviolet A (PUVA) therapy, reduces the number of dendritic cells.[32]
T cells move from the dermis into the epidermis. They are attracted to the epidermis by alpha-1 beta-1 integrin, a signalling molecule on the collagen in the epidermis. Psoriatic T cells secrete interferon-γ and interleukin-17. Interleukin-17 is also associated with interleukin-22. Interleukin-22 induces keratocytes to proliferate.[32]
One hypothesis is that psoriasis involves a defect in regulatory T cells, and in the regulatory cytokine interleukin-10.[32]
Diagnosis
A diagnosis of psoriasis is usually based on the appearance of the skin; there are no special blood tests or diagnostic procedures. Sometimes, a skin biopsy, or scraping, may be needed to rule out other disorders and to confirm the diagnosis. Skin from a biopsy will show clubbed rete pegs if positive for psoriasis. Another sign of psoriasis is that when the plaques are scraped, one can see pinpoint bleeding from the skin below (Auspitz's sign).
Management
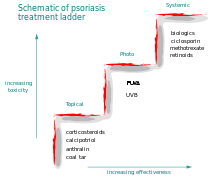
There are a number of different treatment options for psoriasis. Typically topical agents are used for mild disease, phototherapy for moderate disease, and systemic agents for severe disease.[33]
Topical agents
Bath solutions and moisturizers, mineral oil, and petroleum jelly may help soothe affected skin and reduce the dryness which accompanies the build-up of skin on psoriatic plaques. Medicated creams and ointments applied directly to psoriatic plaques can help reduce inflammation, remove built-up scale, reduce skin turn over, and clear affected skin of plaques. Ointment and creams containing coal tar, dithranol (anthralin), corticosteroids like desoximetasone (Topicort), fluocinonide, vitamin D3 analogues (for example, calcipotriol), and retinoids are routinely used. The use of the Finger tip unit may be helpful in guiding how much topical treatment to use.[34] The mechanism of action of each is probably different, but they all help to normalise skin cell production and reduce inflammation. Activated vitamin D and its analogues can inhibit skin cell proliferation.
Phototherapy
Phototherapy in the form of sunlight has long been used effectively for treatment.[33] Wavelengths of 311–313 nm are most effective and special lamps have been developed for this application.[33] The amount of light used is determined by a persons skin type.[33] Increased rates of cancer from treatment appear to be small.[33]
Psoralen and ultraviolet A phototherapy (PUVA) combines the oral or topical administration of psoralen with exposure to ultraviolet A (UVA) light. The mechanism of action of PUVA is unknown, but probably involves activation of psoralen by UVA light, which inhibits the abnormally rapid production of the cells in psoriatic skin. There are multiple mechanisms of action associated with PUVA, including effects on the skin immune system.
PUVA is associated with nausea, headache, fatigue, burning, and itching. Long-term treatment is associated with squamous cell carcinoma (but not with melanoma).[citation needed]
Systemic agents
 Pictures of a patient with psoriasis (and psoriatic arthritis) at baseline and 8 weeks after initiation of infliximab therapy.
Pictures of a patient with psoriasis (and psoriatic arthritis) at baseline and 8 weeks after initiation of infliximab therapy.
Psoriasis that is resistant to topical treatment and phototherapy is treated by medications taken internally by pill or injection (systemic). Patients undergoing systemic treatment are required to have regular blood and liver function tests because of the toxicity of the medication. Pregnancy must be avoided for the majority of these treatments. Most people experience a recurrence of psoriasis after systemic treatment is discontinued.
The three main traditional systemic treatments are methotrexate, cyclosporine and retinoids. Methotrexate and cyclosporine are immunosuppressant drugs; retinoids are synthetic forms of vitamin A. Patients taking methotrexate are prone to ulcerations. Post-surgical eventration may be associated to methotrexate exposure.[35]
Biologics are manufactured proteins that interrupt the immune process involved in psoriasis. Unlike generalised immunosuppressant therapies such as methotrexate, biologics focus on specific aspects of the immune function leading to psoriasis. These drugs (interleukin antagonists) are relatively new, and their long-term impact on immune function is unknown, but they have proven effective in treating psoriasis and psoriatic arthritis. Biologics are usually given by self-injection or in a doctor's office. In the United Kingdom in 2005, the British Association of Dermatologists (BAD) published guidelines for use of biological interventions in psoriasis.[36] A UK national register called the BAD Biological Register (BADBIR) has been set up to collect valuable information on side effects and benefits and will be used to inform doctors on how best to use biological agents and similar drugs.
Two drugs that target T cells are efalizumab and alefacept. Efalizumab is a monoclonal antibody which blocks the molecules that dendritic cells use to communicate with T cells. It also blocks the adhesion molecules on the endothelial cells that line blood vessels, which attract T cells. However, it suppressed the immune system's ability to control normally harmless viruses, which led to fatal brain infections. Efalizumab was voluntarily withdrawn from the US market in April, 2009 by the manufacturer. Alefacept also blocks the molecules that dendritic cells use to communicate with T cells and even causes natural killer cells to kill T cells as a way of controlling inflammation.[32]
Several monoclonal antibodies (MAbs) target cytokines, the molecules that cells use to send inflammatory signals to each other. TNF-α is one of the main executor inflammatory cytokines. Four MAbs (infliximab, adalimumab, golimumab and certolizumab pegol) and one recombinant TNF-α decoy receptor, etanercept, have been developed against TNF-α to inhibit TNF-α signaling. Additional monoclonal antibodies have been developed against pro-inflammatory cytokines IL-12/IL-23 and Interleukin-17 [37] and inhibit the inflammatory pathway at a different point than the anti-TNF-α antibodies.[32] IL-12 and IL-23 share a common domain, p40, which is the target of the recently FDA-approved ustekinumab. Ustekinumab (IL-12/IL-23 blocker) was shown to have higher efficacy than high-dose etanercept over a 12-week period in patients with psoriasis.[38]
In 2008, the FDA approved three new treatment options[39] available to psoriasis patients: 1) Taclonex Scalp, a new topical ointment for treating scalp psoriasis; 2) the Xtrac Velocity excimer laser system, which emits a high-intensity beam of ultraviolet light, can treat moderate to severe psoriasis; and 3) the biologic drug adalimumab (brand name Humira) was also approved to treat moderate to severe psoriasis. Adalimumab had already been approved to treat psoriatic arthritis. The most recent biologic drug that has been approved to treat moderate to severe psoriasis, as of 2010, is ustekinumab (brand name Stelara).
Medications with the least potential for adverse reactions are preferentially employed. If the treatment goal is not achieved, then therapies with greater potential toxicity may be used. Medications with significant toxicity are reserved for severe unresponsive psoriasis. This is called the psoriasis treatment ladder.[40] As a first step, medicated ointments or creams, called topical treatments, are applied to the skin. If topical treatment fails to achieve the desired goal, then the next step would be to expose the skin to ultraviolet (UV) radiation. This type of treatment is called phototherapy. The third step involves the use of medications which are taken internally by pill or injection. This approach is called systemic treatment.
A 2010 meta-analysis compares the change in Psoriasis Area and Severity Index (PASI) improvement from baseline in 22 trials. The combination therapy for moderate to severe psoriasis using psoralen with ultraviolet A (PUVA) plus acitretin shows a 97.3% PASI improvement from baseline. Therapy limitations need to be taken into consideration in the treatment of moderate to severe psoriasis, such as the increased risk of skin cancer with phototherapy and birth defects with acitretin.[41]
Alternative therapy
Some studies suggest psoriasis symptoms can be relieved by changes in diet[42] and lifestyle. Fasting periods, low energy diets and vegetarian diets have improved psoriasis symptoms in some studies,[43] and diets supplemented with fish oil (in this study cod liver oil) have also shown beneficial effects.[43] Fish oils are rich in the two omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) and contain Vitamin E, furthermore cod liver oil contains Vitamin A and Vitamin D.
The severity of psoriasis symptoms may also be influenced by lifestyle habits related to alcohol, smoking, weight, sleep, stress and exercise.[44]
It has been suggested that cannabis might treat psoriasis, due to the anti-inflammatory properties of its cannabinoids, and the regulatory effects of THC on the immune system.[45] The adverse effects of cannabis might be overcome by use of more specific cannabinoid receptor medications,[46] to inhibit keratinocyte proliferation.[47]
Prognosis
Psoriasis is typically a lifelong condition.[48] There is currently no cure, but various treatments can help to control the symptoms. Many of the most effective agents used to treat severe psoriasis carry an increased risk of significant morbidity including skin cancers, lymphoma and liver disease. However, the majority of people's experience of psoriasis is that of minor localized patches, particularly on the elbows and knees, which can be treated with topical medication. Psoriasis can get worse over time, but it is not possible to predict who will go on to develop extensive psoriasis or those in whom the disease may appear to vanish. Individuals will often experience flares and remissions throughout their lives. Controlling the signs and symptoms typically requires lifelong therapy.
According to one study,[49] psoriasis is linked to 2.5-fold increased risk for nonmelanoma skin cancer in men and women, with no preponderance of any specific histologic subtype of cancer. This increased risk could also be attributed to antipsoriatic treatment.
Epidemiology
Psoriasis affects both sexes equally, and can occur at any age, although it most commonly appears for the first time between the ages of 15 and 25 years.
The prevalence of psoriasis in Western populations is estimated to be around 2-3%. The prevalence of psoriasis among 7.5 million patients who were registered with a general practitioner in the United Kingdom was 1.5%.[50] A survey[51] conducted by the National Psoriasis Foundation (a US-based psoriasis education and advocacy group) found a prevalence of 2.1% among adult Americans. The study found 35% of people with psoriasis could be classified as having moderate to severe psoriasis.
Around one-third of people with psoriasis report a family history of the disease, and researchers have identified genetic loci associated with the condition. Studies of monozygotic twins suggest a 70% chance of a twin developing psoriasis if the other twin has psoriasis. The concordance is around 20% for dizygotic twins. These findings suggest both a genetic predisposition and an environmental response in developing psoriasis.[52]
Onset before age 40 usually indicates a greater genetic susceptibility and a more severe or recurrent course of psoriasis.
History
Psoriasis is probably one of the longest known illnesses of humans and simultaneously one of the most misunderstood.[citation needed] Some scholars believe psoriasis to have been included among the skin conditions called tzaraat in the Bible.[53] In more recent times psoriasis was frequently described as a variety of leprosy.[citation needed] The Greeks used the term lepra (λεπρα) for scaly skin conditions. They used the term psora to describe itchy skin conditions. It became known as Willan's lepra in the late 18th century when English dermatologists Robert Willan and Thomas Bateman differentiated it from other skin diseases. Leprosy, they said, is distinguished by the regular, circular form of patches, while psoriasis is always irregular. Willan identified two categories: leprosa graecorum and psora leprosa.[54]
It was not until 1841 that the condition was finally given the name psoriasis by the Viennese dermatologist Ferdinand von Hebra. The name is derived from the Greek word psora which means to itch.[55]
It was during the 20th century that psoriasis was further differentiated into specific types.[citation needed]
Historical treatment
The history of psoriasis is littered with treatments of dubious effectiveness and high toxicity. These treatments received brief popularity at particular time periods or within certain geographical regions. The application of cat faeces to red lesions on the skin, for example, was one of the earliest topical treatments employed in ancient Egypt. Onions, sea salt and urine, goose oil and semen, wasp droppings in sycamore milk, and soup made from vipers have all been reported as being ancient treatments.
In the more recent past, Fowler's solution, which contains a poisonous and carcinogenic arsenic compound, was used by dermatologists as a treatment for psoriasis during the 18th and 19th centuries. Grenz rays (also called ultrasoft X-rays or Bucky rays) was a popular treatment of psoriasis during the middle of the 20th century. This type of therapy was superseded by ultraviolet therapy.
Undecylenic acid was investigated and used for psoriasis some 40 years ago (circa 1950).[56]
All these treatments have fallen out of favour.
Sulphur was fashionable as a treatment for psoriasis in the Victorian and Edwardian eras. It has recently regained some credibility as a safe alternative to steroids and coal tar.[citation needed]
Research
Historically, agents used to treat psoriasis were discovered by experimentation or by accident. In contrast, current novel therapeutic agents are designed from a better understanding of the immune processes involved in psoriasis and by the specific targeting of molecular mediators. Examples can be seen in the use of biologics, which target T cells and TNF inhibitors.
Emerging clinical research has demonstrated the integral role of Janus kinase (JAK) proteins in the pathogenesis of psoriasis. As of 2010, two new oral JAK inhibitor drugs, ruxolitinib and tofacitinib (formerly called tasocitinib), have shown rapid and promising efficacy in Phase I/II trials with patients showing significant skin clearing within one week of beginning treatment.[57][58] Ruxolitimib has completed Phase II clinical trials supplied as a topical cream.[59]
Briakinumab is a human anti-IL-12/IL-23 monoclonal antibody directed against the shared p40 subunit of IL-12 and IL-23. Briakinumab is being developed by Abbott Laboratories in conjunction with Cambridge Antibody Technology for the treatment of multiple autoimmune diseases, including psoriasis. Abbott completed Phase III trials in 2010.[60] Despite successful trials, in January 2011 Abbott withdrew their biologic drug application from United States and European regulatory offices.[61]
Talarozole amplifies the effects of retinoic acid by inhibiting its metabolism. As of February 2009[update], it is undergoing clinical trials.[62]
Research into antisense oligonucleotides carries the potential to provide novel therapeutic strategies for treating psoriasis. Antisense oligonucleotides would be used to down regulate key cellular proteins known to play a role in psoriatic pathogenesis including inflammatory proteins such as ICAM-1 (intercellular adhesion molecule-1), IL-2 and IL-8, cellular proliferation proteins like insulin-like growth factor 1 receptor (IGF-IR) and epidermal growth factor and hyperangiogenesis vascular endothelial growth factor (VEGF).[63]
A novel boron-containing topical anti-inflammatory, AN2728, is currently being developed by Anacor Pharmaceuticals and is in Phase 2b trials for mild-to-moderate plaque type psoriasis.[64] The molecule works by inhibiting PDE4 and reducing the production of TNF-alpha, a precursor of the inflammation associated with psoriasis, as well as other cytokines, including IL-12 and IL-23.
Noting that botulinum toxin has been shown to have an effect on inhibiting neurogenic inflammation, and evidence suggesting the role of neurogenic inflammation in the pathogenesis of psoriasis,[65] the University of Minnesota has begun a clinical trial to follow up on the observation that patients treated with botulinum toxin for dystonia had dramatic improvement in psoriasis.[66]
In 2004, Tas and Avci demonstrated cyclopamine’s clinical potential for the treatment of psoriasis and basal cell carcinoma in two preliminary proof of concept studies.[67] By treating 31 psoriatic lesions in 7 patients, these authors asserted topical cyclopamine was more effective in the clinical and histological clearance of guttate and plaque psoriasis than the topical steroid clobetasol-17 propionate. Furthermore, they demonstrated concurrent application of cylopamine and clobetasol-17 propionate accelerated regression and clearance of selected lesions greater than cyclopamine alone, with clearance times as early as 48 hours. They assert cyclopamine inhibits the abnormal proliferation of epithelial cells, induces terminal differentiation, and is associated with the decreased presence of inflammatory cells, including CD41 lymphocytes.
On 27 August 2006, scientists led by Jeung-Hoon Lee created the synthetic lipids pseudoceramides, which are involved in skin cell growth, and could be used in treating skin diseases such as atopic dermatitis, a form of eczema characterized by red, flaky and very itchy skin; psoriasis, and glucocorticoid-induced epidermal atrophy, in which the skin shrinks due to skin cell loss.[68]
In children
Psoriasis can affect children. Approximately one third of psoriasis patients report being diagnosed before age 20.[69] Self-esteem and behavior can be affected by the disease. Bullying has been noted in clinical research.[70]
References
- ^ "Learn: About psoriasis". National Psoriasis Foundation. http://www.psoriasis.org/netcommunity/about_psoriasis.
- ^ "Psoriasis Linked to Stroke Risk". BBC. 28 August 2011. http://www.bbc.co.uk/news/health-14559523.
- ^ Committee for Medicinal Products for Human Use (CHMP) (18 November 2004). "Guideline on Clinical Investigation of Medicinal Products indicated for the treatment of Psoriasis" (PDF). European Medicines Agency. http://www.ema.europa.eu/pdfs/human/ewp/245402en.pdf.
- ^ http://www.psoriasis.org/learn_statistics Statistic from Psoriasis.org.
- ^ Cox, Neil; White, Gary (2000). Diseases of the skin: a color atlas and text. St. Louis: Mosby. ISBN 0-7234-3155-8.
- ^ see causes
- ^ url=http://kellypalace61.web.officelive.com/Documents/CorticosteriodAddictionArticle.pdf
- ^ http://web.ilds.org/icd10_list.php?VIEW=1&START_CODE=L40.0&START_EXT=00
- ^ "Application to dermatology of International Classification of Disease (ICD-10) — ICD sorted by code: L40.000–L41.000", The International League of Dermatological Societies
- ^ Freedberg, Irwin M.; Fitzpatrick, Thomas B. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York: McGraw-Hill. p. 414. ISBN 0-07-138076-0.
- ^ "Erythrodermic psoriasis", New Zealand Dermatological Society
- ^ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology (10th ed.). Saunders. p. 191–7. ISBN 0-7216-2921-0.
- ^ a b Zadik Y, Drucker S, Pallmon S (Aug 2011). "Migratory stomatitis (ectopic geographic tongue) on the floor of the mouth". J Am Acad Dermatol 65 (2): 459–60. doi:10.1016/j.jaad.2010.04.016. PMID 21763590. http://www.sciencedirect.com/science/article/pii/S0190962210004883.
- ^ Sampogna F, Chren MM, Melchi CF, Pasquini P, Tabolli S, Abeni D (February 2006). "Age, gender, quality of life and psychological distress in patients hospitalized with psoriasis". Br. J. Dermatol. 154 (2): 325–31. doi:10.1111/j.1365-2133.2005.06909.x. PMID 16433804. http://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0007-0963&date=2006&volume=154&issue=2&spage=325.
- ^ "Coping With Psoriasis" Parade.com
- ^ Bhosle MJ, Kulkarni A, Feldman SR, Balkrishnan R (2006). "Quality of life in patients with psoriasis". Health Qual Life Outcomes 4: 35. doi:10.1186/1477-7525-4-35. PMC 1501000. PMID 16756666. http://www.hqlo.com/content/4//35.
- ^ Globe D, Bayliss MS, Harrison DJ (2009). "The impact of itch symptoms in psoriasis: results from physician interviews and patient focus groups". Health Qual Life Outcomes 7: 62. doi:10.1186/1477-7525-7-62. PMC 2717072. PMID 19580674. http://www.hqlo.com/content/7//62.
- ^ Gottlieb A, Feng J, Harrison DJ, Globe D (October 2010). "Validation and response to treatment of a pruritus self-assessment tool in patients with moderate to severe psoriasis". J. Am. Acad. Dermatol. 63 (4): 580–6. doi:10.1016/j.jaad.2009.09.049. PMID 20599294. http://linkinghub.elsevier.com/retrieve/pii/S0190-9622(09)01346-2.
- ^ "Simple Psoriasis Pruritus Self-Assessment Tool Validated". Doctors Lounge. http://www.doctorslounge.com/index.php/news/pb/14435.
- ^ "Psoriasis Update -Skin & Aging". http://www.skinandaging.com/article/5394. Retrieved 2007-07-28.
- ^ Louden BA, Pearce DJ, Lang W, Feldman SR (2004). "A Simplified Psoriasis Area Severity Index (SPASI) for rating psoriasis severity in clinic patients". Dermatol. Online J. 10 (2): 7. PMID 15530297.
- ^ Zenz R, Eferl R, Kenner L, et al. (2005). "Psoriasis-like skin disease and arthritis caused by inducible epidermal deletion of Jun proteins". Nature 437 (7057): 369–75. doi:10.1038/nature03963. PMID 16163348.
- ^ de Cid R, Riveira-Munoz E, Zeeuwen PL, et al. (February 2009). "Deletion of the late cornified envelope LCE3B and LCE3C genes as a susceptibility factor for psoriasis". Nat. Genet. 41 (2): 211–5. doi:10.1038/ng.313. PMC 3128734. PMID 19169253. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3128734.
- ^ Psoriasis Triggers at Psoriasis Net. SkinCarePhysicians.com 9-28-05. American Academy of Dermatology, 2008.
- ^ Behnam SM, Behnam SE, Koo JY (2005). "Smoking and psoriasis". Skinmed 4 (3): 174–6. doi:10.1111/j.1540-9740.2005.03716.x. PMID 15891254. http://www.lejacq.com/articleDetail.cfm?pid=SKINmed_4;3:174.
- ^ Coleman, Lester L (November 30, 1975). "Your Health". Boca Raton News. http://news.google.com/newspapers?id=d9APAAAAIBAJ&sjid=WI0DAAAAIBAJ&pg=4808,3654533&dq.
- ^ Fife DJ, Waller JM, Jeffes EW, Koo JYM (18 May 2007). "Unraveling the Paradoxes of HIV-associated Psoriasis: A Review of T-cell Subsets and Cytokine Profiles". Dermatology Online Journal 13 (2). http://dermatology.cdlib.org/132/reviews/HIV/fife.html. at Medscape
- ^ Ortonne JP, Lebwohl M, Em Griffiths C (2003). "Alefacept-induced decreases in circulating blood lymphocyte counts correlate with clinical response in patients with chronic plaque psoriasis". Eur J Dermatol 13 (2): 117–23. PMID 12695125. http://www.john-libbey-eurotext.fr/medline.md?issn=1167-1122&vol=13&iss=2&page=117.
- ^ Austin LM, Ozawa M, Kikuchi T, Walters IB, Krueger JG (November 1999). "The majority of epidermal T cells in Psoriasis vulgaris lesions can produce type 1 cytokines, interferon-gamma, interleukin-2, and tumor necrosis factor-alpha, defining TC1 (cytotoxic T lymphocyte) and TH1 effector populations: a type 1 differentiation bias is also measured in circulating blood T cells in psoriatic patients". J. Invest. Dermatol. 113 (5): 752–9. doi:10.1046/j.1523-1747.1999.00749.x. PMID 10571730.
- ^ [1] A Case Report of Severe Psoriasis in a Patient with AIDS: The Role of the HIV Virus and the Therapeutic Challenges Involved. Vol: 13 No 2, 2002. National Skin Center. Retrieved 05-13-08.
- ^ "Images of Memorable Cases: Case 34". Connexions. Rice University. http://cnx.org/content/m14956/latest/. "This AIDS patient presented with a pruritic eruption over most of his body"
- ^ a b c d e f g h i j k l m n Nestle FO, Kaplan DH, Barker J (July 2009). "Psoriasis". N. Engl. J. Med. 361 (5): 496–509. doi:10.1056/NEJMra0804595. PMID 19641206. http://content.nejm.org/cgi/content/full/361/5/496. Review article: Mechanisms of Disease.
- ^ a b c d e Menter A, Griffiths CE (July 2007). "Current and future management of psoriasis". Lancet 370 (9583): 272–84. doi:10.1016/S0140-6736(07)61129-5. PMID 17658398.
- ^ Menter, Alan; Gottlieb, Alice; Feldman, Steven R.; Van Voorhees, Abby S.; Leonardi, Craig L.; Gordon, Kenneth B.; Lebwohl, Mark; Koo, John Y. M. et al. (2009). "Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 3". J. Am. Acad. Dermatol. 60 (4): 643–659. doi:10.1016/j.jaad.2008.12.032.
- ^ Conte H, Ezzedine K, Jouary T, Hubiche T, Taieb A, Milpied B (January 2010). "Eventration caused by methotrexate in a psoriatic patient". J Eur Acad Dermatol Venereol 24 (1): 76–7. doi:10.1111/j.1468-3083.2009.03269.x. PMID 19453786.
- ^ Smith CH, Anstey AV, Barker JN, et al. (September 2005). "British Association of Dermatologists guidelines for use of biological interventions in psoriasis 2005". Br. J. Dermatol. 153 (3): 486–97. doi:10.1111/j.1365-2133.2005.06893.x. PMID 16120132. http://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0007-0963&date=2005&volume=153&issue=3&spage=486.
- ^ Hueber W, Patel DD, Dryja T, et al. (October 2010). "Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis". Sci Transl Med 2 (52): 52ra72. doi:10.1126/scitranslmed.3001107. PMID 20926833.
- ^ Griffiths CE, Strober BE, van de Kerkhof P, et al. (January 2010). "Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis". N. Engl. J. Med. 362 (2): 118–28. doi:10.1056/NEJMoa0810652. PMID 20071701.
- ^ "Psoriasis Medical Breakthroughs" Parade.com
- ^ Lofholm PW (2000). "The psoriasis treatment ladder: a clinical overview for pharmacists". US Pharm 25 (5): 26–47. http://www.uspharmacist.com/oldformat.asp?url=newlook/files/Feat/apr00pro.cfm&pub_id=8&article_id=511.
- ^ Hankin CS, Bhatia ND, Goldenberg G, et al. (2010). "A Comparison of the Clinical Effectiveness and Cost-Effectiveness of Treatments for Moderate to Severe Psoriasis". Drug Benefit Trends 21: 17–27. http://dbt.consultantlive.com/display/article/1145628/1524557.
- ^ http://www.ijdvl.com/article.asp?issn=0378-6323;year=2010;volume=76;issue=2;spage=103;epage=115;aulast=Kaimal#Psoriasis Sowmya Kaimal, Devinder Mohan Thappa Diet in dermatology: Revisited Review 2010 | Volume : 76 | Issue : 2 | Page : 103-115
- ^ a b Wolters M (October 2005). "Diet and psoriasis: experimental data and clinical evidence". Br J Dermatol 153 (4): 706–714. doi:10.1111/j.1365-2133.2005.06781.x. PMID 16181450. http://www.medscape.com/viewarticle/514108.
- ^ Treloar V (2010). "Integrative dermatology for psoriasis: facts and controversies". Clinics in Dermatology 28 (1): 93–99. doi:10.1016/j.clindermatol.2009.03.016. PMID 20082958. http://www.ncbi.nlm.nih.gov/pubmed/20082958.
- ^ Namazi MR (2005). "Cannabinoids, loratadine and allopurinol as novel additions to the antipsoriatic ammunition". J Eur Acad Dermatol Venereol 19 (3): 319–22. doi:10.1111/j.1468-3083.2004.01184.x. PMID 15857457.
- ^ Fowler CJ (2005). "Pharmacological properties and therapeutic possibilities for drugs acting upon endocannabinoid receptors". Current drug targets. CNS and neurological disorders 4 (6): 685–96. doi:10.2174/156800705774933041. PMID 16375686.
- ^ Wilkinson JD, Williamson EM (2007). "Cannabinoids inhibit human keratinocyte proliferation through a non-CB1/CB2 mechanism and have a potential therapeutic value in the treatment of psoriasis". J. Dermatol. Sci. 45 (2): 87–92. doi:10.1016/j.jdermsci.2006.10.009. PMID 17157480.
- ^ Jobling R (2007). "A patient's journey:Psoriasis". Br Med J 334 (7600): 953–4. doi:10.1136/bmj.39184.615150.802. PMC 1865393. PMID 17478850. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1865393.
- ^ Olsen JH, Frentz G, Møller H (1993). "[Psoriasis and cancer]" (in Danish). Ugeskr. Laeg. 155 (35): 2687–91. PMID 8212383.
- ^ Gelfand JM et al. (2005). "Prevalence and Treatment of Psoriasis in the United Kingdom". Arch. Dermatol. 141 (12): 1537–1541. doi:10.1001/archderm.141.12.1537. PMID 16365254.
- ^ "Benchmark Survey on Psoriasis and Psoriatic Arthritis: Summary of Top-Line Results" (PDF). National Psoriasis Foundation. http://www.psoriasis.org/files/pdfs/press/npfsurvey.pdf.
- ^ Krueger G, Ellis CN (2005). "Psoriasis--recent advances in understanding its pathogenesis and treatment". J. Am. Acad. Dermatol. 53 (1 Suppl 1): S94–100. doi:10.1016/j.jaad.2005.04.035. PMID 15968269.
- ^ Shai A, Vardy D, Zvulunov A (2002). "[Psoriasis, biblical afflictions and patients' dignity]" (in Hebrew). Harefuah 141 (5): 479–82, 496. PMID 12073533.
- ^ Meenan FO (March 1955). "A note on the history of psoriasis". Ir J Med Sci (351): 141–2. PMID 14353580.
- ^ Glickman FS (1986). "Lepra, psora, psoriasis". J. Am. Acad. Dermatol. 14 (5 Pt 1): 863–6. doi:10.1016/S0190-9622(86)70101-1. PMID 3519699.
- ^ Ereaux L, Craig G (October 1949). "The Oral Administration Of Undecylenic Acid In The Treatment Of Psoriasis". Canad. M. A. J. 61 (4): 361–4. PMC 1591667. PMID 18140580. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1591667. Retrieved 2007-01-05. — see page 4/364 of link
- ^ Mesa RA (June 2010). "Ruxolitinib, a selective JAK1 and JAK2 inhibitor for the treatment of myeloproliferative neoplasms and psoriasis". IDrugs 13 (6): 394–403. PMID 20506062.
- ^ Boy MG, Wang C, Wilkinson BE, et al. (September 2009). "Double-blind, placebo-controlled, dose-escalation study to evaluate the pharmacologic effect of CP-690,550 in patients with psoriasis". J. Invest. Dermatol. 129 (9): 2299–302. doi:10.1038/jid.2009.25. PMID 19225543.
- ^ ClinicalTrials.gov NCT00778700 A Dose Ranging Study of the Effect of INCB018424 Phosphate Cream When Applied to Patients With Plaque Psoriasis
- ^ ClinicalTrials.gov 10 studies with search of: ABT-874
- ^ Krauskopf L (14 January 2011). "Abbott withdraws applications for psoriasis drug". Reuters. http://www.reuters.com/article/idUSN1415033420110114.
- ^ Giltaire, S; Herphelin F, Frankart A, Hérin M, Stoppie P, Poumay Y (11 December 2008). "The CYP26 inhibitor R115866 potentiates the effects of all-trans retinoic acid on cultured human epidermal keratinocytes". Br J Dermatol 160 (3): 505–13. doi:10.1111/j.1365-2133.2008.08960.x. PMID 19120344.
- ^ White PJ, Atley LM, Wraight CJ (2004). "Antisense oligonucleotide treatments for psoriasis". Expert opinion on biological therapy 4 (1): 75–81. doi:10.1517/14712598.4.1.75. PMID 14680470.
- ^ >ClinicalTrials.gov NCT01300052
- ^ Saraceno, R; Kleyn, CE; Terenghi, G; Griffiths, CE (2006). "The role of neuropeptides in psoriasis". The British Journal of Dermatology 155 (5): 876–82. doi:10.1111/j.1365-2133.2006.07518.x. PMID 17034513.
- ^ ClinicalTrials.gov NCT00816517 Use of Botulinum Toxin to Treat Psoriasis
- ^ Tas, S.; Avci, O. (2004). "Rapid clearance of psoriatic skin lesions induced by topical cyclopamine". Dermatology 209 (2): 126–131. doi:10.1159/000079596. PMID 15316166.
- ^ Science Daily, New Skin-healing Chemicals
- ^ Benoit, Sandrine; Hamm, Henning (2007). "Childhood Psoriasis". Clinics in Dermatology 25 (6): 555–562. doi:10.1016/j.clindermatol.2007.08.009. PMID 18021892.
- ^ Magin, Parker; Adams, Jon; Heading, Gaynor; Pond, Dimity; Smith, Wayne (2008). "Experiences of appearance-related teasing and bullying in skin diseases and their psychological sequelae: results of a qualitative study". Scandinavian Journal of Caring Sciences 22 (3): 430–436. doi:10.1111/j.1471-6712.2007.00547.x. PMID 18840226.
Further reading
- Baker, Barbara S. (2008). From Arsenic to Biologicals: A 200 Year History of Psoriasis. Beckenham, UK: Garner Press. ISBN 0955160324.
External links
- National Psoriasis Foundation
- Psoriasis at the Open Directory Project
- Patient information: Psoriasis
Papulosquamous disorders (L40–L45, 696–697) Psoriasis PustularGeneralized pustular psoriasis (Impetigo herpetiformis) · Acropustulosis/Pustulosis palmaris et plantaris (Pustular bacterid) · Annular pustular psoriasis · Localized pustular psoriasisOtherParapsoriasis Pityriasis lichenoides (Pityriasis lichenoides et varioliformis acuta, Pityriasis lichenoides chronica) · Lymphomatoid papulosis · Small plaque parapsoriasis (Digitate dermatosis, Xanthoerythrodermia perstans) · Large plaque parapsoriasis (Retiform parapsoriasis)Other pityriasis Other lichenoid configuration: Annular lichen planus · Linear lichen planus
morphology of lesion: Hypertrophic lichen planus · Atrophic lichen planus · Bullous lichen planus · Ulcerative lichen planus · Lichen planus actinicus · Lichen planus pigmentosus
site of involvement: Mucosal lichen planus · Lichen planus of the nails · Peno-gingival syndrome · Vulvovaginal gingival syndromeoverlap: Lichen planus–lichen sclerosus overlap syndrome · Lichen planus–lupus erythematosus overlap syndrome
special forms: Hepatitis-associated lichen planus · Lichen planus pemphigoidesOtherungrouped lichenoid eruptions: Erythema dyschromicum perstans · Idiopathic eruptive macular pigmentation · Keratosis lichenoides chronica · Kraurosis vulvae · Lichen sclerosus · Lichenoid dermatitis · Lichenoid reaction of graft-versus-host diseaseCategories:- Psoriasis
- Autoimmune diseases
Wikimedia Foundation. 2010.