- Histoplasmosis
-
Histoplasmosis Classification and external resources 
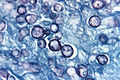
Histoplasma capsulatum. Methenamine silver stain showing histopathologic changes in histoplasmosis.ICD-10 B39 ICD-9 115 DiseasesDB 5925 MedlinePlus 001082 eMedicine med/1021 ped/1017 MeSH D006660 Histoplasmosis (also known as "Cave disease,"[1] "Darling's disease,"[1] "Ohio valley disease,"[1] "Reticuloendotheliosis,"[1] "Spelunker’s Lung" and Caver's disease) is a disease caused by the fungus Histoplasma capsulatum. Symptoms of this infection vary greatly, but the disease primarily affects the lungs.[2] Occasionally, other organs are affected; this is called disseminated histoplasmosis, and it can be fatal if left untreated. Histoplasmosis is common among AIDS patients because of their suppressed immune system.[3]
Contents
Symptoms
 Chest X-ray of a patient with acute pulmonary histoplasmosis.
Chest X-ray of a patient with acute pulmonary histoplasmosis.
If symptoms of histoplasmosis infection occur, they will start within 3 to 17 days after exposure; the average is 12–14 days. Most affected individuals have clinically silent manifestations and show no apparent ill effects.[4] The acute phase of histoplasmosis is characterized by non-specific respiratory symptoms, often cough or flu-like. Chest X-ray findings are normal in 40–70% of cases.[4] Chronic histoplasmosis cases can resemble tuberculosis;[5][6] disseminated histoplasmosis affects multiple organ systems and is fatal unless treated.[7]
While histoplasmosis is the most common cause of mediastinitis, this remains a relatively rare disease. Severe infections can cause hepatosplenomegaly, lymphadenopathy, and adrenal enlargement.[2] Lesions have a tendency to calcify as they heal. Ocular histoplasmosis damages the retina of the eyes. Scar tissue is left on the retina which can experience leakage, resulting in a loss of vision not unlike macular degeneration.[citation needed]
Types
Histoplasmosis may be divided into the following types:[8]:316-317
-
- Primary pulmonary histoplasmosis
- Progressive disseminated histoplasmosis
- Primary cutaneous histoplasmosis
- African histoplasmosis
Epidemiology
Histoplasma capsulatum is found throughout the world. It is endemic in certain areas of the United States, particularly in states bordering the Ohio River valley and the lower Mississippi River. It also common in caves in southern and East Africa. Positive histoplasmin skin tests occur in as many as 90% of the people living in areas where H. capsulatum is common, such as the eastern and central United States.[2]
Disease mechanism
H. capsulatum grows in soil and material contaminated with bird or bat droppings (guano). The fungus has been found in poultry house litter, caves, areas harboring bats, and in bird roosts (particularly those of starlings). The fungus is thermally dimorphic: in the environment it grows as a brownish mycelium, and at body temperature (37 °C in humans) it morphs into a yeast. The inoculum is represented principally by microconidia that, once inhaled into the alveolar spaces, germinate and then transform into budding yeast cells. Histoplasmosis is not contagious, but is contracted by inhalation of the spores from disturbed soil or guano.[2]
Diagnosis
Histoplasmosis can be diagnosed by samples containing the fungus taken from sputum, blood, or infected organs. It can also be diagnosed by detection of antigens in blood or urine samples by ELISA or PCR. It can also be diagnosed by a test for antibodies against Histoplasma in the blood. Histoplasma skin tests indicate whether a person has been exposed, but do not indicate whether they have the disease.[2] Formal histoplasmosis diagnoses are often confirmed only by culturing the fungus directly.[3] Cutaneous manifestations of disseminated disease are diverse and often present as a nondescript rash with systemic complaints. Diagnosis is best established by histopathologic examination with appropriate stains for fungal organisms.[9]
Prevention
It is not practical to test or decontaminate most sites that may be contaminated with H. capsulatum, but the following sources list environments where histoplasmosis is common, and precautions to reduce a person's risk of exposure, in the three parts of the world where the disease is prevalent. Precautions common to all geographical locations would be to avoid accumulations of bird or bat droppings.
- The government of the USA provides a document, Histoplasmosis: Protecting Workers at Risk, which contains information on work practices and personal protective equipment that will reduce the risk of infection.
- Histoplasmosis is common in some Spanish speaking regions; the above document is also available in Spanish: La Protección de los Trabajadores que Tienen un Riesgo de HISTOPLASMOSIS.
- Authors at the University of Nigeria have published a review which includes information on locations in which histoplasmosis has been found in Africa (in chicken runs, bats and the caves bats infest, and in soil), and a thorough reference list including English, French, and Spanish language references.[10]
Treatment
Antifungal medications are used to treat severe cases of acute histoplasmosis and all cases of chronic and disseminated disease. Typical treatment of severe disease first involves treatment with amphotericin B, followed by oral itraconazole.[11] Treatment with itraconazole will need to continue for at least a year in severe cases.[12]
In many milder cases, oral itraconazole or ketoconazole is sufficient. Asymptomatic disease is typically not treated. Past infection results in partial protection against ill effects if reinfected.
History
Histoplasma was discovered in 1905 by Darling,[13] but was only discovered to be a widespread infection in the 1930s. Before then, many cases of histoplasmosis were mistakenly attributed to tuberculosis, and patients were mistakenly admitted to tuberculosis sanatoriums. Some patients contracted tuberculosis in these sanatoriums (reference: Mandell, Bennett and Dolin).
Society and culture
- Johnny Cash included a reference to the disease, even correctly noting its source in bird droppings, in the song "Beans for Breakfast".[14]
- Bob Dylan was hospitalized due to histoplasmosis in 1997, causing the cancellation of concerts in the United Kingdom and Switzerland.[15]
- In episode 21 of season 3 of the television show House, M.D. a patient was diagnosed with histoplasmosis.[16]
- In episode 5 of season 1 of the television show Dexter, C.S. Lee gets worried about getting histoplasmosis from the dust in the air and the hair of the rats.
Additional images
References
- ^ a b c d Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ^ a b c d e Ryan KJ, Ray CG, ed (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 674–6. ISBN 0-8385-8529-9.
- ^ a b Cotran RS, Kumar V, Fausto N, Robbins SL, Abbas AK (2005). Robbins and Cotran Pathologic Basis of Disease. St. Louis: Elsevier/Saunders. pp. 754–5. ISBN 0-7216-0187-1.
- ^ a b Silberberg P (2007-03-26). "Radiology Teaching Files: Case 224856 (Histoplasmosis)". http://www.mypacs.net/cases/HISTOPLASMOSIS-224856.html. Retrieved 2007-07-27.
- ^ Tong P, Tan WC, Pang M (1983). "Sporadic disseminated histoplasmosis simulating miliary tuberculosis". Br Med J (Clin Res Ed) 287 (6395): 822–3. doi:10.1136/bmj.287.6395.822. PMC 1549119. PMID 6412842. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1549119.
- ^ Gari-Toussaint, Marty P, Le Fichoux Y, Loubière R (1987). "Histoplasmose d'importation à Histoplasma capsulatum, données biocliniques et thérapeutiques variées, à propos de trois cas observés dans les Alpes maritimes". Bull Soc Fr Mycol Med 16 (1): 87–90. http://www.scribd.com/full/6931699?access_key=key-1q4cq6j8cywaani3s539.
- ^ Kauffman, CA (January 2007). "Histoplasmosis: a clinical and laboratory update". Clinical Microbiology Reviews 20 (1): 115–132. doi:10.1128/CMR.00027-06. PMC 1797635. PMID 17223625. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1797635.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ^ Rosenberg JD, Scheinfeld NS (December 2003). "Cutaneous histoplasmosis in patients with acquired immunodeficiency syndrome". Cutis 72 (6): 439–45. PMID 14700213.
- ^ Gugnani, HC; Muotoe-Okafor, F (1997). "African histoplasmosis: a review". Rev Iberoam Micol 14 (4): 155–159. PMID 15538817. http://www.reviberoammicol.com/1997-14/155159.pdf.
- ^ Histoplasmosis: Fungal Infections at Merck Manual of Diagnosis and Therapy Home Edition
- ^ Barron MA and Madinger NE (November 18, 2008). "Opportunistic Fungal Infections, Part 3: Cryptococcosis, Histoplasmosis, Coccidioidomycosis, and Emerging Mould Infections". Infections in Medicine. http://www.consultantlive.com/infection/article/1145625/1404367.
- ^ Darling ST (1906). "A protozoan general infection producing pseudotubercles in the lungs and focal necrosis in the liver, spleen and lymphnodes". J Am Med Assoc 46: 1283–5. http://www.bium.univ-paris5.fr/histmed/medica/cote?epo0215.
- ^ Beans for Breakfast lyrics
- ^ CNN - Bob Dylan hospitalized with Histoplasmosis
- ^ House episode "Family"
External links
- Histoplasmosis Resource Guide from the National Eye Institute (NEI).
- NIOSH - Histoplasmosis - Protecting Workers at Risk
- CDC Disease Info histoplasmosis
Infectious diseases · Mycoses and Mesomycetozoea (B35–B49, 110–118) Superficial and
cutaneous
(dermatomycosis):
Tinea=skin;
Piedra (exothrix/
endothrix)=hairBy locationTinea barbae/Tinea capitis (Kerion) · Tinea corporis (Ringworm, Dermatophytid) · Tinea cruris · Tinea manuum · Tinea pedis (Athlete's foot) · Tinea unguium/Onychomycosis (White superficial onychomycosis · Distal subungual onychomycosis · Proximal subungual onychomycosis)
Tinea corporis gladiatorum · Tinea faciei · Tinea imbricata · Tinea incognito · FavusBy organismEpidermophyton floccosum · Microsporum canis · Microsporum audouinii · Trichophyton interdigitale/mentagrophytes · Trichophyton tonsurans · Trichophyton schoenleini · Trichophyton rubrumOtherHortaea werneckii (Tinea nigra) · Piedraia hortae (Black piedra)Subcutaneous,
systemic,
and opportunisticDimorphic
(yeast+mold)Coccidioides immitis/Coccidioides posadasii (Coccidioidomycosis, Disseminated coccidioidomycosis, Primary cutaneous coccidioidomycosis. Primary pulmonary coccidioidomycosis) · Histoplasma capsulatum (Histoplasmosis, Primary cutaneous histoplasmosis, Primary pulmonary histoplasmosis, Progressive disseminated histoplasmosis) · Histoplasma duboisii (African histoplasmosis) · Lacazia loboi (Lobomycosis) · Paracoccidioides brasiliensis (Paracoccidioidomycosis)OtherBlastomyces dermatitidis (Blastomycosis, North American blastomycosis, South American blastomycosis) · Sporothrix schenckii (Sporotrichosis) · Penicillium marneffei (Penicilliosis)Yeast-likeCandida albicans (Candidiasis, Oral, Esophageal, Vulvovaginal, Chronic mucocutaneous, Antibiotic candidiasis, Candidal intertrigo, Candidal onychomycosis, Candidal paronychia, Candidid, Diaper candidiasis, Congenital cutaneous candidiasis, Perianal candidiasis, Systemic candidiasis, Erosio interdigitalis blastomycetica) · C. glabrata · C. tropicalis · C. lusitaniae · Pneumocystis jirovecii (Pneumocystosis, Pneumocystis pneumonia)Mold-likeAspergillus (Aspergillosis, Aspergilloma, Allergic bronchopulmonary aspergillosis, Primary cutaneous aspergillosis) · Exophiala jeanselmei (Eumycetoma) · Fonsecaea pedrosoi/Fonsecaea compacta/Phialophora verrucosa (Chromoblastomycosis) · Geotrichum candidum (Geotrichosis) · Pseudallescheria boydii (Allescheriasis)Entomophthorales
(Entomophthoramycosis)Basidiobolus ranarum (Basidiobolomycosis) · Conidiobolus coronatus/Conidiobolus incongruus (Conidiobolomycosis)Enterocytozoon bieneusi/Encephalitozoon intestinalisMesomycetozoea Ungrouped Alternariosis · Fungal folliculitis · Fusarium (Fusariosis) · Granuloma gluteale infantum · Hyalohyphomycosis · Otomycosis · PhaeohyphomycosisCategories:- Fungal diseases
- Mycosis-related cutaneous conditions
- Rare diseases
-
Wikimedia Foundation. 2010.