- Presumed ocular histoplasmosis syndrome
-
Presumed ocular histoplasmosis syndrome Classification and external resources 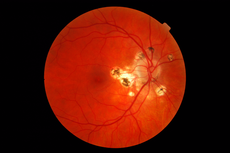
DiseasesDB 31279 eMedicine oph/406 Presumed ocular histoplasmosis syndrome (POHS) is a disease syndrome affecting the eye that is characterized by peripheral atrophic chorioretinal scars, atrophy or scarring adjacent to the optic disc and maculopathy.
The loss of vision in POHS is caused by choroidal neovascularization.
Contents
Causes
It is thought to be caused by Histoplasma capsulatum, but the fungus has rarely been isolated from cases with POHS.
The word "presumed" is also emphasized because the condition has also been found in locations where histoplasmosis is rare.[1]
Diagnosis
Fluorescein angiography is required for diagnosis and follow-up of patients with POHS.
Treatment
Treatment requires careful consideration of FA findings and few cases may respond to corticosteroids and laser photocoagulation. A vitreo-retinal specialist should be consulted for proper management of the case.
Presumed ocular histoplasmosis syndrome and age-related macular degeneration (AMD) have been successfully treated by the drug Bevacizumab (trade name Avastin, Genentech/Roche).[2] Ophthalmologists are using Avastin "off-label"[3] to treat AMD and similar conditions since research indicates that vascular endothelial growth factor (VEGF) is one of the causes for the growth of the abnormal vessels that cause these conditions. Some patients treated with Avastin had less fluid and more normal-appearing maculas, and their vision improved. Avastin injections into the affected eye have been used by retina specialists since early 2005. Thus there is no long term 10 to 15 year follow up data for possible late complications.[4] Early treatment is critical to maintaining vision.
Other treatments include Ranibizumab (trade name Lucentis) which is approved by the FDA for intraocular use. Lucentis uses a smaller molecule compared to Avastin and according to GenenTech, the smaller molecule helps lower the systemic toxicity of the drug, thereby lowering the overall risks compared to Avastin.[5] However, Lucentis costs approximately $1,600 per injection compared to less than $100 per injection for Avastin. Research has shown[6] that Avastin and Lucentis to be equally effective in the treatment of POHS and AMD.
External links
References
- ^ Stefan Dithmar; Frank Gerhard Holz (28 April 2008). Fluorescence Angiography in Ophthalmology. Springer. pp. 168–. ISBN 9783540783596. http://books.google.com/books?id=ebTzQKwQuNEC&pg=PA168. Retrieved 29 June 2010.
- ^ Ehrlich R, Ciulla TA, Maturi R, et al. (2009). "Intravitreal bevacizumab for choroidal neovascularization secondary to presumed ocular histoplasmosis syndrome". Retina (Philadelphia, Pa.) 29 (10): 1418–23. doi:10.1097/IAE.0b013e3181babdf1. PMID 19898179. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0275-004X&volume=29&issue=10&spage=1418.
- ^ AMDsupport.ca
- ^ The Retina Group of Washington: "Informed Consent for Avastin (Bevacizumab) Intravitreal Injection, Feb. 2006.
- ^ "Off-Label Avastin Treatment for Macular Degeneration", Macular Degeneration Support Canada. Published April 18, 2008, AMDsupport.ca
- ^ "Lucentis vs Avastin: Which Drug is Better?", Macular Degeneration Support Canada, Published August 10, 2009, AMDsupport.ca
Infectious diseases · Mycoses and Mesomycetozoea (B35–B49, 110–118) Superficial and
cutaneous
(dermatomycosis):
Tinea=skin;
Piedra (exothrix/
endothrix)=hairBy locationTinea barbae/Tinea capitis (Kerion) · Tinea corporis (Ringworm, Dermatophytid) · Tinea cruris · Tinea manuum · Tinea pedis (Athlete's foot) · Tinea unguium/Onychomycosis (White superficial onychomycosis · Distal subungual onychomycosis · Proximal subungual onychomycosis)
Tinea corporis gladiatorum · Tinea faciei · Tinea imbricata · Tinea incognito · FavusBy organismEpidermophyton floccosum · Microsporum canis · Microsporum audouinii · Trichophyton interdigitale/mentagrophytes · Trichophyton tonsurans · Trichophyton schoenleini · Trichophyton rubrumOtherHortaea werneckii (Tinea nigra) · Piedraia hortae (Black piedra)Subcutaneous,
systemic,
and opportunisticDimorphic
(yeast+mold)Coccidioides immitis/Coccidioides posadasii (Coccidioidomycosis, Disseminated coccidioidomycosis, Primary cutaneous coccidioidomycosis. Primary pulmonary coccidioidomycosis) · Histoplasma capsulatum (Histoplasmosis, Primary cutaneous histoplasmosis, Primary pulmonary histoplasmosis, Progressive disseminated histoplasmosis) · Histoplasma duboisii (African histoplasmosis) · Lacazia loboi (Lobomycosis) · Paracoccidioides brasiliensis (Paracoccidioidomycosis)OtherBlastomyces dermatitidis (Blastomycosis, North American blastomycosis, South American blastomycosis) · Sporothrix schenckii (Sporotrichosis) · Penicillium marneffei (Penicilliosis)Yeast-likeCandida albicans (Candidiasis, Oral, Esophageal, Vulvovaginal, Chronic mucocutaneous, Antibiotic candidiasis, Candidal intertrigo, Candidal onychomycosis, Candidal paronychia, Candidid, Diaper candidiasis, Congenital cutaneous candidiasis, Perianal candidiasis, Systemic candidiasis, Erosio interdigitalis blastomycetica) · C. glabrata · C. tropicalis · C. lusitaniae · Pneumocystis jirovecii (Pneumocystosis, Pneumocystis pneumonia)Mold-likeAspergillus (Aspergillosis, Aspergilloma, Allergic bronchopulmonary aspergillosis, Primary cutaneous aspergillosis) · Exophiala jeanselmei (Eumycetoma) · Fonsecaea pedrosoi/Fonsecaea compacta/Phialophora verrucosa (Chromoblastomycosis) · Geotrichum candidum (Geotrichosis) · Pseudallescheria boydii (Allescheriasis)Entomophthorales
(Entomophthoramycosis)Basidiobolus ranarum (Basidiobolomycosis) · Conidiobolus coronatus/Conidiobolus incongruus (Conidiobolomycosis)Enterocytozoon bieneusi/Encephalitozoon intestinalisMesomycetozoea Ungrouped Alternariosis · Fungal folliculitis · Fusarium (Fusariosis) · Granuloma gluteale infantum · Hyalohyphomycosis · Otomycosis · PhaeohyphomycosisCategories:- Diseases of the eye and adnexa
- Eye stubs
Wikimedia Foundation. 2010.
