- Cryptococcosis
-
Cryptococcosis Classification and external resources 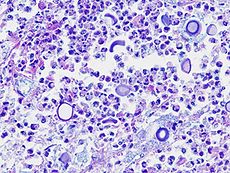
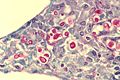
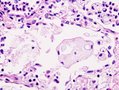
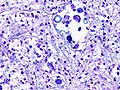
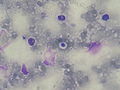
Histopathological image of pulmonary cryptococcosis in an immunocompromised host. Alcian blue-PAS stain.ICD-10 B45 ICD-9 117.5 DiseasesDB 3213 eMedicine med/482 MeSH D003453 Cryptococcosis, or cryptococcal disease, is a potentially fatal fungal disease. It is caused by one of two species; Cryptococcus neoformans and Cryptococcus gattii. These were all previously thought to be subspecies of C. neoformans, but have now been identified as distinct species.
Cryptococcosis is believed to be acquired by inhalation of the infectious propagule from the environment. Although the exact nature of the infectious propagule is unknown, the leading hypothesis is the basidiospore created through sexual or asexual reproduction.
Contents
Etiology and Incidence
Cryptococcosis is a defining opportunistic infection for AIDS. Other conditions which pose an increased risk include certain lymphomas (e.g. Hodgkin's lymphoma), sarcoidosis, and patients on long-term corticosteroid therapy.
Distribution is worldwide in soil[1]. The prevalence of cryptococcosis has been increasing over the past 20 years for many reasons, including the increase in incidence of AIDS and the expanded use of immunosuppressive drugs.
In humans, C. neoformans causes three types of infections:
- Wound or cutaneous cryptococcosis
- Pulmonary cryptococcosis, and
- Cryptococcal meningitis.
Cryptococcal meningitis (infection of the meninges, the tissue covering the brain) is believed to result from dissemination of the fungus from either an observed or unappreciated pulmonary infection. Cryptococcus gattii causes infections in immunocompetent people (those having a functioning immune system), but C. neoformans v. grubii, and v. neoformans usually only cause clinically evident infections in persons who have some form of defect in their immune systems (immunocompromised persons). People who have defects in their cell-mediated immunity, for example, people with AIDS, are especially susceptible to disseminated cryptococcosis. Cryptococcosis is often fatal, especially if untreated.
Although the most common presentation of cryptococcosis is of C. neoformans infection in an immunocompromised person (such as patients with AIDS), the C. gattii is being increasingly recognised as a pathogen in presumptively immunocompetent hosts, especially in Canada and Australia. This may be due to rare exposure and high pathogenicity, or to unrecognised isolated defects in immunity specific to this organism.
Diagnosis
Symptoms include fever, fatigue, chest pain, dry cough, swelling of abdomen, headache, blurred vision and confusion.[2]
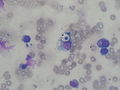
Detection of cryptococcal antigen (capsular material) by culture of CSF, sputum and urine provides definitive diagnosis. Blood cultures may be positive in heavy infections.
Cryptococcosis can rarely occur in the immunocompetent person without HIV, when it usually goes undiagnosed. Less than 250 cases in all are reported in the medical literature, the majority diagnosed postmortem.[3]
Treatment
Treatment options in non-AIDS patients who have reduced immune-system function is not well studied. Intravenous Amphotericin B combined with oral flucytosine may be effective. Every attempt should be made to reduce the amount of immunosuppressive medication until the infection is resolved.
AIDS patients often have a reduced response to Amphotericin B and flucytosine, therefore after initial treatment as above, oral fluconazole can be used.[2] The decision on when to start treatment for HIV is not yet settled, although one small, under-powered trial suggested that delaying the start of treatment for 10 weeks may be beneficial in avoiding deaths from Immune reconstitution inflammatory syndrome (IRIS).[4]
IRIS in immunocompetent hosts
The immune reconstitution inflammatory syndrome (IRIS) has been described in immunocompetent hosts who have meningitis caused by C. gattii and C. grubii. Several weeks or even months into appropriate treatment, there is a sudden onset deterioration with worsening meningitis symptoms and progression or development of new neurological symptoms.
Magnetic resonance imaging shows increase in the size of brain lesions, and CSF abnormalities (white cell count, protein, glucose) increase. CSF culture is sterile, and there is no increase in CSF cryptococcal antigen titre.
The increasing inflammation can cause brain injury or be fatal.[5] [6] [7]
The mechanism behind IRIS in cryptococcal meningitis may be local or systemic immunosuppression induced by the cryptococcal infection which resolves as the organism is killed by antifungal treatment. This is associated with increased inflammation as the recovering immune system recognises the fungus. Treatment with systemic corticosteroids during IRIS may be beneficial in preventing death or progressive neurological deterioration.
IRIS may be the cause of paradoxically worse outcomes for cryptococcal meningitis in immunocompetent compared with immunocompromised hosts, in whom Cryptococcus neoformans is the usual pathogen.
Veterinary cases
Cryptococcosis is also seen in cats and occasionally dogs. It is the most common deep fungal disease in cats, usually leading to chronic infection of the nose and sinuses, and skin ulcers. Cats may develop a bump over the bridge of the nose from local tissue inflammation. It can be associated with FeLV infection in cats.Cryptococcis is most common in dogs and cats but cattle,sheep,goat,horse,wild animals and birds can also be infected.Soil,fowl manure and pigeon droppings are among the sources of infection. [8][9]
Additional images
References
- ^ http://www.umm.edu/ency/article/000642.htm
- ^ a b Barron MA and Madinger NE (November 18, 2008). "Opportunistic Fungal Infections, Part 3: Cryptococcosis, Histoplasmosis, Coccidioidomycosis, and Emerging Mould Infections". Infections in Medicine. http://www.consultantlive.com/infection/article/1145625/1404367?pageNumber=1.
- ^ King JW and Dasgupta A (Jun 15, 2007). "Cryptococcosis". EMedicine. http://emedicine.medscape.com/article/215354-overview.
- ^ Makadzange AT, Ndhlovu CE, Takarinda K, Reid M, Kurangwa M, Gona P, Hakim JG (2010). "Early versus delayed initiation of antiretroviral therapy for concurrent HIV infection and cryptococcal meningitis in sub-saharan Africa". Clin Infect Dis 50 (11): 1532–8. doi:10.1086/652652.|pmid= 20415574}
- ^ Lane M, McBride J and Archer J "Steroid responsive late deterioration in Cryptococcus neoformans variety gattii meningitis", Neurology 2004;63;713-714
- ^ Einsiedel L, Gordon DL, and Dyer JR, "Paradoxical inflammatory reaction during treatment of Cryptococcus neoformans var. gattii meningitis in an HIV-seronegative woman", CID 2004;39:e78–82
- ^ Ecevit IZ, Clancy CJ, Schmalfuss IM, and Nguyen MH, "The poor prognosis of central nervous system cryptococcosis among nonimmunosuppressed atients: A call for better disease recognition and evaluation of adjuncts to antifungal therapy", CID 2006;42:1443–7
- ^ Deep fungal infections
- ^ Malik (2003), "Feline Cryptococcosis"
External links
- The Merck Manual
- Health AtoZ
- synd/1793 at Who Named It?
- See pathology video with commentary of brain tissue infested by cryptoccocus neoformans
Infectious diseases · Mycoses and Mesomycetozoea (B35–B49, 110–118) Superficial and
cutaneous
(dermatomycosis):
Tinea=skin;
Piedra (exothrix/
endothrix)=hairBy locationTinea barbae/Tinea capitis (Kerion) · Tinea corporis (Ringworm, Dermatophytid) · Tinea cruris · Tinea manuum · Tinea pedis (Athlete's foot) · Tinea unguium/Onychomycosis (White superficial onychomycosis · Distal subungual onychomycosis · Proximal subungual onychomycosis)
Tinea corporis gladiatorum · Tinea faciei · Tinea imbricata · Tinea incognito · FavusBy organismEpidermophyton floccosum · Microsporum canis · Microsporum audouinii · Trichophyton interdigitale/mentagrophytes · Trichophyton tonsurans · Trichophyton schoenleini · Trichophyton rubrumOtherSubcutaneous,
systemic,
and opportunisticCoccidioides immitis/Coccidioides posadasii (Coccidioidomycosis, Disseminated coccidioidomycosis, Primary cutaneous coccidioidomycosis. Primary pulmonary coccidioidomycosis) · Histoplasma capsulatum (Histoplasmosis, Primary cutaneous histoplasmosis, Primary pulmonary histoplasmosis, Progressive disseminated histoplasmosis) · Histoplasma duboisii (African histoplasmosis) · Lacazia loboi (Lobomycosis) · Paracoccidioides brasiliensis (Paracoccidioidomycosis)OtherBlastomyces dermatitidis (Blastomycosis, North American blastomycosis, South American blastomycosis) · Sporothrix schenckii (Sporotrichosis) · Penicillium marneffei (Penicilliosis)Yeast-likeCandida albicans (Candidiasis, Oral, Esophageal, Vulvovaginal, Chronic mucocutaneous, Antibiotic candidiasis, Candidal intertrigo, Candidal onychomycosis, Candidal paronychia, Candidid, Diaper candidiasis, Congenital cutaneous candidiasis, Perianal candidiasis, Systemic candidiasis, Erosio interdigitalis blastomycetica) · C. glabrata · C. tropicalis · C. lusitaniae · Pneumocystis jirovecii (Pneumocystosis, Pneumocystis pneumonia)Mold-likeAspergillus (Aspergillosis, Aspergilloma, Allergic bronchopulmonary aspergillosis, Primary cutaneous aspergillosis) · Exophiala jeanselmei (Eumycetoma) · Fonsecaea pedrosoi/Fonsecaea compacta/Phialophora verrucosa (Chromoblastomycosis) · Geotrichum candidum (Geotrichosis) · Pseudallescheria boydii (Allescheriasis)Basidiobolus ranarum (Basidiobolomycosis) · Conidiobolus coronatus/Conidiobolus incongruus (Conidiobolomycosis)Mesomycetozoea Ungrouped Alternariosis · Fungal folliculitis · Fusarium (Fusariosis) · Granuloma gluteale infantum · Hyalohyphomycosis · Otomycosis · PhaeohyphomycosisCategories:- Fungal diseases
- Mycosis-related cutaneous conditions
Wikimedia Foundation. 2010.