- Athlete's foot
-
This article is about a medical condition. For the American retail shoe store, see The Athlete's Foot.
Athlete's Foot Classification and external resources 
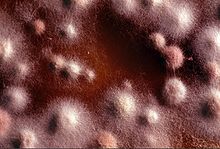
Pale, flaky & split skin of athlete's foot in a toeICD-10 B35.3 ICD-9 110.4 DiseasesDB 13122 MedlinePlus 000875 eMedicine derm/470 MeSH D014008 Athlete's foot (also known as ringworm of the foot[1] and tinea pedis[1]) is a fungal infection of the skin that causes scaling, flaking, and itch of affected areas. It is caused by fungi in the genus Trichophyton and is typically transmitted in moist areas where people walk barefoot, such as showers or bathhouses. Although the condition typically affects the feet, it can spread to other areas of the body, including the groin. Athlete's foot can be treated by a number of pharmaceutical and other treatments.
Contents
Signs and symptoms
Athlete's foot causes scaling, flaking, and itching of the affected skin. Blisters and cracked skin may also occur, leading to exposed raw tissue, pain, swelling, and inflammation. Secondary bacterial infection can accompany the fungal infection, sometimes requiring a course of oral antibiotics.[2][3]
The infection can be spread to other areas of the body, such as the groin, and usually is called by a different name once it spreads, such as tinea corporis on the body or limbs and tinea cruris (jock itch or dhobi itch) for an infection of the groin. Tinea pedis most often manifests between the toes, with the space between the fourth and fifth digits most commonly afflicted.[4][5][6]
Some individuals may experience an allergic response to the fungus called an "id reaction" in which blisters or vesicles can appear in areas such as the hands, chest and arms. Treatment of the fungus usually results in resolution of the id reaction.
Diagnosis
Athlete's foot can usually be diagnosed by visual inspection of the skin, but where the diagnosis is in doubt direct microscopy of a potassium hydroxide preparation (known as a KOH test) may help rule out other possible causes, such as eczema or psoriasis.[7] A KOH preparation is performed on skin scrapings from the affected area. The KOH preparation has an excellent positive predictive value, but occasionally false negative results may be obtained, especially if treatment with an antifungal medication has already begun.[4]
If the above diagnoses are inconclusive or if a treatment regimen has already been started, a biopsy of the affected skin (i.e. a sample of the living skin tissue) can be taken for histological examination.
A Wood's lamp, although useful in diagnosing fungal infections of the scalp (tinea capitis), is not usually helpful in diagnosing tinea pedis, since the common dermatophytes that cause this disease do not fluoresce under ultraviolet light.[4] However, it can be useful for determining if the disease is due to a nonfungal afflictor.[citation needed]
Transmission
- From person to person
Athlete's foot is a communicable disease caused by a parasitic fungus in the genus Trichophyton, either Trichophyton rubrum or Trichophyton mentagrophytes.[8] It is typically transmitted in moist environments where people walk barefoot, such as showers, bath houses, and locker rooms.[8][9][10] It can also be transmitted by sharing footwear with an infected person, or less commonly, by sharing towels with an infected person.
- To other parts of the body
The various parasitic fungi that cause athlete's foot can also cause skin infections on other areas of the body, most often under toenails (onychomycosis) or on the groin (tinea cruris).
Prevention
The fungi that cause athlete's foot can live on shower floors,[11] wet towels, and footwear,[11] and can spread from person to person from shared contact with showers, towels, etc.[12]
Hygiene, therefore, plays an important role in managing an athlete's foot infection. Since fungi thrive in moist environments, keeping feet and footwear as dry as possible, and avoiding sharing towels, etc., aids prevention of primary infection.
Treatments
Without medication athlete's foot resolves in 30–40% of cases[13] and topical antifungal medication consistently produce much higher percentages of cure.[14]
Medication
Conventional treatment typically involves daily or twice daily application of a topical medication in conjunction with hygiene measures outlined in the above section on prevention. Keeping feet dry and practicing good hygiene is crucial to preventing reinfection. Severe or prolonged fungal skin infections may require treatment with oral antifungal medication. Zinc oxide-based diaper rash ointment may be used; talcum powder can be used to absorb moisture to kill off the infection.
Topical
The fungal infection may be treated with topical antifungal agents, which can take the form of a spray, powder, cream, or gel. There exists a large number of antifungal drugs including: miconazole nitrate, clotrimazole, and nystatin.
A solution of 1% potassium permanganate dissolved in hot water may be found to be an excellent alternative to antifungal drugs.[15]
The time-line for cure may be long, often 45 days or longer. The recommended course of treatment is to "continue to use the topical treatment for four weeks after the symptoms have subsided" to ensure the fungus has been completely eliminated. However, because the itching associated with the infection subsides quickly, patients may not complete the courses of therapy prescribed.
Anti-itch creams are not recommended, as they will alleviate the symptoms, but will exacerbate the fungus; this is because anti-itch creams typically enhance the moisture content of the skin and encourage fungal growth.
If the fungal invader is not a dermatophyte, but a yeast, other medications such as fluconazole may be used. Typically, fluconazole is used for candidal vaginal infections (moniliasis), but has been shown to be of benefit for those with cutaneous yeast infections, as well. The most common of these infections occur in the web (intertriginous) spaces of the toes and at the base of the fingernail or toenail. The hallmark of these infections is a cherry red color surrounding the lesion and a yellow thick pus.
Oral
For severe cases, the current preferred oral agent in the UK[16] is the more effective terbinafine.[17] Other prescription oral antifungals include itraconazole and fluconazole.[2]
Alternative treatments
Tea tree oil may improve the symptoms but does not cure the underlying fungal infection.[18][19][20] Ajoene, a compound found in garlic, is sometimes used to treat athlete's foot.[21] Urinating on the feet during a shower may also help with the treatment of athlete's foot.[citation needed]
References
- ^ a b Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. pp. 1135. ISBN 1-4160-2999-0.
- ^ a b Gupta AK, Skinner AR, Cooper EA (2003). "Interdigital tinea pedis (dermatophytosis simplex and complex) and treatment with ciclopirox 0.77% gel". Int. J. Dermatol. 42 (Suppl 1): 23–7. doi:10.1046/j.1365-4362.42.s1.1.x. PMID 12895184.
- ^ Guttman, C; Skinner, Alayne R.; Cooper, Elizabeth A. (2003). "Secondary bacterial infection always accompanies interdigital tinea pedis". Dermatol Times 4: 23–7. doi:10.1046/j.1365-4362.42.s1.1.x. PMID 12895184.
- ^ a b c Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clinical and Molecular Allergy 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029. http://www.clinicalmolecularallergy.com/content/2/1/5.
- ^ Hainer BL (2003). "Dermatophyte infections". American Family Physician 67 (1): 101–8. PMID 12537173.
- ^ Hirschmann JV, Raugi GJ (2000). "Pustular tinea pedis". J. Am. Acad. Dermatol. 42 (1 Pt 1): 132–3. doi:10.1016/S0190-9622(00)90022-7. PMID 10607333.
- ^ del Palacio, Amalia; Margarita Garau, Alba Gonzalez-Escalada and Mª Teresa Calvo. "Trends in the treatment of dermatophytosis" (PDF). Biology of Dermatophytes and other Keratinophilic Fungi: 148–158. http://www.dermatophytes.reviberoammicol.com/p148158.pdf. Retrieved 10 October 2007.
- ^ a b "Athlete's Foot – Cause". WebMD. 2 July 2008. http://www.webmd.com/skin-problems-and-treatments/tc/athletes-foot-cause. Retrieved 13 March 2010.
- ^ "Athlete's foot". Mayo Clinic Health Center. http://www.mayoclinic.com/health/athletes-foot/DS00317.
- ^ [1] Risk factors for athlete's foot, at WebMD
- ^ a b Ajello L, Getz M E (1954). "Recovery of dermatophytes from shoes and a shower stall". J. Invest. Dermat. 22 (4): 17–22. doi:10.1038/jid.1954.5. PMID 11237081.
- ^ Robert Preidt (29 September 2006). "Athlete's Foot, Toe Fungus a Family Affair" (Reprint at USA Today). HealthDay News. http://www.healthscout.com/news/68/535172/main.html. Retrieved 10 October 2007. ""Researchers used advanced molecular biology techniques to test the members of 57 families and concluded that toenail fungus and athlete's foot can infect people living in the same household.""
- ^ Over-the-Counter Foot Remedies (American Family Physician)
- ^ Crawford F, Hollis S (18 July 2007). Crawford, Fay. ed. "Topical treatments for fungal infections of the skin and nails of the foot" (Review). Cochrane Database of Systematic Reviews (3): CD001434. doi:10.1002/14651858.CD001434.pub2. PMID 17636672. http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001434/frame.html.
- ^ "Potassium Permanganate". http://www.dermnetnz.org/treatments/permanganate.html. Retrieved 31 March 2011.
- ^ National Library for Health (6 September 2007). "What is the best treatment for tinea pedis?". UK National Health Service. http://www.clinicalanswers.nhs.uk/index.cfm?question=6098. Retrieved 29 September 2007.
- ^ Bell-Syer SEM, Hart R, Crawford F, Torgerson DJ, Tyrrell W, Russell (22 April 2002). Bell-Syer, Sally EM. ed. "Oral treatments for fungal infections of the skin of the foot". Cochrane Database Syst Rev 2 (2): CD003584. doi:10.1002/14651858.CD003584. PMID 12076488.
- ^ Bedinghaus JM, Niedfeldt MW (2001). "Over-the-counter foot remedies". American Family Physician 64 (5): 791–6. PMID 11563570. http://www.aafp.org/afp/20010901/791.html.
- ^ Tong MM, Altman PM, Barnetson RS (1992). "Tea tree oil in the treatment of tinea pedis". Australasian J. Dermatology 33 (3): 145–9. doi:10.1111/j.1440-0960.1992.tb00103.x. PMID 1303075.
- ^ Satchell AC, Saurajen A, Bell C, Barnetson RS (2002). "Treatment of interdigital tinea pedis with 25% and 50% tea tree oil solution: a randomized, placebo-controlled, blinded study". Australasian J. Dermatology 43 (3): 175–8. doi:10.1046/j.1440-0960.2002.00590.x. PMID 12121393.
- ^ Eliades Ledezma, Katiuska Marcano, Alicia Jorquera, Leonardo De Sousa, Maria Padilla, Mireya Pulgar, Rafael Apitz-Castro (November 2000). "Efficacy of ajoene in the treatment of tinea pedis: A double-blind and comparative study with terbinafine". J Am Acad Dermatol 43 (5 pt 1): 829–832. doi:10.1067/mjd.2000.107243. PMID 11050588.
External links
Infectious diseases · Mycoses and Mesomycetozoea (B35–B49, 110–118) Superficial and
cutaneous
(dermatomycosis):
Tinea=skin;
Piedra (exothrix/
endothrix)=hairBy locationTinea barbae/Tinea capitis (Kerion) · Tinea corporis (Ringworm, Dermatophytid) · Tinea cruris · Tinea manuum · Tinea pedis (Athlete's foot) · Tinea unguium/Onychomycosis (White superficial onychomycosis · Distal subungual onychomycosis · Proximal subungual onychomycosis)
Tinea corporis gladiatorum · Tinea faciei · Tinea imbricata · Tinea incognito · FavusBy organismEpidermophyton floccosum · Microsporum canis · Microsporum audouinii · Trichophyton interdigitale/mentagrophytes · Trichophyton tonsurans · Trichophyton schoenleini · Trichophyton rubrumOtherSubcutaneous,
systemic,
and opportunisticCoccidioides immitis/Coccidioides posadasii (Coccidioidomycosis, Disseminated coccidioidomycosis, Primary cutaneous coccidioidomycosis. Primary pulmonary coccidioidomycosis) · Histoplasma capsulatum (Histoplasmosis, Primary cutaneous histoplasmosis, Primary pulmonary histoplasmosis, Progressive disseminated histoplasmosis) · Histoplasma duboisii (African histoplasmosis) · Lacazia loboi (Lobomycosis) · Paracoccidioides brasiliensis (Paracoccidioidomycosis)OtherBlastomyces dermatitidis (Blastomycosis, North American blastomycosis, South American blastomycosis) · Sporothrix schenckii (Sporotrichosis) · Penicillium marneffei (Penicilliosis)Yeast-likeCandida albicans (Candidiasis, Oral, Esophageal, Vulvovaginal, Chronic mucocutaneous, Antibiotic candidiasis, Candidal intertrigo, Candidal onychomycosis, Candidal paronychia, Candidid, Diaper candidiasis, Congenital cutaneous candidiasis, Perianal candidiasis, Systemic candidiasis, Erosio interdigitalis blastomycetica) · C. glabrata · C. tropicalis · C. lusitaniae · Pneumocystis jirovecii (Pneumocystosis, Pneumocystis pneumonia)Mold-likeAspergillus (Aspergillosis, Aspergilloma, Allergic bronchopulmonary aspergillosis, Primary cutaneous aspergillosis) · Exophiala jeanselmei (Eumycetoma) · Fonsecaea pedrosoi/Fonsecaea compacta/Phialophora verrucosa (Chromoblastomycosis) · Geotrichum candidum (Geotrichosis) · Pseudallescheria boydii (Allescheriasis)Basidiobolus ranarum (Basidiobolomycosis) · Conidiobolus coronatus/Conidiobolus incongruus (Conidiobolomycosis)Mesomycetozoea Ungrouped Alternariosis · Fungal folliculitis · Fusarium (Fusariosis) · Granuloma gluteale infantum · Hyalohyphomycosis · Otomycosis · PhaeohyphomycosisCategories:- Fungal diseases
- Foot diseases
- Mycosis-related cutaneous conditions
Wikimedia Foundation. 2010.