- Wart
-
Warts Classification and external resources 
Warts on the big toeICD-10 B07 ICD-9 078.1 DiseasesDB 28410 MedlinePlus 000885 eMedicine emerg/641 MeSH D014860 A wart is generally a small, rough growth, typically on a human’s hands or feet but often other locations, that can resemble a cauliflower or a solid blister. They are caused by a viral infection, specifically by human papillomavirus 2 and 7. There are as many as 10 varieties of warts, the most common considered to be mostly harmless. It is possible to get warts from others; they are contagious and usually enter the body in an area of broken skin.[1] They typically disappear after a few months but can last for years and can recur.[2]
Contents
Types
A range of types of wart have been identified, varying in shape and site affected, as well as the type of human papillomavirus involved.[3][4] These include:
- Common wart (Verruca vulgaris), a raised wart with roughened surface, most common on hands, but can grow anywhere on the body;
- Flat wart (Verruca plana), a small, smooth flattened wart, flesh-coloured, which can occur in large numbers; most common on the face, neck, hands, wrists and knees;
- Filiform or digitate wart, a thread- or finger-like wart, most common on the face, especially near the eyelids and lips;
- Genital wart (venereal wart, Condyloma acuminatum, Verruca acuminata), a wart that occurs on the genitalia.
- Mosaic wart, a group of tightly clustered plantar-type warts, commonly on the hands or soles of the feet;
- Periungual wart, a cauliflower-like cluster of warts that occurs around the nails.
- Plantar wart (verruca, Verruca plantaris), a hard sometimes painful lump, often with multiple black specks in the center; usually only found on pressure points on the soles of the feet;
Cause
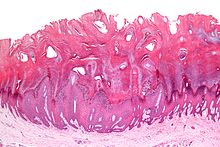 Micrograph of a common wart (verruca vulgaris) showing the characteristic features (hyperkeratosis, acanthosis, hypergranulosis, rete ridge elongation, and large blood vessels at the dermal-epidermal junction. H&E stain.
Micrograph of a common wart (verruca vulgaris) showing the characteristic features (hyperkeratosis, acanthosis, hypergranulosis, rete ridge elongation, and large blood vessels at the dermal-epidermal junction. H&E stain. Main article: Human papilloma virus
Main article: Human papilloma virusWarts are caused by the human papilloma virus (HPV). There are about 130 known types of human papilloma viruses.[5] HPV infects the squamous epithelium, usually of the skin or genitals, but each HPV type is typically only able to infect only a few specific areas on the body. Many HPV types can produce a benign growth, often called a "wart" or "papilloma", in the area they infect. Many of the more common HPV and wart types are as follows:
- Common warts - HPV types 2 and 4 (most common); also types 1, 3, 26, 29, and 57 and others.
- Cancers and Genital dysplasia - "high-risk" HPV types are associated with cancers, (cervical cancer and can also cause some vulvar, vaginal,[6] penile, anal[7] and some oropharyngeal cancers. "low-risk" types are associated with warts or other conditions.[8][9])
-
- High-risk: 16, 18 (cause the most cervical cancer); also 58, 33, 45, 31, 52, 35, 39, 59, and others.
- Plantar warts (myrmecia) - HPV type 1 (most common); also types 2, 3, 4, 27, 28, and 58 and others.
- Anogenital warts (condylomata acuminata or venereal warts) - HPV types 6 and 11 (most common); also types 42, 44 and others.[10]
-
- Low-risk: 6, 11 (most common); also 13, 44, 40, 43, 42, 54, 61, 72, 81, 89, and others.
- Flat warts - HPV types 3, 10, and 28.
- Butcher's warts - HPV type 7.
- Heck's disease (Focal epithelial hyperplasia) - HPV types 13 and 32.
Pathophysiology
Common warts have a characteristic appearance under the microscopic. They have thickening of the stratum corneum (hyperkeratosis), thickening of the stratum spinosum (acanthosis), thickening of the stratum granulosum, rete ridge elongation, and large blood vessels at the dermal-epidermal junction.
Prevention
Gardasil is a HPV vaccine aimed at preventing cervical cancers and genital warts. Gardasil is designed to prevent infection with HPV types 16, 18, 6, and 11. HPV types 16 and 18 currently cause about 70% of cervical cancer cases,[8][9] and also cause some vulvar, vaginal,[6] penile and anal cancers.[7] HPV types 6 and 11 are responsible for 90% of documented cases of genital warts.[11] Unfortunately the HPV vaccines do not currently prevent the virus strain responsible for verrucas.
Treatment
There are many different treatments and procedures associated with wart removal. One review of 52 clinical trials of various cutaneous wart treatments concluded that topical treatments containing salicylic acid were the best supported, with an average cure rate of 75%, compared with 48% for the placebo in six placebo-controlled trials including a total of 376 participants.It can also be controlled by laser therapy[12] The reviewers also concluded that there was little evidence of a significant benefit of cryotherapy over salicylic acid or duct tape.[12]
One complicating factor in the treatment of warts is that the wart may regrow after it has been removed.
Medication
Treatments that may be prescribed by a medical professional include
- Application of podophyllum resin paint [podophyllum resin I.P.'66 (20% w/v), benzoin I.P. (10% w/v), aloes I.P. (2% w/v), isopropyl alcohol I.P. to make (100% v/v)]
- Imiquimod, a topical cream that helps the body's immune system fight the wart virus by encouraging interferon production. Approved by the U.S. Food and Drug Administration (FDA) for genital warts.[13] The drug is very expensive.
- Cantharidin, a chemical found naturally in many members of the beetle family Meloidae which causes dermal blistering. Either used by itself or compounded with podophyllin. Not FDA approved, but available through Canada or select US compounding pharmacies.
- Bleomycin, not US FDA approved. One or two injections used. It can cause necrosis of digits and Raynaud syndrome.[14][15]
- Dinitrochlorobenzene (DNCB), like salicylic acid, this is applied directly to the wart. Studies showed this method was effective with a cure rate of 80%. But DNCB must be used much more cautiously than salicylic acid; the chemical is a known mutagen, able to cause genetic mutations. So a physician must administer DNCB. This drug induces an allergic immune response resulting in inflammation that wards off the wart-causing virus.[16]
- Fluorouracil, which inhibits DNA synthesis, is being used as an experimental treatment. It is applied directly to the wart (especially plantar warts) and covered (for example: with tape). This treatment is combined with the use of a pumice stone, but tends to work very slowly.[17]
- Salicylic acid can be prescribed by a dermatologist in a higher concentration than that found in over-the-counter products. Examples include a topical solution marketed by Elorac, Inc. under the trade name Durasal.
There are several over-the-counter options. The most common ones involve salicylic acid. These products are readily available at drugstores and supermarkets. There are typically two types of products: adhesive pads treated with salicylic acid or a bottle of concentrated salicylic acid solution. Removing a wart with salicylic acid can be done by cleaning the area, applying the acid, and removing the dead skin with a pumice stone or emery board. It may take up to a year to remove a wart[citation needed].
Another product available over-the-counter that can aid in wart removal is silver nitrate in the form of a caustic pencil, which is also available at drug stores. In a placebo-controlled study of 70 patients, silver nitrate given over nine days resulted in clearance of all warts in 43% and improvement in warts in 26% one month after treatment compared to 11% and 14%, respectively, in the placebo group.[18] The instructions must be followed to minimize staining of skin and clothing. Occasionally pigmented scars may develop.
Cryosurgery or cryotherapy devices using a dimethyl ether - propane mixture are inexpensive. A disadvantage is that the sponge applicator is too large for small warts, and the temperature achieved is not nearly as low as with liquid nitrogen. Complications include blistering of normal skin if excess freezing is not controlled.
Several randomized controlled trials have found that zinc sulfate, consumed orally, can bring to the disappearance of warts,[19][20][21] using typically about 2.5 mg/kg/day elemental zinc (large amounts of zinc may cause a copper deficiency[19]). Other trials have found that topical zinc sulfate solution[22] or zinc oxide[23] are also effective.
Procedures
- Keratolysis, of dead surface skin cells usually using salicylic acid, blistering agents, immune system modifiers ("immunomodulators"), or formaldehyde, often with mechanical paring of the wart with a pumice stone, blade etc.[24]
- Electrodesiccation[25]
- Cryosurgery, which involves freezing the wart (generally with liquid nitrogen), creating a blister between the wart and epidermal layer, after which the wart and surrounding dead skin falls off by itself. An average of 3 to 4 treatments are required for warts of thin skin. Warts on calloused skin like plantar warts might take dozens or more treatments.[14]
- Surgical curettage of the wart;
- Laser treatment - often with a pulse dye laser or carbon dioxide (CO2) laser. Pulse dye lasers (wavelength 582 nm) work by selective absorption by blood cells (specifically haemoglobin). CO2 lasers work by selective absorption by water molecules. Pulse dye lasers are less destructive and more likely to heal without scarring. CO2 laser works by vaporizing and destroying tissue and skin. Laser treatments can be painful, expensive (though covered by many insurances), and can cause little scarring when used appropriately. CO2 lasers will require local anaesthetic. Pulse dye laser treatment does not need conscious sedation nor local anesthetic. It takes 2 to 4 treatments but can be many more for extreme cases. Typically, 10-14 days are required between treatments. Preventative measures are important.[14]
- Infrared coagulator - an intense source of infrared light in a small beam like a laser. This works essentially on the same principle as laser treatment. It is less expensive. Like the laser, it can cause blistering pain and scarring.[26]
- Duct tape occlusion therapy (DTOT) involves placing a piece of duct tape over the wart. The evidence as to whether or not it is effective is poor.[27][28]
In other animals
References
- ^ http://www.webmd.com/skin-problems-and-treatments/tc/warts-and-plantar-warts-topic-overview
- ^ medline plus warts National institutes of Health.
- ^ Mosby's Medical, Nursing, & Allied Health Dictionary (5th edn), Anderson KN, Anderson LE, Glanze WD, eds, Mosby
- ^ "MedlinePlus: Warts". 2010. http://www.webmd.com/skin-problems-and-treatments/tc/warts-and-plantar-warts-topic-overview.
- ^ de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H (Jun 2004). "Classification of papillomaviruses". Virology 324 (1): 17–27. doi:10.1016/j.virol.2004.03.033. PMID 15183049.
- ^ a b "FDA Approves Expanded Uses for Gardasil to Include Preventing Certain Vulvar and Vaginal Cancers". 2008-09-12. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116945.htm. Retrieved 2009-08-04.
- ^ a b Cortez, Michelle Fay and Pettypiece, Shannon. "Merck Cancer Shot Cuts Genital Warts, Lesions in Men". Bloomberg News. (Bloomberg.com) 13 Nov 2008.
- ^ a b Lowy DR, Schiller JT (2006). "Prophylactic human papillomavirus vaccines.". J. Clin. Invest. 116 (5): 1167–73. doi:10.1172/JCI28607. PMC 1451224. PMID 16670757. http://www.jci.org/articles/view/JCI28607. Retrieved 2007-12-01.
- ^ a b Muñoz N, Bosch FX, Castellsagué X, Díaz M, de Sanjose S, Hammouda D, Shah KV, Meijer CJ (2004-08-20). "Against which human papillomavirus types shall we vaccinate and screen? The international perspective.". Int J Cancer 111 (2): 278–85. doi:10.1002/ijc.20244. PMID 15197783.
- ^ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Mitchell, Richard (2007). "Chapter 19 The Female Genital System and Breast". Robbins Basic Pathology (8 ed.). Philadelphia: Saunders. ISBN 1-4160-2973-7.
- ^ Steinbrook, Robert (March 16, 2006). "Perspective - The Potential of Human Papillomavirus Vaccines". http://content.nejm.org/cgi/content/full/354/11/1109.
- ^ a b Gibbs S, Harvey I, Sterling JC, Stark R (2003). "Local treatments for cutaneous warts". Cochrane Database Syst Rev (3): CD001781. doi:10.1002/14651858.CD001781. PMID 12917913.
- ^ "Medscape Imiquimod article". http://www.medscape.org/viewarticle/740315. Retrieved 10 August 2011.
- ^ a b c Aafp.org
- ^ Champion, R.H., et al. Rook's Textbook of Dermatology. Blackwell Science. 1998. p. 1044
- ^ Health.harvard.edu
- ^ Podiatrytoday.com
- ^ [1] Sterling, J. C.; Handfield-Jones, S.; Hudson, P. M.; British Association of Dermatologists (2001). "Guidelines for the management of cutaneous warts". British Journal of Dermatology 144 (1): 4–11. doi:10.1046/j.1365-2133.2001.04066.x. PMID 11167676.
- ^ a b Stefani M, Bottino G, Fontenelle E, Azulay DR (2009). "Efficacy comparison between cimetidine and zinc sulphate in the treatment of multiple and recalcitrant warts". An Bras Dermatol 84 (1): 23–9. PMID 19377755. http://www.scielo.br/scielo.php?pid=S0365-05962009000100003&script=sci_arttext&tlng=en.
- ^ Yaghoobi R, Sadighha A, Baktash D (April 2009). "Evaluation of oral zinc sulfate effect on recalcitrant multiple viral warts: a randomized placebo-controlled clinical trial". J. Am. Acad. Dermatol. 60 (4): 706–8. doi:10.1016/j.jaad.2008.09.010. PMID 19293025. http://www.eblue.org/article/S0190-9622%2808%2901148-1/fulltext.
- ^ Al-Gurairi FT, Al-Waiz M, Sharquie KE (March 2002). "Oral zinc sulphate in the treatment of recalcitrant viral warts: randomized placebo-controlled clinical trial". Br. J. Dermatol. 146 (3): 423–31. doi:10.1046/j.1365-2133.2002.04617.x. PMID 11952542.
- ^ Sharquie KE, Khorsheed AA, Al-Nuaimy AA (September 2007). "Topical zinc sulphate solution for treatment of viral warts". Saudi Med J 28 (9): 1418–21. PMID 17768472.
- ^ Khattar JA, Musharrafieh UM, Tamim H, Hamadeh GN (April 2007). "Topical zinc oxide vs. salicylic acid-lactic acid combination in the treatment of warts". Int. J. Dermatol. 46 (4): 427–30. doi:10.1111/j.1365-4632.2006.03138.x. PMID 17442091.
- ^ Warts at About.com
- ^ Pubmedcentral.nih.gov
- ^ Halazs C. L. G., Treatment of common warts using the infrared coagulator. The Journal of dermatologic surgery and oncology ISSN 0148-0812. 1994, vol. 20, no4, pp. 252-256 (21 ref.)
- ^ Wenner, R; Askari, SK, Cham, PM, Kedrowski, DA, Liu, A, Warshaw, EM (2007 Mar). "Duct tape for the treatment of common warts in adults: a double-blind randomized controlled trial.". Archives of dermatology 143 (3): 309-13. PMID 17372095.
- ^ Ringold, S; Mendoza, JA, Tarini, BA, Sox, C (2002 Oct). "Is duct tape occlusion therapy as effective as cryotherapy for the treatment of the common wart?". Archives of pediatrics & adolescent medicine 156 (10): 975-7. PMID 12361441.
External links
- Wart photo library, Dermnet
Infectious skin disease: Viral cutaneous conditions, including viral exanthema (B00–B09, 050–059) HSV (Herpes simplex, Herpetic whitlow, Herpes gladiatorum, Herpetic keratoconjunctivitis, Herpetic sycosis, Neonatal herpes simplex, Herpes genitalis, Herpes labialis, Eczema herpeticum, Herpetiform esophagitis) · Herpes B virus (B virus infection)VZV (Chickenpox, Herpes zoster, Herpes zoster oticus, Ophthalmic zoster, Disseminated herpes zoster, Zoster-associated pain, Inflammatory skin lesions following zoster infection, Modified varicella-like syndrome)SealpoxOtherPapillomaviridaeHPV (Wart/Plantar wart, Heck's disease, Genital wart (giant), Laryngeal papillomatosis, Butcher's wart, Bowenoid papulosis, Epidermodysplasia verruciformis, Verruca plana, Pigmented wart, Verrucae palmares et plantares )
BPV (Equine sarcoid)Parvovirus B19 (Erythema infectiosum, Reticulocytopenia, Papular purpuric gloves and socks syndrome)CAV (Hand, foot and mouth disease, Herpangina) · FMDV (Foot-and-mouth disease) · Boston exanthem diseaseUngrouped unknown/multiple: Asymmetric periflexural exanthem of childhood · Post-vaccination follicular eruption · Lipschütz ulcer · Eruptive pseudoangiomatosis · Viral-associated trichodysplasia · Gianotti–Crosti syndromePapillomavirus – Human papillomavirus Related
diseasesCervical cancer ·
Warts (genital, plantar, flat, Laryngeal papillomatosis), Epidermodysplasia verruciformis, Focal epithelial hyperplasia, Papilloma
Factor in other cancers (Anal, Vaginal, Vulvar, Penile, Head and neck cancer (HPV-positive oropharyngeal cancer)) ·Vaccine Screening Pap test (stain) - Cytopathology/Cytotechnology results Bethesda System
Experimental techniques (Speculoscopy, Cervicography)Colposcopy Biopsy histology Treatment History Categories:- Papillomavirus
- Virus-related cutaneous conditions
Wikimedia Foundation. 2010.



