- Darier's disease
-
Darier's disease Classification and external resources 
Linear Darier's diseaseICD-10 Q82.8 (ILDS Q82.868) ICD-9 757.39 OMIM 124200 DiseasesDB 3467 eMedicine derm/209 MeSH D007644 Darier's disease (DAR), also known as Darier disease, Darier–White disease,[1] Dyskeratosis follicularis[1] and Keratosis follicularis,[2]:523[3]:567 is an autosomal dominant disorder discovered by French dermatologist Ferdinand-Jean Darier. Darier's is characterized by dark crusty patches on the skin, sometimes containing pus. The crusty patches are also known as keratotic papules, keratosis follicularis or dyskeratosis follicularis.[4][5]
Contents
Characteristics
DAR affects both men and women and is not contagious. The disease often starts during or later than the teenage years, typically by the third decade. Short stature is common. The prevalence is estimated as between 1: 30,000 and 1: 100,000. The symptoms of the disease are thought to be caused by an abnormality in the desmosome-keratin filament complex leading to a breakdown in cell adhesion.
It most commonly affects the chest, neck, back, ears, forehead, and groin, but may involve other body areas. The rash associated with Darier's disease often has a distinct odor. Palms & soles may become thickened, intra oral papules can be found. Finger nails become fragile and this helps in diagnosis of the disease. The rash can be aggravated by heat, humidity, and exposure to sunlight. In some cases, sunlight makes it better, especially in the forehead.
Minor forms of the disease are the most common, and may remain undiagnosed throughout life. These consist mainly of minor rashes without odor that are aggravated by heat, humidity, stress and sunlight. Poorly formed fingernails containing vertical striations are diagnostic.
A recent study examined neuropsychiatric conditions in a non-random sample of 100 British individuals assessed as having DAR. There were high lifetime rates for mood disorders (50%), including depression (30%), bipolar disorder (4%), suicidal thoughts (31%) and suicide attempts (13%), suggesting a possible common genetic link.[6] Scattered case studies also suggest a possible link to learning disorders (not yet confirmed).
Genetics
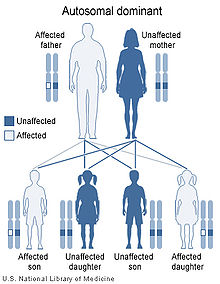
DAR is inherited in an autosomal dominant manner,[7] which indicates that the defective gene responsible for a disorder is located on an autosome, and only one copy of the gene is sufficient to cause the disorder, when inherited from a parent who has the disorder.
The disorder is caused by a mutation in the gene ATP2A2.[7] Family members with confirmed identical ATP2A2 mutations can exhibit differences in the clinical severity of disease, suggesting that other genes or environmental factors affect the expression of Darier's disease. With the discovery of the ATP2A2 gene, performing genetic tests to confirm the diagnosis of Darier's disease is now possible.
Treatment
Treatment of choice for severe cases is oral retinoids. During flares, topical or oral antibiotics may be administered. Ciclosporin and prescription-only topical corticosteroids, eg, betamethasone, have been used during acute flares. Some patients are able to prevent flares with use of topical sunscreens and oral vitamin C.[8]
For minor forms, no specific treatment is required, but avoidance of excessive heat, humidity, stress and tight-fitting clothes (and general cleanliness) is advised. Topical creams (as above) are occasionally required to deal with flare-ups.
See also
- Linear Darier disease
- List of cutaneous conditions
References
- ^ a b Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ^ Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0071380760.
- ^ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0721629210.
- ^ National Organization for Rare Disorders (2002). NORD Guide to Rare Disorders. Lippincott Williams & Wilkins. ISBN 0781730635.
- ^ Sehgal, V. N.; Srivastava, G. (2005). "Darier's (Darier-White) disease / keratosis follicularis". International Journal of Dermatology 44 (3): 184–192. doi:10.1111/j.1365-4632.2004.02408.x. PMID 15807723.
- ^ Gordon-Smith, K. et al. (2010). "The neuropsychiatric phenotype in Darier disease". British Journal of Dermatology 163 (3): 515–522. doi:10.1111/j.1365-2133.2010.09834.x. PMID 20456342.
- ^ a b Sakuntabhai A, Burge S, Monk S, Hovnanian A (September 1999). "Spectrum of novel ATP2A2 mutations in patients with Darier's disease". Hum. Mol. Genet. 8 (9): 1611–9. doi:10.1093/hmg/8.9.1611. PMID 10441323. http://hmg.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=10441323.
- ^ Andrew's Diseases of the Skin (James, Berger, Elston, 10th ed., Saunders Elsevier, 2006)
- ^ Lippincott's Illustrated Reviews: Biochemistry (Champe, Harvey & Ferrier, ISBN 0781722659, 3rd ed., Lippincott Williams & Wilkins 2005)
External links
- DermNet scaly/darier
- Photos at skinsite.com
Congenital malformations and deformations of integument / skin disease (Q80–Q82, 757.0–757.3) Genodermatosis Congenital ichthyosis/
erythrokeratodermiaADARUngroupedIchthyosis bullosa of Siemens · Ichthyosis follicularis · Ichthyosis prematurity syndrome · Ichthyosis–sclerosing cholangitis syndrome · Nonbullous congenital ichthyosiform erythroderma · Ichthyosis linearis circumflexa · Ichthyosis hystrixrelated: Costello syndrome · Kindler syndrome · Laryngoonychocutaneous syndrome · Skin fragility syndrome ·Naegeli syndrome/Dermatopathia pigmentosa reticularis · Hay–Wells syndrome · Hypohidrotic ectodermal dysplasia · Focal dermal hypoplasia · Ellis–van Creveld syndrome · Rapp–Hodgkin syndrome/Hay–Wells syndromeEhlers–Danlos syndrome · Cutis laxa (Gerodermia osteodysplastica) · Popliteal pterygium syndrome · Pseudoxanthoma elasticum · Van Der Woude syndromediffuse: Diffuse epidermolytic palmoplantar keratoderma • Diffuse nonepidermolytic palmoplantar keratoderma • Palmoplantar keratoderma of Sybert • Mal de Meleda •syndromic (connexin (Bart–Pumphrey syndrome • Clouston's hidrotic ectodermal dysplasia • Vohwinkel syndrome) • Corneodermatoosseous syndrome • plakoglobin (Naxos syndrome) • Scleroatrophic syndrome of Huriez • Olmsted syndrome • Cathepsin C (Papillon–Lefèvre syndrome • Haim–Munk syndrome) • Camisa diseasefocal: Focal palmoplantar keratoderma with oral mucosal hyperkeratosis • Focal palmoplantar and gingival keratosis • Howel–Evans syndrome • Pachyonychia congenita (Pachyonychia congenita type I • Pachyonychia congenita type II) • Striate palmoplantar keratoderma • Tyrosinemia type II)punctate: Acrokeratoelastoidosis of Costa • Focal acral hyperkeratosis • Keratosis punctata palmaris et plantaris • Keratosis punctata of the palmar creases • Schöpf–Schulz–Passarge syndrome • Porokeratosis plantaris discreta • Spiny keratodermaungrouped: Palmoplantar keratoderma and spastic paraplegia • desmoplakin (Carvajal syndrome) • connexin (Erythrokeratodermia variabilis • HID/KID)OtherMeleda disease · Keratosis pilaris · ATP2A2 (Darier's disease) · Dyskeratosis congenita · Lelis syndromeDyskeratosis congenita · Keratolytic winter erythema · Keratosis follicularis spinulosa decalvans · Keratosis linearis with ichthyosis congenital and sclerosing keratoderma syndrome · Keratosis pilaris atrophicans faciei · Keratosis pilarisOthercadherin (EEM syndrome) · immune system (Hereditary lymphedema, Mastocytosis/Urticaria pigmentosa) · Hailey–Hailey
see also Template:Congenital malformations and deformations of skin appendages, Template:Phakomatoses, Template:Pigmentation disorders, Template:DNA replication and repair-deficiency disorderDevelopmental
anomaliesMidlineOther/ungroupedAplasia cutis congenita · Amniotic band syndrome · Branchial cyst · Cavernous venous malformation
Accessory nail of the fifth toe · Bronchogenic cyst · Congenital cartilaginous rest of the neck · Congenital hypertrophy of the lateral fold of the hallux · Congenital lip pit · Congenital malformations of the dermatoglyphs · Congenital preauricular fistula · Congenital smooth muscle hamartoma · Cystic lymphatic malformation · Median raphe cyst · Melanotic neuroectodermal tumor of infancy · Mongolian spot · Nasolacrimal duct cyst · Omphalomesenteric duct cyst · Poland anomaly · Rapidly involuting congenital hemangioma · Rosenthal–Kloepfer syndrome · Skin dimple · Superficial lymphatic malformation · Thyroglossal duct cyst · Verrucous vascular malformation · BirthmarkGenetic disorder, membrane: ATPase disorders ATP1 ATP2 ATP7 ATP13 Other see also ATPase
B structural (perx, skel, cili, mito, nucl, sclr) · DNA/RNA/protein synthesis (drep, trfc, tscr, tltn) · membrane (icha, slcr, atpa, abct, othr) · transduction (iter, csrc, itra), trfkCategories:- Genodermatoses
- Conditions of the skin appendages
- Autosomal dominant disorders
- Papulosquamous hyperkeratotic cutaneous conditions
Wikimedia Foundation. 2010.