- Netherton syndrome
-
Netherton syndrome Classification and external resources ICD-10 Q80.8 (ILDS Q80.870) ICD-9 757.1 OMIM 256500 DiseasesDB 30791 eMedicine derm/431 Netherton syndrome is a severe, autosomal recessive[1] form of ichthyosis associated with mutations in the SPINK5 gene.[2][3] It is named after E.W. Netherton.[4]
Contents
Characteristics
Netherton syndrome is characterised by chronic skin inflammation, universal pruritus (itch), severe dehydration and stunted growth. Patients with this disorder tend to have a hair shaft defect (trichorrhexis invaginata), also known as "bamboo hair". The disrupted skin barrier function in affected individuals also presents a high susceptibility to infection and allergy, leading to the development of scaly, reddish skin similar to atopic dermatitis.[5] In severe cases, these atopic manifestations persist throughout the individual's life, and consequently post-natal mortality rates are high. In less severe cases, this develops into the milder ichthyosis linearis circumflexa.[3]
Allergies to nuts and fish are also common amongst affected people but they are not always present in every case.[citation needed]
Cause and Genetics
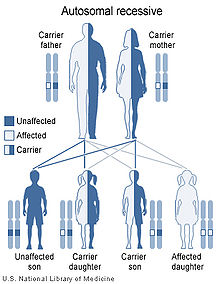 Netherton syndrome has an autosomal recessive pattern of inheritance.
Netherton syndrome has an autosomal recessive pattern of inheritance.
Netherton syndrome is an autosomal recessive disorder associated with mutations in the SPINK5 gene, which encodes the serine protease inhibitor lympho-epithelial Kazal-type-related inhibitor (LEKTI).[2] These mutations result in a dysfunctional protein that has a reduced capacity to inhibit serine proteases expressed in the skin. Potential endogenous targets of LEKTI include KLK5, KLK7 and KLK14.[6] These enzymes are involved in various aspects of epidermal remodelling, including desquamation, PAR-2 activation and degradation of lipid hydrolases, suggesting a potential mechanism for the development of atopic manifestations characteristic of Netherton syndrome.[7]
Disease severity is determined by the level of LEKTI expression and, consequently, serine protease activity. Complete SPINK5 gene deletions have been linked to severe cases, while mutations which induce alternate splicing or create premature stop codons may lead to varying levels of severity.[7] Furthermore, LEKTI-knockout mice exhibit a phenotype similar to Netherton syndrome in humans.[5]
Treatment
There is no known cure at the moment but there are several things that can be done to relieve the symptoms. moisturising products are very helpful to minimise the scaling/cracking and anti-infective treatments are useful when appropriate because the skin is very susceptible to infection. Extra protein in the diet during childhood is also beneficial to replace that which is lost through the previously mentioned "leaky" skin.
Steroid and retinoid products have been proven ineffective against Netherton syndrome and may in fact make things worse for the affected individual.[citation needed]
See also
References
- ^ Chao SC, Richard G, Lee JY (2005). "Netherton syndrome: report of two Taiwanese siblings with staphylococcal scalded skin syndrome and mutation of SPINK5". Br J Dermatol. 152 (1): 159–165. doi:10.1111/j.1365-2133.2005.06337.x. PMID 15656819.
- ^ a b Chavanas S, Bodemer C, Rochat A, (June 2000). "Mutations in SPINK5, encoding a serine protease inhibitor, cause Netherton syndrome". Nat Genet. 25 (2): 141–142. doi:10.1038/75977. PMID 10835624.
- ^ a b Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0071380760.
- ^ Netherton, E. W. A unique case of trichorrhexis nodosa: 'bamboo hairs.'. Arch. Derm. 78: 483-487, 1958.
- ^ a b Descargues P, Deraison C, Bonnart C, Kreft M, Kishibe M, Ishida-Yamamoto A, Elias P, Barrandon Y, Zambruno G, Sonnenberg A, Hovnanian A. (Jan 2005). "Spink5-deficient mice mimic Netherton syndrome through degradation of desmoglein 1 by epidermal protease hyperactivity.". Nat Genet 37 (1): 56-65. PMC 15619623. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=15619623.
- ^ Ovaere P, Lippens S, Vandenabeele P, Declercq W. (Aug 2009). "The emerging roles of serine protease cascades in the epidermis". Trends Biochem Sci 34 (9): 453–63. doi:10.1016/j.tibs.2009.08.001. PMID 19726197.
- ^ a b Hachem JP, Wagberg F, Schmuth M, Crumrine D, Lissens W, Jayakumar A, Houben E, Mauro TM, Leonardsson G, Brattsand M, Egelrud T, Roseeuw D, Clayman GL, Feingold KR, Williams ML, Elias PM. (April 2006). "Serine protease activity and residual LEKTI expression determine phenotype in Netherton syndrome". J Invest Dermatol. 126 (7): 1609-21. PMID 16601670.
External links
Congenital malformations and deformations of integument / skin disease (Q80–Q82, 757.0–757.3) Genodermatosis Congenital ichthyosis/
erythrokeratodermiaADARUngroupedIchthyosis bullosa of Siemens · Ichthyosis follicularis · Ichthyosis prematurity syndrome · Ichthyosis–sclerosing cholangitis syndrome · Nonbullous congenital ichthyosiform erythroderma · Ichthyosis linearis circumflexa · Ichthyosis hystrixEB
and relatedJEB (JEB-H, Mitis, Generalized atrophic, JEB-PA)related: Costello syndrome · Kindler syndrome · Laryngoonychocutaneous syndrome · Skin fragility syndrome ·Naegeli syndrome/Dermatopathia pigmentosa reticularis · Hay–Wells syndrome · Hypohidrotic ectodermal dysplasia · Focal dermal hypoplasia · Ellis–van Creveld syndrome · Rapp–Hodgkin syndrome/Hay–Wells syndromeEhlers–Danlos syndrome · Cutis laxa (Gerodermia osteodysplastica) · Popliteal pterygium syndrome · Pseudoxanthoma elasticum · Van Der Woude syndromeHyperkeratosis/
keratinopathydiffuse: Diffuse epidermolytic palmoplantar keratoderma • Diffuse nonepidermolytic palmoplantar keratoderma • Palmoplantar keratoderma of Sybert • Mal de Meleda •syndromic (connexin (Bart–Pumphrey syndrome • Clouston's hidrotic ectodermal dysplasia • Vohwinkel syndrome) • Corneodermatoosseous syndrome • plakoglobin (Naxos syndrome) • Scleroatrophic syndrome of Huriez • Olmsted syndrome • Cathepsin C (Papillon–Lefèvre syndrome • Haim–Munk syndrome) • Camisa diseasefocal: Focal palmoplantar keratoderma with oral mucosal hyperkeratosis • Focal palmoplantar and gingival keratosis • Howel–Evans syndrome • Pachyonychia congenita (Pachyonychia congenita type I • Pachyonychia congenita type II) • Striate palmoplantar keratoderma • Tyrosinemia type II)punctate: Acrokeratoelastoidosis of Costa • Focal acral hyperkeratosis • Keratosis punctata palmaris et plantaris • Keratosis punctata of the palmar creases • Schöpf–Schulz–Passarge syndrome • Porokeratosis plantaris discreta • Spiny keratodermaungrouped: Palmoplantar keratoderma and spastic paraplegia • desmoplakin (Carvajal syndrome) • connexin (Erythrokeratodermia variabilis • HID/KID)OtherMeleda disease · Keratosis pilaris · ATP2A2 (Darier's disease) · Dyskeratosis congenita · Lelis syndromeDyskeratosis congenita · Keratolytic winter erythema · Keratosis follicularis spinulosa decalvans · Keratosis linearis with ichthyosis congenital and sclerosing keratoderma syndrome · Keratosis pilaris atrophicans faciei · Keratosis pilarisOthercadherin (EEM syndrome) · immune system (Hereditary lymphedema, Mastocytosis/Urticaria pigmentosa) · Hailey–Hailey
see also Template:Congenital malformations and deformations of skin appendages, Template:Phakomatoses, Template:Pigmentation disorders, Template:DNA replication and repair-deficiency disorderDevelopmental
anomaliesMidlineOther/ungroupedAplasia cutis congenita · Amniotic band syndrome · Branchial cyst · Cavernous venous malformation
Accessory nail of the fifth toe · Bronchogenic cyst · Congenital cartilaginous rest of the neck · Congenital hypertrophy of the lateral fold of the hallux · Congenital lip pit · Congenital malformations of the dermatoglyphs · Congenital preauricular fistula · Congenital smooth muscle hamartoma · Cystic lymphatic malformation · Median raphe cyst · Melanotic neuroectodermal tumor of infancy · Mongolian spot · Nasolacrimal duct cyst · Omphalomesenteric duct cyst · Poland anomaly · Rapidly involuting congenital hemangioma · Rosenthal–Kloepfer syndrome · Skin dimple · Superficial lymphatic malformation · Thyroglossal duct cyst · Verrucous vascular malformation · BirthmarkCategories:- Autosomal recessive disorders
- Genodermatoses
- Rare diseases
- Syndromes
Wikimedia Foundation. 2010.
