- Onchocerciasis
-
"River Blindness" redirects here. For the song by J. Geils Band, see Freeze Frame (J. Geils Band album).
Onchocerciasis Classification and external resources 
Adult black fly (Simulium yahense) with parasite (Onchocerca volvulus) emerging from the insect's antenna, magnified 100xICD-10 B73 ICD-9 125.3 DiseasesDB 9218 eMedicine med/1667 oph/709 MeSH D009855 Onchocerciasis (
 /ˈɒŋkɵsɜrˈsaɪ.əsɨs/ or /ˈɒŋkɵsɜrˈkaɪ.əsɨs/), also known as river blindness and Robles' disease, is a parasitic disease caused by infection by Onchocerca volvulus, a nematode (roundworm).[1] Onchocerciasis is the world's second-leading infectious cause of blindness.[1] It is not the nematode, but its endosymbiont, Wolbachia pipientis, that causes the severe inflammatory response that leaves many blind.[2] The parasite is transmitted to humans through the bite of a black fly of the genus Simulium. The larval nematodes spread throughout the body. When the worms die, their Wolbachia symbionts are released, triggering a host immune system response that can cause severe itching, and can destroy optical tissue in the eye.[3]
/ˈɒŋkɵsɜrˈsaɪ.əsɨs/ or /ˈɒŋkɵsɜrˈkaɪ.əsɨs/), also known as river blindness and Robles' disease, is a parasitic disease caused by infection by Onchocerca volvulus, a nematode (roundworm).[1] Onchocerciasis is the world's second-leading infectious cause of blindness.[1] It is not the nematode, but its endosymbiont, Wolbachia pipientis, that causes the severe inflammatory response that leaves many blind.[2] The parasite is transmitted to humans through the bite of a black fly of the genus Simulium. The larval nematodes spread throughout the body. When the worms die, their Wolbachia symbionts are released, triggering a host immune system response that can cause severe itching, and can destroy optical tissue in the eye.[3]The vast majority of infections occur in sub-Saharan Africa, although cases have also been reported in Yemen and isolated areas of Central and South America.[4] An estimated 18 million people suffer from onchocerciasis, with approximately 270,000 cases of blindness related to the infection.[1]
In 1915, Dr. Rodolfo Robles Valverde's study on patients with river blindness in Guatemala led to the discovery that the disease is caused by filaria of O. volvulus, and sheds light on the life cycle and transmission of the parasite. Using case studies of coffee plantation workers in Guatemala, Robles hypothesized the vector of the disease is a day-biting insect, and more specifically, two anthropophilic species of Simulium flies found in the endemic areas. He published his findings on a “new disease” from Guatemala associated with subcutaneous nodules, anterior ocular (eye) lesions, dermatitis, and microfilariae in 1917.[5]
Treatment may involve the use of the drug ivermectin. For best effect, entire communities are treated at the same time. A single dose may kill first-stage larvae (microfilariae) in infected people, and it prevents transmission for many months in the remaining population.[6] Other drugs are also available, including the tetracycline-class antibiotic doxycycline, which kills the Wolbachia and renders the female nematodes sterile. The removal of the palpable nodules is common in Guatemala, Ecuador, and Mexico.[7]
Contents
Classification
Onchocerciasis may be divided into the following phases or types:[8]:440-441[verification needed]
- Erisipela de la costa
- An acute phase, it is characterized by swelling of the face, with erythema and itching.[8]:440 Onchocerciasis causes different kinds of skin changes and these changes vary in different geographic regions. This skin change, erisípela de la costa', of acute onchocerciasis is most commonly seen among victims in Central and South America.[7]
- Mal morando
- This cutaneous condition is characterized by inflammation accompanied by hyperpigmentation.[8]:440
- Sowda
- A cutaneous condition, it is a localized type of onchocerciasis.[8]:440
Additionally, the various skin changes associated with onchocerciasis may be described as follows:[8]:440
- Leopard skin
- A term referring to the spotted depigmentation of the skin that may occur with onchocerciasis[8]:440
- Elephant skin
- A term used to describe the thickening of human skin that may be associated with onchocerciasis[8]:440
- Lizard skin
- A term used to describe the thickened, wrinkled skin changes that may result with onchocerciasis[8]:441
Life cycle of O. volvulus
The life of the parasite can be traced through the black fly and the human hosts in the following steps:[citation needed]
- A Simulium female black fly takes a blood meal on an infected human host, and ingests microfilaria.
- The microfilaria enter the gut and thoracic flight muscles of the black fly, progressing into the first larval stage (J1.).
- The larvae mature into the second larval stage (J2.), and move to the proboscis and into the saliva in its third larval stage (J3.). Maturation takes about 7 days.
- The black fly takes another blood meal, passing the larvae into the next human host’s blood.
- The larvae migrate to the subcutaneous tissue and undergo two more molts. They form nodules as they mature into adult worms over six to twelve months.
- After maturing, adult male worms mate with female worms in the subcutaneous tissue to produce between 700 and 1,500 microfilaria per day.
- The microfilaria migrate to the skin during the day, and the black flies only feed in the day, so the parasite is in a prime position for the female fly to ingest it. Black flies take blood meals to ingest these microfilaria to restart the cycle.
Signs and symptoms
Adult worms remain in subcutaneous nodules, limiting access to the host's immune system.[citation needed] Microfilariae, in contrast, are able to induce intense inflammatory responses, especially upon their death. Dying microfilariae have been recently discovered to release Wolbachia surface protein that activates TLR2 and TLR4, triggering innate immune responses and producing the inflammation and its associated morbidity.[9] Wolbachia species have been found to be endosymbionts of O. volvulus adults and microfilariae, and are thought to be the driving force behind most of O. volvulus morbidity. The severity of illness is directly proportional to the number of infected microfilariae and the power of the resultant inflammatory response.[citation needed]
Skin involvement typically consists of intense itching, swelling, and inflammation.[10] A grading system has been developed to categorize the degree of skin involvement:[11][12][verification needed]
- Acute papular onchodermatitis - scattered pruritic papules,
- Chronic papular onchodermatitis - larger papules, resulting in hyperpigmentation,
- Lichenified onchodermatitis - hyperpigmented papules and plaques, with edema, Lymphadenopathy, pruritus and common secondary bacterial infections,
- Skin atrophy - loss of elasticity, the skin resembles tissue paper, 'lizard skin' appearance, and
- Depigmentation - 'leopard skin' appearance, usually on anterior lower leg.
Ocular involvement provides the common name associated with onchocerciasis, river blindness, and may involve any part of the eye from conjunctiva and cornea to uvea and posterior segment, including the retina and optic nerve.[10] The microfilariae migrate to the surface of the cornea. Punctate keratitis occurs in the infected area. This clears up as the inflammation subsides. However, if the infection is chronic, sclerosing keratitis can occur, making the affected area become opaque. Over time, the entire cornea may become opaque, thus leading to blindness. Some evidence suggests the effect on the cornea is caused by an immune response to bacteria present in the worms.[citation needed].As the skin is itchy, it can lead to severe rashes and you can permanently kill off patches of skin.
The Mazzotti reaction, first described in 1948, is a symptom complex seen in patients after undergoing treatment of onchocerciasis with the medication diethylcarbamazine (DEC). Mazzotti reactions can be life-threatening, and are characterized by fever, urticaria, swollen and tender lymph nodes, tachycardia, hypotension, arthralgias, oedema, and abdominal pain that occur within seven days of treatment of microfilariasis. The phenomenon is so common when DEC is used for the treatment of onchocerciasis that this drug is the basis of a skin patch test used to confirm that diagnosis. The drug patch is placed on the skin, and if the patient is infected with the microfilaria of O. volvulus, localized pruritus and urticaria are seen at the application site.[13]
Prevention
Various control programs aim to stop onchocerciasis from being a public health problem. The first was the Onchocerciasis Control Programme (OCP), which was launched in 1974, and at its peak, it covered 30 million people in eleven countries. Through the use of larvicide spraying of fast-flowing rivers to control black fly populations, and from 1988 onwards, the use of ivermectin to treat infected people, the OCP eliminated onchocerciasis as a public health problem. The OCP, a joint effort of the World Health Organisation, the World Bank, the United Nations Development Programme and the UN Food and Agriculture Organization, was considered to be a success, and came to an end in 2002. Continued monitoring ensures onchocerciasis cannot reinvade the area of the OCP.[14]
In 1992, the Onchocerciasis Elimination Programme for the Americas (OEPA), which also relies on ivermectin, was launched.[15]
In 1995, the African Programme for Onchocerciasis Control (APOC) began covering another 19 countries, mainly relying upon the use of ivermectin. Its goal is to set up a community-directed supply of ivermectin for those who are infected. In these ways, transmission has declined.[16]
Treatment
In mass drug administration (MDA) programmes, the treatment for onchocerciasis is ivermectin (trade name: Mectizan); infected people can be treated with two doses of ivermectin, six months apart, repeated every three years. The drug paralyses and kills the microfilariae causing fever, itching, and possibly oedema, arthritis and lymphadenopathy. Intense skin itching is eventually relieved, and the progression towards blindness is halted. In addition, while the drug does not kill the adult worm, it does prevent them from producing additional offspring. The drug therefore prevents both morbidity and transmission.
Ivermectin treatment is particularly effective because it only needs to be taken once or twice a year, needs no refrigeration, and has a wide margin of safety, with the result that it has been widely given by minimally trained community health workers.[17]
Antibiotics
For the treatment of individuals, doxycycline is used to kill the Wolbachia bacteria that live in adult worms. This adjunct therapy has been shown to significantly lower microfilarial loads in the host, and may have activity against the adult worms, due to the symbiotic relationship between Wolbachia and the worm.[18][19] In four separate trials over ten years with various dosing regimens of doxycycline for individualized treatment, doxycycline was found to be effective in sterilizing the female worms and reducing their numbers over a period of four to six weeks. Research on other antibiotics, such as rifampicin, has shown it to been effective in animal models at reducing Wolbachia both as an alternative and as an adjunct to doxycycline.[20] However, doxycycline treatment requires daily dosing for at least four to six weeks, making it more difficult to administer in the affected areas.[17]
Ivermectin
Ivermectin kills the parasite by interfering with the nervous system and muscle function, in particular, by enhancing inhibitory neurotransmission. The drug binds to and activates glutamate-gated chloride channels (GluCls).[17] These channels, present in neurons and myocytes, are not invertebrate-specific, but are protected in vertebrates from the action of ivermectin by the blood-brain barrier.[17] Ivermectin is thought to irreversibly activate these channel receptors in the worm, eventually causing an inhibitory postsynaptic potential (IPSP). The chance of a future action potential occurring in synapses between neurons decreases and the nematodes experience flaccid paralysis followed by death.[21][22][23]
Ivermectin is directly effective against the larval stage microfilariae of O. volvulus; they are paralyzed and can be killed by eosinophils and macrophages. It does not kill adult females (macrofilariae), but does cause them to cease releasing microfilariae, perhaps by paralyzing the reproductive tract.[17]
Since 1988, ivermectin has been provided free of charge for use in humans by Merck through the Mectizan donation program (MDP). The MDP works together with ministries of health and nongovernmental development organisations, such as the World Health Organization, to provide free ivermectin to those who need it in endemic areas.[24]
A study of 2501 people in Ghana showed the prevalence rate doubled between 2000 and 2005 despite treatment, suggesting the parasite is developing resistance to the drug.[20][25][26] A clinical trial of another antiparasitic agent, moxidectin (manufactured by Wyeth), began on July 1, 2009 (NCT00790998).[27]
Epidemiology
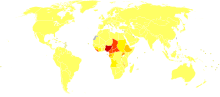 Disability-adjusted life year for onchocerciasis per 100,000 inhabitants
Disability-adjusted life year for onchocerciasis per 100,000 inhabitants no dataless than 1010-5050-6060-7070-8080-9090-100100-150150-200200-300300-400more than 400
no dataless than 1010-5050-6060-7070-8080-9090-100100-150150-200200-300300-400more than 400About 99% of onchocerciasis cases occur in Africa.[4] As of 2008, about 18 million people were infected with this parasite; about 300,000 had been permanently blinded.[28] Onchocerciasis is currently endemic in 30 African countries, Yemen, and isolated regions of South America.[29] Over 85 million people live in endemic areas, and half of these reside in Nigeria. Another 120 million people are at risk for contracting the disease. Due to the vector’s breeding habitat, the disease is more severe along the major rivers in the northern and central areas of the continent, and severity declines in villages farther from rivers.[citation needed] Travelers who do not stay long in those areas have little risk of developing the disease, as it requires prolonged exposure to the fly bites, and parasite introduction.
According to a 2002 WHO report, onchocerciasis has not caused a single death, but its global burden is 987,000 disability adjusted life years (DALYs). The severe pruritis alone accounts for 60% of the DALYs. Infection reduces the host’s immunity and resistance to other diseases, which results in an estimated reduction in life expectancy of 13 years.[29]
Research
Animal models for the disease are somewhat limited, as the parasite only lives in primates, but there are close parallels. Litomosoides sigmodontis , which will naturally infect cotton rats, has been found to fully develop in BALB/c mice. Onchocerca ochengi, the closest relative of O. volvulus, lives in intradermal cavities in cattle, and is also spread by black flies. Both systems are useful, but not exact, animal models.[30]
See also
- Carter Center River Blindness Program
- List of parasites (human)
- Neglected diseases
- Rodolfo Robles
- United Front Against Riverblindness
References
- ^ a b c "Water-related Diseases: Onchocerciasis". World Health Organization. http://www.who.int/water_sanitation_health/diseases/oncho/en/. Retrieved 2010-04-26.
- ^ Willey JM, Sherwood L, Woolverton CJ, Prescott LM (2009). Prescott's Principles of Microbiology. McGraw Hill Higher Education. pp. 645. ISBN 9780077213411. OCLC 181068277.
- ^ "Causes of river blindness". Sightsavers International. Archived from the original on 2007-10-15. http://web.archive.org/web/20071015154331/http://sightsavers.org/What+We+Do/Eye+Conditions/River+Blindness/World1629.html. Retrieved 2008-01-28. (archived 2007-10-15)
- ^ a b "Status of onchocerciasis in APOC countries". World Health Organization. 2008. http://www.who.int/apoc/onchocerciasis/status/en/index.html. Retrieved 2010-04-26.
- ^ ROBLES R. Enfermedad nueva en Guatemala. La Juventud Médica 1917; 17: 97-115.
- ^ Okulicz JF. "Onchocerciasis (River Blindness)". eMedicine. http://www.emedicine.com/derm/topic637.htm#section~treatment. Retrieved 2008-01-28.
- ^ a b Marty AM. "Filariasis". eMedicine. http://emedicine.medscape.com/article/1109642-overview. Retrieved 2009-10-22.
- ^ a b c d e f g h James, William D.; Berger, Timothy G.; Elston, Dirk M; Odom, Richard B. (2006). Andrews' Diseases of the Skin: clinical dermatology (10th ed.). Saunders Elsevier. ISBN 0-7216-2921-0. OCLC 62736861.
- ^ Baldo L, Desjardins CA, Russell JA, Stahlhut JK, Werren JH (2010-02-17). "Accelerated microevolution in an outer membrane protein (OMP) of the intracellular bacteria Wolbachia". BMC Evol Biol 10: 10:48. doi:10.1186/1471-2148-10-48. PMC 2843615. PMID 20163713. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2843615.
- ^ a b Wani, M.G. (February 2008). Onchocerciasis. [Southern Sudan Medical Journal].
- ^ Ali MM, Baraka OZ, AbdelRahman SI, Sulaiman SM, Williams JF, Homeida MM, Mackenzie CD (15 February 2003). "Immune responses directed against microfilariae correlate with severity of clinical onchodermatitis and treatment history". Journal of Infectious Diseases 187 (4): 714–7. doi:10.1086/367709. JSTOR 30085595. PMID 12599094.
- ^ Murdoch ME, Hay RJ, Mackenzie CD, Williams JF, Ghalib HW, Cousens S, Abiose A, Jones BR (1993 Sep). "A clinical classification and grading system of the cutaneous changes in onchocerciasis". Br J Dermatol 129 (3): 260–9. doi:10.1111/j.1365-2133.1993.tb11844.x. PMID 8286222.
- ^ http://microblog.me.uk/420
- ^ "Onchocerciasis Control Programme (OCP)". Programmes and Projects. World Health Organization. http://www.who.int/blindness/partnerships/onchocerciasis_OCP/en/index.html. Retrieved 2010-06-15.
- ^ "Onchocerciasis Elimination Program for the Americas (OEPA)". Programmes and Projects. World Health Organization. http://www.who.int/blindness/partnerships/onchocerciasis_oepa/en/index.html. Retrieved 2010-06-15.
- ^ "African Programme for Onchocerciasis Control (APOC)". Programmes and Projects. World Health Organization. http://www.who.int/blindness/partnerships/APOC/en/index.html. Retrieved 2010-06-15.
- ^ a b c d e Rea PA, Zhang V, Baras YS (2010). "Ivermectin and River Blindness". American Scientist 98 (4): 294–303. http://www.americanscientist.org/issues/feature/2010/4/ivermectin-and-river-blindness.
- ^ Trattler, Bill; Gladwin, Mark (2007). Clinical Microbiology Made Ridiculously Simple. Miami: MedMaster. ISBN 0-940780-81-X. OCLC 156907378.
- ^ Taylor MJ, Bandi C, Hoerauf A (2005). "Wolbachia bacterial endosymbionts of filarial nematodes". Adv. Parasitol. 60: 245–84. doi:10.1016/S0065-308X(05)60004-8. PMID 16230105. http://linkinghub.elsevier.com/retrieve/pii/S0065-308X(05)60004-8.
- ^ a b Hoerauf A (2008). "Filariasis: new drugs and new opportunities for lymphatic filariasis and onchocerciasis". Current Opinion in Infectious Diseases 21 (6): 673–81. doi:10.1097/QCO.0b013e328315cde7. PMID 18978537.
- ^ Yates DM, Wolstenholme AJ (August 2004). "An ivermectin-sensitive glutamate-gated chloride channel subunit from Dirofilaria immitis". International Journal for Parasitology 34 (9): 1075–81. doi:10.1016/j.ijpara.2004.04.010. PMID 15313134.
- ^ Harder A (2002). "Chemotherapeutic approaches to nematodes: current knowledge and outlook". Parasitology Research 88 (3): 272–7. doi:10.1007/s00436-001-0535-x. PMID 11954915.
- ^ Wolstenholme AJ, Rogers AT (2005). "Glutamate-gated chloride channels and the mode of action of the avermectin/milbemycin anthelmintics". Parasitology 131 (Suppl:S85-95): S85–95. doi:10.1017/S0031182005008218. PMID 16569295.
- ^ Thylefors B, Alleman MM, Twum-Danso NA (2008 May). "Operational lessons from 20 years of the Mectizan Donation Program for the control of onchocerciasis". Trop Med Int Health 13 (5): 689–96. doi:10.1111/j.1365-3156.2008.02049.x. PMID 18419585.
- ^ "River blindness resistance fears". BBC News. 2007-06-14. http://news.bbc.co.uk/2/hi/health/6753003.stm. Retrieved 2007-06-15.
- ^ Osei-Atweneboana MY, Eng JK, Boakye DA, Gyapong JO, Prichard RK (June 2007). "Prevalence and intensity of Onchocerca volvulus infection and efficacy of ivermectin in endemic communities in Ghana: a two-phase epidemiological study". Lancet 369 (9578): 2021–9. doi:10.1016/S0140-6736(07)60942-8. PMID 17574093. http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(07)60942-8.
- ^ [No author listed] (11 July 2009). "Fighting river blindness and other ills". Lancet 374 (9684): 91. doi:10.1016/S0140-6736(09)61262-9. PMID 19595328. (editorial)
- ^ "What is river blindness?". Sightsavers International. Archived from the original on 2007-12-15. http://web.archive.org/web/20071215140210/http://www.sightsavers.org/What+We+Do/Eye+Conditions/River+Blindness/World1622.html. Retrieved 2008-01-28.
- ^ a b "Epidemiology". Stanford University. 2006. http://www.stanford.edu/class/humbio103/ParaSites2006/Onchocerciasis/Epidemiology.html.
- ^ Allen JE, Adjei O, Bain O, Hoerauf A, Hoffmann WH, Makepeace BL, Schulz-Key H, Tanya VN, Trees AJ, Wanji S, Taylor DW (April 2008). "Of mice, cattle, and humans: the immunology and treatment of river blindness". PLoS Negl Trop Dis 2 (4): e217. doi:10.1371/journal.pntd.0000217. PMC 2323618. PMID 18446236. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2323618.
External links
- Onchocerciasis, Southern Sudan Medical Journal
- Onchocerciasis research project at the University of Tuebingen
- Mectizan Donation Program
- River blindness documentary "37 Million and Counting" by Aaron Edell
- SightSavers
- What is River Blindness?, CBM International
- CDC Parasites of public health concern
- American NGDO treating river blindness in the Democratic Republic of the Congo
Eye disease · pathology of the eye (H00–H59, 360–379) Adnexa eyelid: inflammation (Stye, Chalazion, Blepharitis) · Entropion · Ectropion · Lagophthalmos · Blepharochalasis · Ptosis · Blepharophimosis · Xanthelasma · eyelash (Trichiasis, Madarosis)conjunctiva: Conjunctivitis (Allergic conjunctivitis) · Pterygium · Pinguecula · Subconjunctival hemorrhageGlobe sclera: Scleritis
cornea: Keratitis (Herpetic keratitis, Acanthamoeba keratitis, Fungal keratitis) · Corneal ulcer · Photokeratitis · Thygeson's superficial punctate keratopathy · Corneal dystrophy (Fuchs', Meesmann) · Keratoconus · Keratoconjunctivitis sicca · Keratoconjunctivitis · Corneal neovascularization · Kayser-Fleischer ring · Arcus senilis · Band keratopathyLensRetinaRetinitis (Chorioretinitis, Cytomegalovirus retinitis) · Retinal detachment · Retinoschisis · Ocular ischemic syndrome/Central retinal vein occlusion · Retinopathy (Bietti's crystalline dystrophy, Coats disease, Diabetic retinopathy, Hypertensive retinopathy, Retinopathy of prematurity) · Macular degeneration · Retinitis pigmentosa · Retinal haemorrhage · Central serous retinopathy · Macular edema · Epiretinal membrane · Macular pucker · Vitelliform macular dystrophy · Leber's congenital amaurosis · Birdshot chorioretinopathyOtherPathways Other binocularAmblyopia · Leber's congenital amaurosis · Subjective (Asthenopia, Hemeralopia, Photophobia, Scintillating scotoma) · Diplopia · Scotoma · Anopsia (Binasal hemianopsia, Bitemporal hemianopsia, Homonymous hemianopsia, Quadrantanopia) · Color blindness (Achromatopsia, Dichromacy, Monochromacy) · Nyctalopia (Oguchi disease) · Blindness/Low visionOtherEye infections M: EYE
anat(g/a/p)/phys/devp/prot
noco/cong/tumr, epon
proc, drug(S1A/1E/1F/1L)
Diseases of poverty Diseases of poverty Neglected diseases Cholera · Chagas disease · African Sleeping Sickness · Schistosomiasis · Guinea worm · River blindness · LeishmaniasisMiscellaneous Categories:- Parasites
- Nematodes
- Tropical diseases
- Helminthiases
- Neglected diseases
- Parasitic infestations, stings, and bites of the skin
Wikimedia Foundation. 2010.