- Ofloxacin
-
Ofloxacin 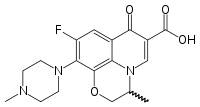
Systematic (IUPAC) name (RS)-7-fluoro-2-methyl-6-(4-methylpiperazin-1-yl)-10-oxo-4-oxa-1-azatricyclo[7.3.1.05,13]trideca-5(13),6,8,11-tetraene-11-carboxylic acid Clinical data Trade names Floxin, Ocuflox AHFS/Drugs.com monograph MedlinePlus a691005 Pregnancy cat. C(US) Legal status ℞-only (US) Routes Oral, IV, topical (eye drops and ear drops) Pharmacokinetic data Bioavailability 85% - 95% Protein binding 32% Half-life 8–9 hours Identifiers CAS number 82419-36-1 
ATC code J01MA01 ,S01AX11, S02AA16 PubChem CID 4583 DrugBank APRD00502 ChemSpider 4422 
UNII A4P49JAZ9H 
KEGG D00453 
ChEBI CHEBI:7731 
ChEMBL CHEMBL4 
Synonyms (±)-9-fluoro-2,3-dihydro-3-methyl-10-(4-methyl-1-piperazinyl)-7-oxo-7H-pyrido[1,2,3-de][1,4]benzoxazine-6-carboxylic acid Chemical data Formula C18H20FN3O4 Mol. mass 361.368 g/mol SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Ofloxacin is a synthetic chemotherapeutic antibiotic of the fluoroquinolone drug class considered to be a second-generation fluoroquinolone.[1][2] The original brand, Floxin, has been discontinued by the manufacturer in the United States on 18 June 2009, though generic equivalents continue to be available.
Ofloxacin was first patented in 1982 (European Patent Daiichi) and received approval from the U.S. Food and Drug Administration (FDA) on December 28, 1990. Ofloxacin is sold under a wide variety of brand names as well as generic drug equivalents, for oral and intravenous administration. Ofloxacin is also available for topical use, as eye drops and ear drops (marketed as Ocuflox and Floxin Otic respectively in the United States).
Ofloxacin is a racemic mixture, which consists of 50% levofloxacin (the biologically active component) and 50% of its “mirror image” or enantiomer dextrofloxacin.[3] When levofloxacin disks were not available in early clinical trials, a 5-pg ofloxacin disk was substituted. The U.S. Food and Drug Administration (FDA) medical reviewers considered the two drugs to be one and the same and hence interchangeable.[4][5]
Like other quinolones, ofloxacin has been associated with a significant number of serious adverse drug reactions, such as tendon damage (including spontaneous tendon ruptures) and peripheral neuropathy (which may be irreversible); such reactions may manifest long after therapy had been completed, and, in severe cases, may result in life-long disabilities.[6] Ofloxacin has also been associated with severe psychiatric adverse reactions.
Hepatotoxicity has also been reported with the use of ofloxacin.[7][8] Case reports of hepatitis have been published for the older fluoroquinolones including ciprofloxacin, ofloxacin, and norfloxacin.[7][9][10][11]
History
Ofloxacin was developed as a broader-spectrum analog of norfloxacin, the first fluoroquinolone antibiotic,[12] Ofloxacin was first patented in 1982 (European Patent Daiichi) and received U.S. Food and Drug Administration (FDA) approval December 28, 1990. One of the first major adverse reactions noted with Ofloxacin were psychiatric in nature. Ofloxacin can cause serious psychiatric side effects with up to 25% of such patients suffering such reactions.[13][14] This reaction was detailed within Stephen Fried’s 1999 book: “Bitter Pills”[15]
In the United States name branded ofloxacin is rarely used anymore, having been discontinued by the manufacturer, Ortho McNeil Janssen, a subsidiary of Johnson & Johnson.[16] Johnson and Johnson's annual sales of Floxin in 2003 was approximately $30 million, where as their combined sales of Levaquin/Floxin exceeded $ 1.15 billion in the same year.[17][18] However generic use continues. The FDA website lists Floxin (Ortho McNeil Jannsen) as being discontinued, with just a few generic equivalents still in use. The otic solution continues to be listed as being available both as an original drug as well as a generic equivalent.
During the 2008 Johnson & Johnson shareholder’s meetings, the safety of both ofloxacin and levofloxacin were called into question. Paul Cahan, a shareholder who had suffered severe and continuing adverse reactions to ofloxacin, publicly challenged Johnson and Johnson’s CEO, William Weldon, to adhere to the company’s credo. This credo states in part “to put the needs and well-being of the people we serve first”. Mr. Cahan requested additional warnings be added to the package inserts for both ofloxacin and levofloxacin.[19][20]
During the 2009 meeting, yet another shareholder who alleges to have been crippled by these drugs, raised these same issues having seen no significant changes in the warnings (regarding the issues raised during the 2008 meeting). Once again a public request for stronger warnings for both ofloxacin and levofloxacin was made. Though the FDA requested additional Black Box Warnings concerning the tendon issues in 2008, these warnings were still not present in the inserts for ofloxacin or levofloxacin that are being dispensed by pharmacists in 2009, prompting this second request by a shareholder for stronger warnings and Dear Doctor Letters
Medical uses
Oral and I.V. Floxin is not licensed by the FDA for use in children due to the risk of serious reversible and irreversible injury to the musculoskeletal system. Other fluoroquinolones do have a limited licensed uses in children but are generally not recommended due to safety concerns.[21][22] Ofloxacin (and its derivatives) has also been associated with a few isolated reports of unexplained pediatric fatalities.[23][24] Children (those under 18) are also at an increased risk of bone, joint, or tendon toxicities.[25]
Prescribing ofloxacin in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of severe adverse drug reactions.[25]
In the adult population ofloxacin is limited to the treatment of proven serious and life threatening bacterial infections such as:
- Acute bacterial exacerbations of chronic bronchitis
- Community-acquired pneumonia
- Uncomplicated skin and skin structure infections
- Nongonococcal urethritis and cervicitis
- Uncomplicated cystitis
- Complicated urinary tract infections
- Acute, uncomplicated urethral and cervical gonorrhea.
Ofloxacin has not been shown to be effective in the treatment of syphilis.[25] Floxin is now considered to be contraindicated for the treatment of certain sexually transmitted diseases by some experts due to bacterial resistance.[26]
Available forms
Ofloxacin for systemic use is available as tablets (multiple strengths), oral solution (250 mg/ml), and injectable solution (multiple strengths). It is also used as eye drops (trade name Exocin, known as Ocuflox in the United States) and ear drops (Floxin Otic).
Ofloxacin is also used in animals. Its veterinary formulation is sold as Marfloxacin (not to be confused with marbofloxacin, another veterinary-use fluoroquinolone).
Mode of action
Ofloxacin is a broad-spectrum antibiotic that is active against both Gram-positive and Gram-negative bacteria. It functions by inhibiting DNA gyrase, a type II topoisomerase, and topoisomerase IV,[27] which is an enzyme necessary to separate replicated DNA, thereby inhibiting cell division.
The fluoroquinolones interfere with DNA replication by inhibiting an enzyme complex called DNA gyrase. This can also affect mammalian cell replication. In particular, some congeners of this drug family display high activity not only against bacterial topoisomerases, but also against eukaryotic topoisomerases and are toxic to cultured mammalian cells and in vivo tumor models. Although the quinolone is highly toxic to mammalian cells in culture, its mechanism of cytotoxic action is not known. Quinolone induced DNA damage was first reported in 1986.[28]
Recent studies have demonstrated a correlation between mammalian cell cytotoxicity of the quinolones and the induction of micronuclei.[29][30][31] As such some fluoroquinolones may cause injury to the chromosome of eukaryotic cells.[32][33][34][35][36]
There is debate as to whether or not this DNA damage is to be considered one of the mechanisms of action concerning the severe and non abating adverse reactions experienced by some patients following fluoroquinolone therapy.[37][38][39]
Contraindications
As noted above, under licensed use, ofloxacin is now considered to be contraindicated for the treatment of certain sexually transmitted diseases by some experts due to bacterial resistance.[26]
Due to growing prevalence of antibiotic resistance to the fluoroquinolones in southeast Asia, the use of ofloxacin in patients who have been to southeast Asia is increasingly being contraindicated.[40]
Caution in patients with liver disease.[41] The excretion of ofloxacin may be reduced in patients with severe liver function disorders (e.g., cirrhosis with or without ascites).
Ofloxacin is also considered to be contraindicated within the pediatric population, pregnancy, nursing mothers, patients with psychiatric illnesses and in patients with epilepsy or other seizure disorders.
Pregnancy
Research indicates that the fluoroquinolones can rapidly cross the blood-placenta and blood-milk barrier, and are extensively distributed into the fetal tissues. Peak concentration in human breast milk is similar to levels attained in plasma. Breast-feeding mothers who take ofloxacin may expose their infants to severe adverse reactions. [42][43] Other flouroquinolones have also been reported as being present in the mother’s milk and are passed on to the nursing child, which may increases the risk of the child suffering from this syndrome as well, even though the child had never been prescribed or taken any of the drugs found within this class.[44][45]
The data on the safety of the fluoroquinolones in pregnancy contains conflicting reports and is to be considered incomplete due to the lack of adequate studies. But it should be noted that several studies have reported spontaneous abortions following the exposure to the fluoroquinolones during pregnancy, as well as therapeutic/elective abortions due to the perceived, as well as actual, risk of birth defects.[46][47] However, within one study the authors concluded that the use of quinolones during pregnancy may in some cases be necessary; e.g. drug resistant serious infections,[47] but if safer antibiotics such as penicillin, cephalosporins or erythromycin are an option they should be used instead due to their clearer safety profile.[46]
In regards to Floxin, within a prospective follow-up study of 93 women treated with ofloxacin during pregnancy, the authors report that there was a higher than expected (11.9%) malformation rate among the infants.[48] According to the March of Dimes only about 3 to 5 percent of all pregnancies result in children born with birth defects.
For this reason the prescribing of ofloxacin is contraindicated during pregnancy due to the risk of spontaneous abortions and birth defects. Such spontaneous abortions and birth defects have also been found with other drugs within this class, i.e. Ciprofloxacin,[49] Pefloxacin,[50] Norfloxacin[51] and Nalidixic acid.[52] It is generally accepted that the fluoroquinolone class should not be used to treat women who are pregnant due to such risks.[53][54][55]
Pediatric use
Oral and IV fluoroquinolones including ofloxacin are not licensed by the FDA for use in children due to the risk of permanent injury to the musculoskeletal system. Within one study it was stated that the pediatric patient has a 3.8% chance of experiencing a serious musculoskeletal adverse event.[56]
However the two most recent pediatric studies involving the use of levofloxacin, the biologically active component of floxin, indicates that the pediatric patient has a greater than 50% chance of experiencing one or more adverse reactions. Which would be consistent with the studies found within the NDA (new drug application) for Levofloxacin[4] which showed and ADR rate in excess of 40%, as well as a number of reported fatalities. Within the first study[57] it is stated that “Of the 712 subjects evaluable for safety, 275 (52%) levofloxacin-treated subjects experienced one or more adverse event.... Serious adverse events were reported in 33 (6%) levofloxacin-treated subjects.... Two serious adverse events in levofloxacin-treated subjects resulted in fatal outcomes.” Within the second study[58] it is stated that “Of the 204 subjects evaluable for safety, 122 experienced one or more adverse events...Twelve subjects (6%) discontinued study drug due to an adverse event.... Seven subjects (3%) experienced 8 serious adverse events.” (circa 2007)
As such the current ban on the use of ofloxacin and other fluoroquinolones in the pediatric population appears to be both reasonable and supported by various clinical studies. The risk of permanent injury may outweigh the potential benefits. Within the United States the FDA has stated that it is their intention to pursue the licensing of the fluoroquinolones for pediatric use in spite of the evidence presented at that 62 Meeting of the Anti-Infective Drugs Advisory Committee (1996) that the fluoroquinolones cause irreversible joint damage in the pediatric population.[59]
Adverse effects
Serious adverse events occur more commonly with fluoroquinolones than with any other antibiotic drug classes.[60][61] There has been a number of regulatory actions taken as a result of such adverse reactions associated with ofloxacin therapy, which included published warnings,[62][63][64] additional warnings and safety information added to the package inserts which includes a black box warning concerning spontaneous tendon ruptures and the resultant permanent disability.[65] In 2008 the FDA had also requested that the manufacturers of Floxin (as well as generic ofloxacin) issue a "Dear Doctor Letter" to inform physicians of this black box warning.
In 2004 the FDA requested new warning labels to be added to all of the fluoroquinolones, including ofloxacin, regarding peripheral neuropathy (irreversible nerve damage), tendon damage, heart problems (prolonged QT interval / torsades de pointes), pseudomembranous colitis, rhabdomyolysis (muscle wasting), Stevens-Johnson syndrome, as well as concurrent usage of NSAIDs contributing to the severity of these reactions. Subsequently changes were made to the package insert for Floxin to state that Floxin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria,[66] and additional warnings concerning irreversible peripheral neuropathy and Torsades de pointes being associated with floxin therapy were added.[67] In 2007 warnings regarding fatal Clostridium difficile associated diarrhea (CDAD: reported to occur over two months after the administration),[68] severe photosensitivity/phototoxicity reactions and hepatic failure (including fatal cases) and Toxic Epidermal Necrolysis (TEN) were added to the package inserts.[69]
The psychiatric adverse events,[70][71][72][73] as well as central nervous system[74][75][76] and peripheral nervous system[76] associated with ofloxacin has been well documented within the literature.
Adverse reactions may manifest during, as well as after fluoroquinolone therapy.[77]
Liver damage and dysglycemia has been associated with ofloxacin.[78][79][80][80] Additionally in 2005 acute rhabdomyolysis had been associated with ofloxacin/levofloxacin therapy.[81]
Some groups refer to the presentation of these multiple adverse events as "fluoroquinolone toxicity". These groups of patients claim to have suffered serious long term harm to their health from using fluoroquinolones. This has led to a class action lawsuit being filed by these groups as well as action by the consumer advocate group Public Citizen.[82][83] Partly as a result of the efforts of Public Citizen the FDA requested a Black Box Warnings on all fluoroquinolones advising consumers of the possible toxic effects of fluoroquinolones on tendons.[84]
Severe hepatotoxicity has been reported as noted above. Reports of hepatic or hypersensitivity vasculitis occurring as a result of ofloxacin therapy have also been reported.[85][86] Older patients may have an increased risk of tendinopathy (including rupture), especially with concomitant corticosteroid use and such patients may also be more susceptible to prolongation of the QT interval.[25] Patients with known prolongation, those with hypokalemia, or being treated with other drugs that prolong the QT interval should avoid the use of ofloxacin. Hematologic reactions (including agranulocytosis, thrombocytopenia), and renal toxicities may occur after multiple doses.[25]
Tendon damage
As with all fluoroquinolones, there is a possibility of spontaneous tendon rupture.[87] Such ruptures may occur both during therapy and long after therapy has been discontinued; there are documented cases where rupture has occurred six months after therapy.[87] The risk of tendon damage is greater in people taking corticosteroids and in the elderly.[88] Since July 2008, all systemic fluoroquinolones (those taken internally, not as eye drops or ear drops) available in the United States were requested, by the FDA, to carry a black box warning of the risk of tendon damage. However, the addition of this warning was not mandatory.[88]
Interactions
Ofloxacin has been reported to interact with a significant number of other drugs, as well as a number of herbal and natural supplements. Such interactions increased the risk of cardiotoxicity and arrhythmias, anticoagulant effects, the formation of non-absorbable complexes, as well as increasing the risk of toxicity.[89] Concurrent administration of ofloxacin, with magnesium or aluminum antacids, sucralfate or products containing calcium, iron or zinc may substantially decrease the absorption of ofloxacin, resulting in serum and urine levels considerably lower than desired.
Specific drug interaction studies do not appear to have been conducted with ofloxacin. However, the systemic administration of some fluoroquinolones has been shown to interfere with the metabolism of caffeine, elevate plasma concentrations of theophylline and enhance the effects of the warfarin and its derivatives. Some fluoroquinolones exert an inhibitory effect on the cytochrome P-450 system, thereby reducing theophylline clearance and increasing theophylline blood levels. Co-administration may dangerously increase coumadin warfarin activity, therefore International Normalized Ratio (INR) should be monitored closely. Such drug interactions appear to be related to the structural changes of the quinolone ring and the inhibitory effect on the cytochrome P-450 system. As such, these drug interactions involving the fluoroquinolones appear to be drug specific rather than a class effect.
The use of NSAIDs (Non Steroid Anti Inflammatory Drugs) while undergoing fluoroquinolone therapy is contra-indicated due to the risk of severe CNS adverse reactions, including but not limited to seizure disorders. Fluoroquinolones with an unsubstituted piperazinyl moiety at position 7 have the potential to interact with NSAIDs and/or their metabolites, resulting in antagonism of GABA neurotransmission.[90] Patients have reported reactions to NSAIDS long after completion of fluoroquinolone therapy, but there does not appear to be any research that would either confirm or deny this association other than these anecdotal reports.
The fluoroquinolones have been shown to increase the anticoagulant effect of Acenocoumarol, Anisindione, and Dicumarol. Additionally there is an increase the risk of cardiotoxicity and arrhythmias when co administered with drugs such as Dihydroquinidine barbiturate, Quinidine, and Quinidine barbiturate.[89] The fluoroquinolones have also been reported to interact with the GABA A receptor and cause neurological symptoms; this effect is augmented by certain non-steroidal anti-inflammatory drugs.[91]
Current or past treatment with oral corticosteroids is associated with an increased risk of Achilles tendon rupture, especially in elderly patients who are also taking the fluoroquinolones.[92]
A possible interaction between oral hypoglycemic drugs (e.g., glyburide/glibenclamide) or with insulin and fluoroquinolone antimicrobial agents have been reported resulting in a potentiation of the hypoglycemic action of these drugs.[25]
Overdose
There is only limited information on overdose with ofloxacin. Current advise for the management of an acute overdose of ofloxacin is emptying of the stomach, along with close observation, and making sure that the patient is appropriately hydrated. Hemodialysis or peritoneal dialysis is of only limited effectiveness.[25] Overdose may result in central nervous system toxicity, cardiovascular toxicity, tendon/articular toxicity, and hepatic toxicity[93] as well as renal failure and seizure.[93] Seizures have however, been reported to occur at therapeutic dosage as well as severe psychiatric reactions.[13][14][15]
Pharmacology
The bioavailability of ofloxacin in the tablet form is approximately 98% following oral administration reaching maximum serum concentrations within one to two hours. Between 65% and 80% of an administered oral dose of ofloxacin is excreted unchanged via the kidneys within 48 hours of dosing. Therefore elimination is mainly by renal excretion. However, four to eight percent of an ofloxacin dose is excreted in the feces. This would indicate a small degree of biliary excretion as well. Plasma elimination half-life is approximately 4 to 5 hours in patients and approximately 6.4 to 7.4 hours in elderly patients.[25]
Pharmacokinetics
"After multiple-dose administration of 200 mg and 300 mg doses, peak serum levels of 2.2 μg/mL and 3.6 μg/mL, respectively, are predicted at steady-state. In vitro, approximately 32% of the drug in plasma is protein bound. Floxin is widely distributed to body tissues. Ofloxacin has been detected in blister fluid, cervix, lung tissue, ovary, prostatic fluid, prostatic tissue, skin, and sputum. Pyridobenzoxazine ring appears to decrease the extent of parent compound metabolism. Less than 5% is eliminated by the kidneys as desmethyl or N-oxide metabolites; 4% to 8% by feces."[25][94]
There are a number of the endogenous compounds that have been reported to be affected by ofloxacin as inhibitors, alteraters and depletors. See the latest package insert for Ofloxacin for additional details.[25]
Dosage
Ofloxacin should only be administered as described within the Dosage Guidelines table found within the most current package insert. The status of the patient’s renal function and hepatic function must also be taken into consideration to avoid an accumulation that may lead to a fatal drug overdose. Ofloxacin is eliminated primarily by renal excretion. However, the drug is also metabolized and partially cleared through the liver. Modification of the dosage is required using the table found within the package insert for those with impaired liver or kidney function (Particularly for patients with severe renal dysfunction). However, since the drug is known to be substantially excreted by the kidneys, the risk of toxic reactions to this drug may be greater in patients with impaired renal function. The duration of treatment depends upon the severity of infection and the usual duration is 7 to 14 days.[25]
NOTE: The patient’s serum levels should be monitored during therapy to avoid a drug overdose. See the most current Package Insert for proper dosing guidelines and relevant warnings/precautions.
Susceptible bacteria
Aerobic Gram-positive microorganisms
- Staphylococcus aureus (methicillin-susceptible strains)
- Streptococcus pneumoniae (penicillin-susceptible strains)
- Streptococcus pyogenes
Aerobic Gram-negative microorganisms
- Citrobacter (diversus) koseri
- Enterobacter aerogenes
- Escherichia coli
- Haemophilus influenzae
- Klebsiella pneumoniae
- Neisseria gonorrhoeae
- Proteus mirabilis
- Pseudomonas aeruginosa
Other microorganisms
- Chlamydia trachomatis
Referencing the latest package insert for Floxin.
Additional regulatory history
See also Levaquin regulator history
Floxin:
- December 28, 1990 The approval of the new drug application (NDA for floxacin).
- December 28, 1990 to March 6, 2004 Fourteen years worth of data has been removed from the FDA website. As such, this information is no longer available. The NDA (new drug application) documents have also been removed from the FDA site.[95] As such the regulatory history begins fourteen years after initial approval beginning with the 2004 changes:
- September 15, 2004[67] The Tendon effects subsection was revised which minimized the warnings concerning that spontaneous tendon ruptures may be increased in patients receiving corticosteroids with Floxin (ofloxacin—floxacin) and other quinolones. The statement that tendon rupture can occur “at any time” was removed.
- June 14, 2006[96]
The Indications and Usage section of the package insert was revised as follows: “Uncomplicated skin and skin structure infections due to methicillin-susceptible Staphylococcus aureus, Streptococcus pyogenes, or Proteus mirabilis.”
- June 19, 2007[69]
The Tendon effects subsection was revised to minimize the warnings stating that the risk of serious tendon disorders is higher in those over 65 years of age, especially those on steroids.
- October 3, 2008[97]
Addition of Black Box Warning.
- February 12, 2009[98]
Issuance of a Medication Guide and revisions to include new safety information including the addition of the Black Box Warning to the Medication Guide. The FDA had determined that Ofloxacin poses a serious and significant public health concern, requiring the distribution of a Medication Guide
Note: Although the FDA had requested that the revised labeling (which were to include the Black Box Warnings) accompany the package inserts for any newly shipped products (effective January 2009) there are continuing reports that as of September 2009, that the products continue to contain the older labels, and not the revised labels, and that the Medication Guides (absent of the Black Box Warnings) were not made available for distribution.[97]
Notice given to the FDA of the discontinuance of Floxacin by the manufacturer effective June 18, 2009.
History of the black box warnings
Musculoskeletal disorders attributed to use of quinolone antibiotics were first reported in the medical literature in 1972, as an adverse reaction to nalidixic acid.[101] Rheumatic disease after use of a fluoroquinolone (norfloxacin) was first reported eleven years later.[102] In a 1995 letter published in the New England Journal of Medicine, representatives of the U.S. Food and Drug Administration (FDA) stated that the agency would "update the labeling [package insert] for all marketed fluoroquinolones to include a warning about the possibility of tendon rupture."[103]
By August 1996, the FDA had not taken action, and the consumer advocacy group Public Citizen filed a petition with the FDA prompting the agency to act.[104] Two months later, the FDA published an alert in the FDA Medical Bulletin and requested that fluoroquinolone package inserts be amended to include information on this risk.[105]
In 2005, the Illinois Attorney General filed a petition with the FDA seeking black box warnings and "Dear Doctor" letters emphasizing the risk of tendon rupture; the FDA responded that it had not yet been able to reach a decision on the matter, though they had been reviewing this issue since 1995.[106] In 2006, Public Citizen, supported by the Illinois Attorney General, renewed its demand of ten years prior for a Black Box Warning.[106][107] In January 2008, Public Citizen filed suit in Federal Court to compel the FDA to respond to their 2006 petition.[108][109] On July 7, 2008 the FDA requested that the makers of systemic-use fluoroquinolones add a boxed warning regarding tendon rupture, and to develop a Medication Guide for patients.[88] The package inserts for Ciprofloxacin, Avelox (moxifloxacin), Proquin XR, Factive (gemifloxacin), Floxin (ofloxacin), Noroxin (norfloxacin) and Levaquin (levofloxacin) were amended on September 8, 2008 to include these new warnings.[65][110] Bayer, which manufactures Cipro, Avelox and Proquin XR, issued a Dear Healthcare Professional letter on October 22, 2008 concerning these changes.[111] Ortho-McNeil, the manufacturers of Levaquin and Floxin, issued a similar letter in November.[112] through the Health Care Notification Network, a registration-only website that distributes drug alerts only to licensed healthcare professionals.
Review of the FDA website indicates that the generic versions of the fluoroquinolones have not been updated to include this Black Box Warning as of June 2009. And there are numerous reports that this information has not been dessiminated to the pharmacist, the generic products (as well name branded products) continue to contain the previous labels that are absent of this warning, and the Medication Guide has not been made available to the pharmicist or physician for distribution.
Although the FDA had requested that the revised labeling (which included the Black Box Warnings)[97] accompany the package inserts for any newly shipped products (effecticve January 2009) there are continuing reports that as of September 2009, that the products continue to contain the older labels, and not the revised labels, and are absent of the required medication guides.
Antibiotic abuse and bacterial resistance
Resistance to ofloxacin and other fluoroquinolones may evolve rapidly, even during a course of treatment. Numerous pathogens, including Staphylococcus aureus, enterococci, and Streptococcus pyogenes now exhibit resistance worldwide.[113]
Years ago the FDA had added warnings regarding the proper use of ofloxacin within the package insert to combat such antibiotic abuse, advising physicians that ofloxacin: "...should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria....".[25]
Normally ofloxacin should only be used in patients who have failed at least one prior therapy. Reserved for the use in patients who are seriously ill and may soon require immediate hospitalization.[114]
The use of the ofloxacin and other fluoroquinolones had increased threefold in an emergency room environment in the United States between 1995 and 2002, while the use of safer alternatives such as macrolides declined significantly.[115][116]
Within a recent study concerning the proper use of ofloxacin and other fluoroquinolones in the emergency room it was revealed that 99% of these prescriptions were in error. Out of the one hundred total patients studied, eighty one received a fluoroquinolone for an inappropriate indication. Out of these cases, forty three (53%) were judged to be inappropriate because another agent was considered first line, twenty seven (33%) because there was no evidence of a bacterial infection to begin with (based on the documented evaluation), and eleven (14%) because of the need for such therapy was questionable. Out of the nineteen patients who received a fluoroquinolone for an appropriate indication, only one patient out of one hundred received both the correct dose and duration of therapy.[117]
Ofloxacin and other fluoroquinolones had become the most commonly prescribed class of antibiotics to adults in 2002. Nearly half (42%) of these prescriptions were for conditions not approved by the FDA, such as acute bronchitis, otitis media, and acute upper respiratory tract infection, according to a study that was supported in part by the Agency for Healthcare Research and Quality.[116][118] Additionally they are commonly prescribed for medical conditions that are not even bacterial to begin with, such as viral infections, or those to which no proven benefit exists.
Current litigation
The manufacturers (Johnson and Johnson/Ortho McNeil) of ofloxacin are currently embroiled in litigation concerning levofloxacin/ofloxacin in regards to spontaneous tendon ruptures. There are a significant number of cases currently pending before the United States District Court, District of Minnesota, involving spontaneous tendon ruptures alleged to be caused by these drugs. On June 13, 2008 a Judicial Panel On Multidistrict Litigation (MDL) granted the Plaintiffs’ motion to centralize individual and class action lawsuits involving levaquin in the District of Minnesota over objection of Defendants, Johnson and Johnson / Ortho McNeil.[83] Such ruptures have also been associated with ofloxacin, as well as other drugs found within this class.[119][120][121][122][123][124]
Douglas & London in New York, who represents more than 200 such plaintiffs from 38 States, expects to file many additional product liability suits involving levofloxacin/ofloxacin. As plaintiffs attorney, lawyer Michael London had recently asked the New Jersey Supreme Court to accord mass-tort treatment to their suits against the manufacturer, Johnson & Johnson subsidiary Ortho-McNeil Pharmaceutical Inc.[125]
The various manufacturers have countered these allegations stating that they believe that these drugs are both safe and effective antibiotics, well tolerated with a minimum of side-effects, that such reactions are “rare” and the benefits of such therapy outweigh the perceived risks.[126]
Several class action lawsuits had been filed in regards to the adverse reactions suffered by those exposed to Ciprofloxacin during the Anthrax scare of 2001 as well.[127][128][129]
Package insert links
See also
- Adverse effects of fluoroquinolones
- Fluoroquinolone
- Quinolone
- Levofloxacin
- Cetraxal
References
- ^ Nelson, JM.; Chiller, TM.; Powers, JH.; Angulo, FJ. (Apr 2007). "Fluoroquinolone-resistant Campylobacter species and the withdrawal of fluoroquinolones from use in poultry: a public health success story.". Clin Infect Dis 44 (7): 977–80. doi:10.1086/512369. PMID 17342653.
- ^ Kawahara, S. (December 1998). "[Chemotherapeutic agents under study]". Nippon Rinsho 56 (12): 3096–9. PMID 9883617.
- ^ http://www.wvnd.uscourts.gov/Opinions/orthoorder.pdf
- ^ a b R.W. Johnson (April 24, 2007). "Levaquin (Levofloxacin) NDA 20634 Approved: 12/20/1996". USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/nda/96/020634_levaquin_toc.cfm. Retrieved July 22, 2009.
- ^ Davis, R.; Bryson, H. M. (1994). "Levofloxacin". Drugs 47 (4): 677–700. doi:10.2165/00003495-199447040-00008. PMID 7516863.
- ^ Clodagh Sheehy (August 2, 2008). "Warning over two types of antibiotic". Republic of Ireland. http://www.herald.ie/national-news/warning-over-two-types-of-antibiotic-1445498.html. Retrieved July 17, 2009.
- ^ a b Blum, A (1991). "Ofloxacin-induced acute severe hepatitis.". Southern medical journal 84 (9): 1158. doi:10.1097/00007611-199109000-00027. PMID 1891746.
- ^ González Carro P, Huidobro ML, Zabala AP, Vicente EM (June 2000). "Fatal subfulminant hepatic failure with ofloxacin". Am. J. Gastroenterol. 95 (6): 1606. doi:10.1111/j.1572-0241.2000.02118.x. PMID 10894622.
- ^ Jones, SF; Smith (1997). "Quinolones may induce hepatitis.". BMJ (Clinical research ed.) 314 (7084): 869. PMC 2126221. PMID 9093098. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2126221.
- ^ Hautekeete, ML; Kockx; Naegels; Holvoet; Hubens; Kloppel (1995). "Cholestatic hepatitis related to quinolones: a report of two cases.". Journal of hepatology 23 (6): 759–60. doi:10.1016/0168-8278(95)80045-X. PMID 8750178.
- ^ Villeneuve, JP; Davies; Côté (1995). "Suspected ciprofloxacin-induced hepatotoxicity.". The Annals of pharmacotherapy 29 (3): 257–9. PMID 7606070.
- ^ Mark B. Abelson, MD; Stephen J. Hallas (April 15, 2003). "The New Antibiotics: The Path of Least Resistance". Review of Ophthalmology. http://www.revophth.com/index.asp?page=1_303.htm. Retrieved October 3, 2009.
- ^ a b Hall, CE; Keegan, H; Rogstad, KE (September 2003). "Psychiatric side effects of ofloxacin used in the treatment of pelvic inflammatory disease.". Int J STD AIDS 14 (9): 636–7. doi:10.1258/095646203322301121. PMID 14511503.
- ^ a b Amsden, GW; Graci, DM; Cabelus, LJ; Hejmanowski, LG (July 1999). "A randomized, crossover design study of the pharmacology of extended-spectrum fluoroquinolones for pneumococcal infections." (PDF). Chest 116 (1): 115–9. doi:10.1378/chest.116.1.115. PMID 10424513. http://chestjournal.chestpubs.org/content/116/1/115.full.pdf.
- ^ a b http://www.randomhouse.com/author/results.pperl?authorid=9367
- ^ Douglas C. Throckmorton (May 19, 2009). "Novartis Pharmaceuticals Corp. et al.; Withdrawal of Approval of 92 New Drug Applications and 49 Abbreviated New Drug Applications". Trading Markets. http://www.tradingmarkets.com/.site/news/Stock%20News/2335053/. "see also FDA docket number FDA-2009-N-0211"
- ^ Business Wire (September 2, 2003). "Teva Announces Approval of Ofloxacin Tablets, 200 mg, 300 mg, and 400 mg". Business Wire. http://findarticles.com/p/articles/mi_m0EIN/is_2003_Sept_2/ai_107154169/.
- ^ Johnson and johnson (2003). "Building on a foundation of health" (PDF). Shareholder. http://files.shareholder.com/downloads/JNJ/0x0x180977/C0E8971E-DC6F-4DB2-AF7E-00ED716010C8/jnj_2003annual.pdf.
- ^ http://www.investor.jnj.com/webcasts-presentations.cfm 2009 shareholders meeting; time stamped at 1 hour 42 minutes.
- ^ http://fqresearch.org/j_and_j.
- ^ Chalumeau, M., M; Tonnelier, S; D'athis, P; Tréluyer, JM; Gendrel, D; Bréart, G; Pons, G; Pediatric Fluoroquinolone Safety Study Investigators, Investigators (June 2003). "Fluoroquinolone Safety in Pediatric Patients: A Prospective, Multicenter, Comparative Cohort Study in France" (PDF). Pediatrics 111 (6 Pt 1): e714. doi:10.1542/peds.111.6.e714. ISSN 0031-4005. PMID 12777590. http://pediatrics.aappublications.org/cgi/reprint/111/6/e714.
- ^ Dolui, SK.; Das, M.; Hazra, A. (Apr-Jun 2007). "Ofloxacin-induced reversible arthropathy in a child.". J Postgrad Med 53 (2): 144–5. doi:10.4103/0022-3859.32220. PMID 17495385.
- ^ The Pediatric Infectious Disease Journal: March 1999 - Volume 18 - Issue 3 - pp 245–248 Original Studies A comparative study of ofloxacin and cefixime for treatment of typhoid fever in children Phuong, Cao Xuan Thanh Md; Kneen, Rachel Mrcp; Anh, Nguyen Tuyet Md; Luat, Truong Dinh Md; White, Nicholas J. Frcp; Parry, Christopher M. Mrcp; The Dong Nai Pediatric Center Typhoid Study Group “unexplained death of a 6-year-old patient receiving ofloxacin...” http://journals.lww.com/pidj/Abstract/1999/03000/A_comparative_study_of_ofloxacin_and_cefixime_for.7.aspx
- ^ http://www.fdable.com/advanced_aers_query/a394b5b5480c21476cd297cfcc986819 3431736 00Q1 3452229 DEATH DE LEVOFLOXACIN (01/19/00 R.W. JOHNSON 13 year old male) 3461848 00Q1 SUDDEN DEATH UNEXPLAINED DE LEVOFLOXACIN (01/19/00 R.W. JOHNSON 13 year old male)
- ^ a b c d e f g h i j k l Ortho-McNeil-Janssen Pharmaceuticals, Inc (2008). "FLOXIN Tablets (Ofloxacin Tablets)" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/019735s059lbl.pdf.
- ^ a b Susan Blank; Julia Schillinger (May 14, 2004). "DOHMH ALERT #8:Fluoroquinolone-resistant gonorrhea, NYC". USA: New York County Medical Society. http://www.nycms.org/article_view.php3?view=947&part=1. Retrieved July 22, 2009.
- ^ Drlica K, Zhao X (1 September 1997). "DNA gyrase, topoisomerase IV, and the 4-quinolones". Microbiol Mol Biol Rev. 61 (3): 377–92. PMC 232616. PMID 9293187. http://mmbr.asm.org/cgi/pmidlookup?view=long&pmid=9293187.
- ^ Hussy P, Maass G, Tümmler B, Grosse F, Schomburg U (June 1986). "Effect of 4-quinolones and novobiocin on calf thymus DNA polymerase alpha primase complex, topoisomerases I and II, and growth of mammalian lymphoblasts". Antimicrob. Agents Chemother. 29 (6): 1073–8. PMC 180502. PMID 3015015. http://aac.asm.org/cgi/reprint/29/6/1073.pdf.
- ^ Hosomi JA. Maeda Y. Oomori T. Irikura and T. Yokota (1988). "Mutagenicity of norfloxacin and AM-833 in bacteria and mammalian cells". Rev. Infect. Dis 10 (Suppl. 1): S148–S149.
- ^ Forsgren A, Bredberg A, Pardee AB, Schlossman SF, Tedder TF, A (May 1987). "Effects of ciprofloxacin on eucaryotic pyrimidine nucleotide biosynthesis and cell growth" (PDF). Antimicrob. Agents Chemother. 31 (5): 774–9. ISSN 0066-4804. PMC 174831. PMID 3606077. http://aac.asm.org/cgi/reprint/31/5/774.pdf.
- ^ Gootz TD, Barrett JF, Sutcliffe JA, TD (January 1990). "Inhibitory effects of quinolone antibacterial agents on eucaryotic topoisomerases and related test systems". Antimicrob. Agents Chemother. 34 (1): 8–12. ISSN 0066-4804. PMC 171510. PMID 2158274. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=171510.
- ^ Elsea SH, Osheroff N, Nitiss JL, SH (July 1992). "Cytotoxicity of quinolones toward eukaryotic cells. Identification of topoisomerase II as the primary cellular target for the quinolone CP-115,953 in yeast". J. Biol. Chem. 267 (19): 13150–3. ISSN 0021-9258. PMID 1320012. http://www.jbc.org/cgi/reprint/267/19/13150.
- ^ Enzmann H, Wiemann C, Ahr HJ, Schlüter G, H (April 1999). "Damage to mitochondrial DNA induced by the quinolone Bay y 3118 in embryonic turkey liver". Mutat. Res. 425 (2): 213–24. doi:10.1016/S0027-5107(99)00044-5. ISSN 0027-5107. PMID 10216214.
- ^ Kashida Y, Sasaki YF, Ohsawa K, Y (October 2002). "Mechanistic study on flumequine hepatocarcinogenicity focusing on DNA damage in mice". Toxicol. Sci. 69 (2): 317–21. doi:10.1093/toxsci/69.2.317. ISSN 1096-6080. PMID 12377980. http://toxsci.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12377980.
- ^ Thomas A, Tocher J, Edwards DI, A (May 1990). "Electrochemical characteristics of five quinolone drugs and their effect on DNA damage and repair in Escherichia coli". J. Antimicrob. Chemother. 25 (5): 733–44. doi:10.1093/jac/25.5.733. ISSN 0305-7453. PMID 2165050. http://jac.oxfordjournals.org/cgi/reprint/25/5/733.
- ^ "Fluoroquinolones and Quinolones". The American Academy of Optometry (British Chapter). http://www.academy.org.uk/pharmacy/fluoroq.htm. Retrieved January 29, 2009.
- ^ Al-Soud, Yaseen A.; Al-masoudi, Najim A (2003). "A new class of dihaloquinolones bearing N'-aldehydoglycosylhydrazides, mercapto-1,2,4-triazole, oxadiazoline and a-amino ester precursors: synthesis and antimicrobial activity". J. Braz. Chem. Soc 14 (5). doi:10.1590/S0103-50532003000500014. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-50532003000500014&lng=es&nrm=iso&tlng=es. "Nevertheless, some quinolones cause injury to the chromosome of eukaryotic cells.21,22 These findings prompted us to optimize the substituent at C-3, by..."
- ^ Yaseen A. Al-Soud a and Najim A. Al-Masoudi (2003). "A New Class of Dihaloquinolones Bearing N’-Aldehydoglycosylhydrazides, Mercapto-1,2,4-triazole, Oxadiazoline and α-Amino Ester Precursors: Synthesis and Antimicrobial Activity". J. Braz. Chem. Soc 14 (5): 790–796. doi:10.1590/S0103-50532003000500014. http://jbcs.sbq.org.br/jbcs/2003/v14_n5/13-048-02.pdf. "Although the current quinolones are not considered to be potent inhibitors of eucaryotic topoisomerases, some effects on these and other enzymes involved with DNA replication have been observed"
- ^ Sissi C, Palumbo M, C (November 2003). "The quinolone family: from antibacterial to anticancer agents". Curr Med Chem Anticancer Agents 3 (6): 439–50. doi:10.2174/1568011033482279. ISSN 1568-0118. PMID 14529452. http://openurl.ingenta.com/content/nlm?genre=article&issn=1568-0118&volume=3&issue=6&spage=439&aulast=Sissi. "The present review focuses on the structural modifications responsible for the transformation of an antibacterial into an anticancer agent. Indeed, a distinctive feature of drugs based on the quinolone structure is their remarkable ability to target different type II topoisomerase enzymes. In particular, some congeners of this drug family display high activity not only against bacterial topoisomerases, but also against eukaryotic topoisomerases and are toxic to cultured mammalian cells and in vivo tumor models."
- ^ Centers for Disease Control and Prevention (CDC) (October 1995). "Fluoroquinolone resistance in Neisseria gonorrhoeae—Colorado and Washington, 1995". MMWR Morb Mortal Wkly Rep. 44 (41): 761–4. PMID 7565558. http://www.cdc.gov/mmwr/preview/mmwrhtml/00039305.htm.
- ^ Coban S, Ceydilek B, Ekiz F, Erden E, Soykan I (October 2005). "Levofloxacin-induced acute fulminant hepatic failure in a patient with chronic hepatitis B infection". Ann Pharmacother 39 (10): 1737–40. doi:10.1345/aph.1G111. PMID 16105873.
- ^ Pharmacotherapy: Official Journal of the American College of Clinical Pharmacy Print ISSN: 0277-0008 Volume: 25 | Issue: 1 Cover date: January 2005 Page(s): 116-118
- ^ Nardiello S, Pizzella T, Ariviello R (March 2002). "Risks of antibacterial agents in pregnancy.". Le infezioni in medicina : rivista periodica di eziologia, epidemiologia, diagnostica, clinica e terapia delle patologie infettive 10 (1): 8–15. PMID 12700435.
- ^ Shin HC, Kim JC, Chung MK (September 2003). "Fetal and maternal tissue distribution of the new fluoroquinolone DW-116 in pregnant rats". Comp. Biochem. Physiol. C Toxicol. Pharmacol. 136 (1): 95–102. doi:10.1016/j.cca.2003.08.004. PMID 14522602.
- ^ Dan M, Weidekamm E, Sagiv R, Portmann R, Zakut H (February 1993). "Penetration of fleroxacin into breast milk and pharmacokinetics in lactating women". Antimicrob. Agents Chemother. 37 (2): 293–6. PMC 187655. PMID 8452360. http://aac.asm.org/cgi/pmidlookup?view=long&pmid=8452360.
- ^ a b Schaefer C, Amoura-Elefant E, Vial T (November 1996). "Pregnancy outcome after prenatal quinolone exposure. Evaluation of a case registry of the European Network of Teratology Information Services (ENTIS)". Eur. J. Obstet. Gynecol. Reprod. Biol. 69 (2): 83–9. doi:10.1016/0301-2115(95)02524-3. PMID 8902438. http://linkinghub.elsevier.com/retrieve/pii/0301211595025243.
- ^ a b Loebstein R, Addis A, Ho E (June 1998). "Pregnancy outcome following gestational exposure to fluoroquinolones: a multicenter prospective controlled study". Antimicrob. Agents Chemother. 42 (6): 1336–9. PMC 105599. PMID 9624471. http://aac.asm.org/cgi/content/full/42/6/1336?view=long&pmid=9624471.
- ^ Schaefer, C.; Amoura-Elefant, E.; Vial, T.; Ornoy, A.; Garbis, H.; Robert, E.; Rodriguez-Pinilla, E.; Pexieder, T. et al. (November 1996). "Pregnancy outcome after prenatal quinolone exposure. Evaluation of a case registry of the European Network of Teratology Information Services (ENTIS).". Eur J Obstet Gynecol Reprod Biol 69 (2): 83–9. doi:10.1016/0301-2115(95)02524-3. PMID 8902438.
- ^ Schluter (1989), Bomford et al (1993), Rosa (1993) Michigan MSS, and Schaefer et al (1996)
- ^ Schaefer et al (1996)
- ^ Rosa (1993) Michigan MSS
- ^ Deonna and Guignard (1974), Asscher (1977), Murray (1981), Czeizel et al (2001) Hyngarian CCSCA, and (Belton and Jones 1965)
- ^ Sullivan, Donald L. (2001). The expectant mother's guide to prescription and nonprescription drugs, vitamins, home remedies, and herbal products. New York: St. Martin's Griffin. pp. 55–56. ISBN 0-312-25190-4.
- ^ Compliance a Key Consideration: Fewer Options in Pregnancy http://www.medscape.com/viewarticle/406494_9 “Tetracyclines (e.g. doxycycline) and fluoroquinolones (e.g. ofloxacin) should not be used to treat women who are pregnant because of associated adverse events in the fetus. “
- ^ http://www.healthline.com/yodocontent/pregnancy/treatment-chlamydial-infection.html “The treatment for gonorrhea in pregnant women is essentially the same as in non-pregnant women. The notable exception is that quinolone antibiotics, like ciprofloxacin and ofloxacin, should not be used since these antibiotics inhibit DNA formation and can cause birth defects.”
- ^ Noel GJ, Bradley JS, Kauffman RE (October 2007). "Comparative safety profile of levofloxacin in 2523 children with a focus on four specific musculoskeletal disorders". Pediatr. Infect. Dis. J. 26 (10): 879–91. doi:10.1097/INF.0b013e3180cbd382. PMID 17901792.
- ^ "SYNOPSIS". USA. http://download.veritasmedicine.com/PDF/CR002392_CSR.pdf. Retrieved January 29, 2009.
- ^ "SYNOPSIS". USA. http://download.veritasmedicine.com/PDF/CR002389_CSR.pdf. Retrieved January 29, 2009.
- ^ "FOOD AND DRUG ADMINISTRATION, ANTI-INFECTIVE DRUGS ADVISORY COMMITTEE, 62nd MEETING, Wednesday, November 19". USA: FDA. Archived from the original on 2009. http://fqresearch.org/pdf_files/62nd_fda_meeting.pdf.
- ^ Owens Rc, Jr; Ambrose (2005). "Antimicrobial safety: focus on fluoroquinolones.". Clinical Infectious Diseases 41 Suppl 2: S144–57. doi:10.1086/428055. PMID 15942881.
- ^ Iannini, PB (2007). "The safety profile of moxifloxacin and other fluoroquinolones in special patient populations.". Current medical research and opinion 23 (6): 1403–13. doi:10.1185/030079907X188099. PMID 17559736.
- ^ http://www.fqresearch.org/text_documents/FDA_Medical_Bulletin_1996.doc
- ^ U S Food and Drug Administration (July 8, 2008). "FDA Requests Boxed Warnings on Fluoroquinolone Antimicrobial Drugs" (PDF). USA: FDA. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116919.htm. Retrieved September 5, 2009.
- ^ US Food and Drug Administration (2008). "Fluoroquinolone Antimicrobial Drugs [ciprofloxacin (marketed as Cipro and generic ciprofloxacin), ciprofloxacin extended release (marketed as Cipro XR and Proquin XR), gemifloxacin (marketed as Factive), levofloxacin (marketed as Levaquin), moxifloxacin (marketed as Avelox), norfloxacin (marketed as Noroxin), and ofloxacin (marketed as Floxin and generic ofloxacin)"]. USA. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm084316.htm. Retrieved 5 September 2009.[dead link]
- ^ a b US Food and Drug Administration. "Drugs at FDA: FDA Approved Drug Products". USA: FDA. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Label_ApprovalHistory#apphist. Retrieved September 5, 2009.
- ^ Renata Albrecht (2004). "NDA 19-735/S-051" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2004/19735slr051ltr.pdf.
- ^ a b Renata Albrecht (September 15, 2004). "NDA 19-735/S-052, S-053" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2004/19735s052,053ltr.pdf.
- ^ Renata Albrecht (May 16, 2007). "NDA 19-735/S-056" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2007/019735s056ltr.pdf.
- ^ a b Renata Albrecht (June 19, 2007). "NDA 19-735/S-057" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2007/019735s057ltr.pdf.
- ^ Salm, EF.; Egberts, AC.; Maartense, E.; Hart, W.; Stricker, BH. (May 1994). "[Psychotic reactions during administration of quinolones]". Ned Tijdschr Geneeskd 138 (21): 1080–2. PMID 8202181.
- ^ Hall, CE.; Keegan, H.; Rogstad, KE. (September 2003). "Psychiatric side effects of ofloxacin used in the treatment of pelvic inflammatory disease.". Int J STD AIDS 14 (9): 636–7. doi:10.1258/095646203322301121. PMID 14511503.
- ^ Hollweg, M.; Kapfhammer, HP.; Krupinski, M.; Möller, HJ. (January 1997). "[Psychopathological syndromes in treatment with gyrase inhibitors]". Nervenarzt 68 (1): 38–47. PMID 9132619.
- ^ Zaudig, M.; von Bose, M.; Weber, MM.; Bremer, D.; Zieglgänsberger, W. (January 1989). "Psychotoxic effects of ofloxacin.". Pharmacopsychiatry 22 (1): 11–5. doi:10.1055/s-2007-1014570. PMID 2710806.
- ^ De Bleecker, JL.; Vervaet, VL.; De Sarro, A. (June 2004). "Reversible orofacial dyskinesia after ofloxacin treatment.". Mov Disord 19 (6): 731–2. doi:10.1002/mds.20053. PMID 15197723.
- ^ Walton, GD.; Hon, JK.; Mulpur, TG. (December 1997). "Ofloxacin-induced seizure.". Ann Pharmacother 31 (12): 1475–7. PMID 9416384.
- ^ a b Thomas, RJ.; Reagan, DR. (February 1996). "Association of a Tourette-like syndrome with ofloxacin.". Ann Pharmacother 30 (2): 138–41. PMID 8835045.
- ^ Saint F, Gueguen G, Biserte J, Fontaine C, Mazeman E (September 2000). "[Rupture of the patellar ligament one month after treatment with fluoroquinolone"] (in French). Rev Chir Orthop Reparatrice Appar Mot 86 (5): 495–7. PMID 10970974. http://www.masson.fr/masson/MDOI-RCO-09-2000-86-5-0035-1040-101019-ART7.
- ^ Jones, SF.; Smith, RH. (March 1997). "Quinolones may induce hepatitis.". BMJ 314 (7084): 869. PMC 2126221. PMID 9093098. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2126221.
- ^ Blum, A. (September 1991). "Ofloxacin-induced acute severe hepatitis.". South Med J 84 (9): 1158. doi:10.1097/00007611-199109000-00027. PMID 1891746.
- ^ a b González Carro, P.; Huidobro, ML.; Zabala, AP.; Vicente, EM. (June 2000). "Fatal subfulminant hepatic failure with ofloxacin.". Am J Gastroenterol 95 (6): 1606. doi:10.1111/j.1572-0241.2000.02118.x. PMID 10894622.
- ^ Hsiao, SH.; Chang, CM.; Tsao, CJ.; Lee, YY.; Hsu, MY.; Wu, TJ. (January 2005). "Acute rhabdomyolysis associated with ofloxacin/levofloxacin therapy.". Ann Pharmacother 39 (1): 146–9. doi:10.1345/aph.1E285. PMID 15562138.
- ^ "Public Citizen Warns of Cipro Dangers". USA: Consumer affairs. August 30, 2006. http://www.consumeraffairs.com/news04/2006/08/pubcit_cipro.html. Retrieved September 7, 2009.
- ^ a b Judge John R. Tunheim. "Levaquin MDL". USA: US Courts. http://www.mnd.uscourts.gov/MDL-Levaquin/index.shtml. Retrieved September 7, 2009.
- ^ "FDA orders 'black box' label on some antibiotics". CNN. July 8, 2008. http://www.cnn.com/2008/HEALTH/07/08/antibiotics.risk/index.html. Retrieved July 8, 2008.
- ^ Pipek R, Vulfsons S, Wolfovitz E, Har-Shai Y, Taran A, Peled IJ (February 1996). "Case report: ofloxacin-induced hypersensitivity vasculitis". Am. J. Med. Sci. 311 (2): 82–3. doi:10.1097/00000441-199602000-00005. PMID 8615379.
- ^ González Carro P, Huidobro ML, Zabala AP, Vicente EM (June 2000). "Fatal subfulminant hepatic failure with ofloxacin". Am. J. Gastroenterol. 95 (6): 1606. doi:10.1111/j.1572-0241.2000.02118.x. PMID 10894622.
- ^ a b Khaliq Y, Zhanel GG (June 2003). "Fluoroquinolone-associated tendinopathy: a critical review of the literature". Clinical Infectious Diseases 36 (11): 1404–10. doi:10.1086/375078. PMID 12766835.
- ^ a b c "FDA Requests Boxed Warnings on Fluoroquinolone Antimicrobial Drugs" (Press release). U.S. Food and Drug Administration. July 8, 2008. http://www.fda.gov/bbs/topics/NEWS/2008/NEW01858.html. Retrieved October 11, 2008.
- ^ a b "Showing drug card for Ofloxacin (DB01165)". Canada: DrugBank. February 19, 2009. http://www.drugbank.ca/drugs/DB01165.
- ^ Domagala, Jm (April 1994). "Structure-activity and structure-side-effect relationships for the quinolone antibacterials.". The Journal of antimicrobial chemotherapy 33 (4): 685–706. doi:10.1093/jac/33.4.685. ISSN 0305-7453. PMID 8056688.
- ^ Brouwers JR, JR (July 1992). "Drug interactions with quinolone antibacterials". Drug Saf 7 (4): 268–81. doi:10.2165/00002018-199207040-00003. ISSN 0114-5916. PMID 1524699.
- ^ van der Linden PD, Sturkenboom MC, Herings RM, Leufkens HM, Rowlands S, Stricker BH, PD (August 2003). "Increased risk of achilles tendon rupture with quinolone antibacterial use, especially in elderly patients taking oral corticosteroids". Arch. Intern. Med. 163 (15): 1801–7. doi:10.1001/archinte.163.15.1801. ISSN 0003-9926. PMID 12912715. http://archinte.ama-assn.org/cgi/content/full/163/15/1801.
- ^ a b Nelson, Lewis H.; Flomenbaum, Neal; Goldfrank, Lewis R.; Hoffman, Robert Louis; Howland, Mary Deems; Neal A. Lewin (2006). Goldfrank's toxicologic emergencies. New York: McGraw-Hill, Medical Pub. Division. ISBN 0-07-143763-0. http://books.google.com/?id=cvJuLqBxGUcC&pg=PA849&dq=goldfranks+Fluoroquinolone+toxicity.
- ^ Drugs.com. "Complete Ofloxacin information from Drugs.com". http://www.drugs.com/ppa/ofloxacin.html.
- ^ "Floxin (Ofloxacin) Tablets" (PDF). USA: FDA. May 5, 2006. http://www.accessdata.fda.gov/drugsatfda_docs/nda/pre96/019735_s001_FloxinTOC.cfm.
- ^ Renata Albrecht, M.D. (June 14, 2006). "NDA 19-735/S-055" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2006/019735s055LTR.pdf.
- ^ a b c Renata Albrecht (June 19, 2007). "NDA 19-735/S-057" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2008/019735s059ltr.pdf.
- ^ Ozlem Belen (February 12, 2009). "NDA 19-735/S-060" (PDF). USA: FDA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2009/019735s060ltr.pdf.
- ^ Douglas C. Throckmorton (May 19, 2009). "Novartis Pharmaceuticals Corp. et al.; Withdrawal of Approval of 92 New Drug Applications and 49 Abbreviated New Drug Applications". USA: Trading Markets. http://www.tradingmarkets.com/.site/news/Stock%20News/2335053/.
- ^ see also FDA Notices Vol. 74, No. 095 [Docket No. FDA-2009-N-0211]
- ^ Bailey RR, Natale R, Linton AL (October 1972). "Nalidixic acid arthralgia". Can Med Assoc J 107 (7): 604 passim. PMC 1940945. PMID 4541768. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1940945.
- ^ Bailey RR, Kirk JA, Peddie BA (July 1983). "Norfloxacin-induced rheumatic disease". N Z Med J 96 (736): 590. PMID 6223241.
- ^ Szarfman A, Chen M, Blum MD (January 1995). "More on fluoroquinolone antibiotics and tendon rupture" (letter). N Engl J Med 332 (3): 193. doi:10.1056/NEJM199501193320319. PMID 7800023.
- ^ "Petition to Require a Warning on All Fluoroquinolone Antibiotics (HRG Publication #1399)". Public Citizen. August 1, 1996. http://www.citizen.org/publications/release.cfm?ID=6595. Retrieved December 27, 2008.
- ^ "Reports of adverse events with fluoroquinolones" (Doc). FDA Medical Bulletin 26 (3). October 1996. http://www.fqresearch.org/text_documents/FDA_Medical_Bulletin_1996.doc.
- ^ a b "Madigan, Public Citizen, petition FDA for "black box" warning regarding potential adverse effects of certain popular antibiotics" (Press release). Office of the Illinois Attorney General. August 29, 2006. http://www.illinoisattorneygeneral.gov/pressroom/2006_08/20060829.html. Retrieved December 27, 2008. Full text of the 2005 petition and FDA response available from the Fluoroquinolone Toxicity Research Foundation, a U.S. consumer advocacy group.
- ^ "Public Citizen Petitions the FDA to Include a Black Box Warning on Fluoroquinolone Antibiotics (HRG Publication #1781)". Public Citizen. August 29, 2006. http://www.citizen.org/publications/release.cfm?ID=7453. Retrieved December 27, 2008.
- ^ "Public Citizen v. Food and Drug Administration (FDA) (Fluoroquinolone)". Public Citizen. January 3, 2008. http://www.citizen.org/litigation/forms/cases/CaseDetails.cfm?cID=444. Retrieved December 27, 2008.
- ^ Ravn, Karen (August 18, 2008). "Behind the FDA’s ‘black box’ warnings". Los Angeles Times. http://articles.latimes.com/2008/aug/18/health/he-closer18. Retrieved December 27, 2008.
- ^ FDA. "MedWatch: The FDA Safety Information and Adverse Event Reporting Program". USA: FDA. http://www.fda.gov/medwatch. Retrieved August 12, 2009.
- ^ MacCarthy, Paul (October 22, 2008). "Important Change in the Avelox (moxifloxacin hydrochloride) and Cipro (ciprofloxacin) Complete Prescribing Information – Addition of Boxed Warning and Medication Guide Regarding Tendinitis and Tendon Rupture". Bayer HealthCare Pharmaceuticals. http://www.cipro.com/html/pdf/dhpl.pdf. Retrieved December 27, 2008.
- ^ Rosenthal, Norman (November 2008). "Important Change in the LEVAQUIN (Ievofloxacin) Complete Prescribing Information -Addition of Boxed Warning and Medication Guide Regarding Tendinitis and Tendon Rupture". Ortho-McNeil Janssen Scientific Affairs, LLC. http://www.fqresearch.org/pdf_files/Levaquin_11_2008_ortho_mcneil_dear_dr_letter.pdf. Retrieved December 27, 2008.
- ^ M Jacobs, Worldwide Overview of Antimicrobial Resistance. International Symposium on Antimicrobial Agents and Resistance 2005.
- ^ Jim Hoover, for Bayer Corporation, Alaska Pharmacy and Therapeutics Committee March 19, 2004.
- ^ MacDougall, C, C; Guglielmo, Bj, BJ; Maselli, J, J; Gonzales, R, R (March 2005). "Antimicrobial drug prescribing for pneumonia in ambulatory care." (Free full text). Emerging infectious diseases 11 (3): 380–4. ISSN 1080-6040. PMID 15757551. http://www.cdc.gov/ncidod/EID/vol11no03/04-0819.htm.
- ^ a b Linder JA, Huang ES, Steinman MA, Gonzales R, Stafford RS (March 2005). "Fluoroquinolone prescribing in the United States: 1995 to 2002". Am. J. Med. 118 (3): 259–68. doi:10.1016/j.amjmed.2004.09.015. PMID 15745724. http://linkinghub.elsevier.com/retrieve/pii/S0002-9343(04)00711-9.
- ^ Lautenbach, E.; Larosa, LA.; Kasbekar, N.; Peng, HP.; Maniglia, RJ.; Fishman, NO. (March 2003). "Fluoroquinolone utilization in the emergency departments of academic medical centers: prevalence of, and risk factors for, inappropriate use.". Arch Intern Med 163 (5): 601–5. doi:10.1001/archinte.163.5.601. PMID 12622607.
- ^ K08 HS14563 and HS11313
- ^ Khaliq Y, Zhanel GG (June 2003). "Fluoroquinolone-associated tendinopathy: a critical review of the literature". Clin. Infect. Dis. 36 (11): 1404–10. doi:10.1086/375078. PMID 12766835. http://www.journals.uchicago.edu/cgi-bin/resolve?CID30513. "6 cases (6.1%) were reported in association with ofloxacin...."
- ^ Schwald, N.; Debray-Meignan, S. (1999). "Suspected role of ofloxacin in a case of arthalgia, myalgia, and multiple tendinopathy.". Rev Rhum Engl Ed 66 (7-9): 419–21. PMID 10526383.
- ^ Long term outcome after Fluoroquinolones tendinopathies 13/01/2004 14:11:07 P-0077 C Guy (1); Y Murat (1); MN Beyens (1); M Ratrema (1); G Mounier (1); M Ollagnier (1); (1) Centre de Pharmacovigilance, Hôpital Bellevue - CHU St-Etienne, Sant-Etienne
- ^ van der Linden, PD.; Sturkenboom, MC.; Herings, RM.; Leufkens, HM.; Rowlands, S.; Stricker, BH. (2003). "Increased risk of achilles tendon rupture with quinolone antibacterial use, especially in elderly patients taking oral corticosteroids.". Arch Intern Med 163 (15): 1801–7. doi:10.1001/archinte.163.15.1801. PMID 12912715.
- ^ Aouam, K.; El Aïdli, S.; Daghfous, R.; Kastalli, S.; Lakhal, M.; Loueslati, MH.; Belkahia, C. (2004). "[Ofloxacin-induced achilles tendinitis in the absence of a predisposition]". Therapie 59 (6): 653–5. PMID 15789832.
- ^ Uppsala Monitoring Centre. "NATIONALLY CIRCULATED INFORMATION". World Health Organisation. http://www.who-umc.org/DynPage.aspx?id=14335. "Tendon ruptures represent 81 cases for 921 reports of tendon disorders which are related in decreasing order to pefloxacin 1/23130 case per days of treatment, ofloxin, norfloxacin and ciprofloxacin 1/779600 case per days of treatment."
- ^ "Mass-Tort Treatment Sought for Suits Over Ortho-McNeil Antibiotic Levaquin - FDA says Levaquin users are at heightened risk of tendonitis and tendon rupture in the shoulder, biceps, hand and thumb". USA: New Jersey Law Journal. May 13, 2009. http://www.law.com/jsp/article.jsp?id=1202430654875&MassTort_Treatment_Sought_for_Suits_Over_OrthoMcNeil_Antibiotic_Levaquin. Retrieved May 16, 2009.
- ^ In The United States District Court District Of Minnesota Levaquin Products Liability Litigation Mdl No. 08-1943 Court File No. 09-Cv-00812 (JRT) Defendant Johnson & Johnson's Answer To Plaintiff's Complaint Filed May 12, 2009 www.fqresearch.org/pdf_files/232-1.pdf
- ^ "Anthrax Scare Leaves Trail of Cipro Victims - Class Actions filed in Two States". USA: Sheller Ludwig & Sheller. October 17, 2003. http://www.sheller.com/NewsDetails.asp?NewsID=72. Retrieved September 9, 2009.[dead link]
- ^ "LEGAL BRIEF of Postal Employees Cases (EEOC, MSPB, District Courts)". USA: Postal Reporter. http://www.lunewsviews.com/legal_briefs_archives.htm#cipro. Retrieved September 9, 2009.
- ^ Charles P. Goodell, Jr. "Profile". USA: Goodell, DeVries, Leech & Dann, LLP. http://www.gdldlaw.com/content/bio_goodell.htm. Retrieved September 9, 2009.
External links
- Ofloxacin: an overview - A site with its chemical properties and alternate brand names.
- U.S. National Library of Medicine: Drug Information Portal - Ofloxacin
Antibacterials: nucleic acid inhibitors (J01E, J01M) Antifolates
(inhibits
purine metabolism,
thereby inhibiting
DNA and RNA synthesis)Other/ungroupedCombinationsTopoisomerase
inhibitors/
quinolones/
(inhibits
DNA replication)1st g.2nd g.Ciprofloxacin# • Enoxacin‡ • Fleroxacin‡ • Lomefloxacin • Nadifloxacin • Ofloxacin • Norfloxacin • Pefloxacin • Rufloxacin3rd g.4th g.Besifloxacin • Clinafloxacin† • Garenoxacin • Gemifloxacin • Moxifloxacin • Gatifloxacin‡ • Sitafloxacin • Trovafloxacin‡/Alatrofloxacin‡ • PrulifloxacinVet.Related (DG)Anaerobic DNA
inhibitorsNitrofuran derivativesRNA synthesis Otologicals (S02) Anti-infectives Acetic acid • Aluminium acetotartrate • Boric acid • Chloramphenicol • Chlorhexidine • Ciprofloxacin • Clioquinol • Gentamicin • Hydrogen peroxide • Miconazole • Neomycin • Nitrofurazone • Ofloxacin • Polymyxin B • Rifamycin • TetracyclineCorticosteroids Analgesics and anesthetics M: EAR
anat(e/p)/phys/devp
noco/cong, epon
proc, drug(S2)
Categories:- Fluoroquinolone antibiotics
- Piperazines
- Otologicals
- Ophthalmology drugs
- Nitrogen heterocycles
- Oxygen heterocycles
Wikimedia Foundation. 2010.
