- Cinoxacin
-
Cinoxacin 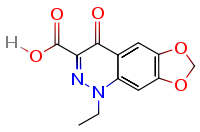
Systematic (IUPAC) name 1-Ethyl- 1,4-Dihydro- 4-oxo [1,3] Dioxolo [4,5-g] Cinnoline- 3-Carboxylic Acid Clinical data AHFS/Drugs.com Micromedex Detailed Consumer Information MedlinePlus a601013 Pregnancy cat. ? Legal status discontinued UK USA Pharmacokinetic data Protein binding 60 to 80% Identifiers CAS number 28657-80-9 ATC code J01MB06 PubChem CID 2762 DrugBank APRD00873 ChemSpider 2660 
UNII LMK22VUH23 
KEGG D00872 
ChEBI CHEBI:3716 
ChEMBL CHEMBL1208 
Chemical data Formula C12H10N2O5 Mol. mass 262.218 g/mol SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Cinoxacin has been discontinued in the U.K.[1] as well the United States, both as a branded drug or a generic.
Cinoxacin was an older synthetic antimicrobial related to the quinolone class of antibiotics with activity similar to Oxolinic Acid and Nalidixic Acid. It was commonly used thirty years ago to treat urinary tract infections in adults. There are reports that cinoxacin had also been used to treat initial and recurrent urinary tract infections and bacterial prostatitis in dogs[2] however this veterinary use was never approved by the United States Food and Drug Administration (FDA). In complicated UTI, the older gyrase-inhibitors such as cinoxacin are no longer indicated.[3]
Contents
History
Cinoxacin is one of the original quinolone drugs, which were introduced in the 1970s. Commonly referred to as the first generation quinolones. This first generation also included other quinolone drugs such as pipemidic acid, and oxolinic acid, but this first generation proved to be only marginal improvements over nalidixic acid. Cinoxacin is similar chemically (and in antimicrobial activity) to oxolonic acid and nalidixic acid. Relative to nalidixic acid, cinoxacin was found to have a slightly greater inhibitory and bactericidal activity. Cinoxacin was patented in 1972 and assigned to Eli Lilly.[4] Eli Lilly obtained approval from the FDA to market cinoxacin in the United States as Cinobac on June 13, 1980. Prior to this cinobac was marketed in the U.K. and Switzerland in 1979.
Oclassen Pharmaceuticals (Oclassen Dermatologics) commenced sales of Cinobac in the United States and Canada back in September 1992, under an agreement with Eli Lilly which granted Oclassen exclusive United States and Canadian distribution rights.[5] Oclassen promoted Cinobac primarily to urologists for the outpatient treatment of initial and recurrent urinary tract infections and prophylaxis. Oclassen Pharmaceuticals was a privately held pharmaceutical company founded in 1985 until acquired by Watson Pharmaceuticals, Inc., in 1997. Watson Pharmaceuticals, Inc., (also incorporated in 1985), having acquired Oclassen Pharmaceuticals (Oclassen Dermatologics) also acquired the marketing rights contained within the agreement with Eli Lilly to market cinobac.[6]
Oddly enough Watson Pharma stated in 1999 that they were marketing cinobac for the treatment of skin diseases[7] (an unapproved use) and in 2001 that they were marketing cinobac as a general pain management product (yet another unapproved use).[8] It appears that this branded version was withdrawn sometime after 2003.
Licensed uses
Urinary tract infections only
Pediatric restrictions
Cinobac is not approved to treat pediatric patients. Prescribing Cinobac to treat an unapproved use (other than Urinary tract infections) within the pediatric, as well as the adult population, does take place rather frequently. The fluoroquinolones are not licensed by the FDA for use in children (other than the exception inhalational anthrax, which is restricted to levaquin and ciprofloxacin) due to the risk of fatalities[9][10] as well as permanent injury to the musculoskeletal system.[11] Although alleged to be effective, neither ciprofloxacin or levofloxacin is considered to be a first line agent for inhalational anthrax in the pediatric population due to severe adverse reactions involving the musculoskeletal system and other serious adverse reactions, including fatalities.[11][12][13][14][15][16]
The CDC revoked its recommendation regarding the use of fluoroquinolones (ciprofloxacin) as a first line agent in treating anthrax (in part) due to the risk of adverse reactions documented within the Antimicrobial Postexposure Prophylaxis for Anthrax study (aka Cipro 60-day study).[17] However, the fluoroquinolones are licensed to treat lower respiratory infections in children with cystic fibrosis in the UK. Within the United States the FDA has stated that it is their intention to pursue the licensing of the fluoroquinolones for pediatric use in spite of the evidence presented at that 62 Meeting of the Anti-Infective Drugs Advisory Committee (Circa 1997) that the fluoroquinolones cause irreversible joint damage in the pediatric population.[18]
Note: Cinoxacin may be licensed for other uses, or restricted, by the various regulatory agencies worldwide.
Availability
250 mg, capsules (prescription only)
Mode of action
Cinoxacin mode of action involves the inhibiting of DNA gyrase, a type II topoisomerase, and topoisomerase iv,[19] which is an enzyme necessary to separate replicated DNA, thereby inhibiting cell division.
Evidence exists that cinoxacin binds strongly to DNA, interfering with synthesis of RNA and, consequently, with protein synthesis.[20] The fluoroquinolones interfere with DNA replication by inhibiting an enzyme complex called DNA gyrase. This can also affect mammalian cell replication. In particular, some congeners of this drug family display high activity not only against bacterial topoisomerases but also against eukaryotic topoisomerases, and are toxic to cultured mammalian cells and in vivo tumor models. Although the quinolone is highly toxic to mammalian cells in culture, its mechanism of cytotoxic action is not known. Quinolone-induced DNA damage was first reported in 1986 (Hussy et al.).[21]
Recent studies have demonstrated a correlation between mammalian cell cytotoxicity of the quinolones and the induction of micronuclei.[22][23][24][25] As such some fluoroquinolones may cause injury to the chromosome of eukaryotic cells.[26][27][28][29][30][31]
There continues to be considerable debate as to whether or not this DNA damage is to be considered one of the mechanisms of action concerning the severe and non-abating adverse reactions experienced by some patients following fluoroquinolone therapy.[32][33][34]
Contraindications
Within the most recent package insert (circa 1999) Cinobac is listed as being contraindicated in patients with a history of hypersensitivity to cinoxacin or other quinolones.
Adverse reactions
See also: Adverse effects of fluoroquinolonesSerious adverse events occur more commonly with fluoroquinolones than with any other antibiotic drug classes.[35] [36] There has been a number of regulatory actions taken as a result of such adverse reactions, which included published warnings,[37][38] additional warnings and safety information added to the package inserts.
In 2004 the FDA requested new warning labels to be added to all of the Fluoroquinolones, regarding Peripheral Neuropathy (irreversible nerve damage),[39] Tendon Damage [40] ,[41] Heart Problems (prolonged QT Interval / Torsades de pointes),[42] Pseudomembranous colitis[43] , Rhabdomyolysis (muscle wasting)[44][45][46] , Steven Johnson Syndrome [47] , as well as concurrent usage of NSAIDs contributing to the severity of these reactions.[48] It is unknown whether or not cinobac was removed from clinical practice prior to this request by the FDA.
Children and the elderly are at a much greater risk of experiencing such adverse reactions.[49] [50] Older patients may have an increased risk of tendinopathy (including rupture), especially with concomitant corticosteroid use, and such patients may also be more susceptible to prolongation of the QT interval. Patients with known prolongation, those with hypokalemia, or being treated with other drugs that prolong the QT interval should avoid the use of cinoxacin. Such reactions may manifest during, as well as long after fluoroquinolone therapy had been discontinued.[51]
Some groups refer to these adverse events as "fluoroquinolone toxicity". These groups of people claim to have suffered serious long term harm to their health from using fluoroquinolones. This has led to a class action lawsuit by people harmed by the use of fluoroquinolones as well as legal action by the consumer advocate group Public Citizen.[52] Partly as a result of the efforts of The State of Illinois and Public Citizen the FDA ordered a black box warnings on all fluoroquinolones advising consumers of the possible toxic effects of fluoroquinolones on tendons.[53]
However, unlike the other drugs found within this class, the safety profile of cinoxacin appears to be rather unremarkable. Adverse drug reactions appear to be limited to the gastrointestinal system and the central nervous system.[54] Hypersensitivity resulting in an anaphylactic reactions (as seen with all drugs found within this class) has also been reported in association with cinoxacin.[55][56] Animal studies have shown that Cinoxacin is associated with renal damage. Such damage appears to be due to the physical trauma resulting from deposition of cinoxacin crystals in the urinary tract.[57] Such crystaluria has also been reported with other drugs in this class.[58] A review of the literature indicates that patients treated with cinoxacin reported fewer adverse drug reactions than those treated with nalidixic acid, furadantin, amoxicillin, or trimethoprim-sulfamethoxazole.[59]
Although phototoxicity and photoallergenicity is well demonstrated experimentally, phototoxicity does not appear to be an issue with cinoxacin.[60] As a result of this safety profile the manufacturer, Eli Lilley states that “cinoxacin perhaps should be reserved only for those patients with organisms resistant to usual first-line agents or those who fail to respond to therapy with these agents.”[61]
Overdose
Symptoms following an overdose of cinoxacin may include anorexia, nausea, vomiting, epigastric distress, and diarrhea. The severity of the epigastric distress and the diarrhea are dose related.[62] Patients who have ingested an overdose of cinoxacin should be kept well hydrated to prevent crystalluria. Forced diuresis, peritoneal dialysis, hemodialysis, or charcoal hemoperfusion have not been established as beneficial for an overdose of cinoxacin.[63]
Pharmacokinetics
Biotransformation is mainly hepatic, with approximately 30-40% metabolized to inactive metabolites. Protein Binding ranges from 60 to 80%. Cinoxacin is rapidly absorbed after oral administration. The presence of food delays absorption but does not affect total absorption. The mean serum half-life is 1.5 hours. Half-life in patients with impaired renal function may exceed 10 hours.[62][64]
Dosing
The usual adult dosage for the treatment of urinary tract infections is 1 g daily, administered orally in 2 or 4 divided doses (500 mg b.i.d. or 250 mg q.i.d. respectively) for 7 to 14 days.
Impaired Renal Function
When renal function is impaired, a reduced dosage must be employed.
Susceptible bacteria
Gram-negative aerobes:
- Enterobacter species
- Escherichia coli
- Klebsiella species
- Proteus mirabilis
- Proteus vulgaris
Note: Enterococcus species, Pseudomonas species, and Staphylococcus species are resistant.
Regulatory history
The regulatory history in the United States regarding cinoxacin has been deleted from the FDA site. Though approved in 1980, there is only one document (circa 2002) available for reference. Twenty two years worth or regulatory history concerning cinoxacin is unavailable.
History of the black box warnings
Musculoskeletal disorders attributed to use of quinolone antibiotics were first reported in the medical literature in 1972, as an adverse reaction to nalidixic acid.[65] Rheumatic disease after use of a fluoroquinolone (norfloxacin) was first reported eleven years later.[66] In a 1995 letter published in the New England Journal of Medicine, representatives of the U.S. Food and Drug Administration (FDA) stated that the agency would "update the labeling [package insert] for all marketed fluoroquinolones to include a warning about the possibility of tendon rupture."[67]
By August 1996, the FDA had not taken action, and the consumer advocacy group Public Citizen filed a petition with the FDA prompting the agency to act.[68] Two months later, the FDA published an alert in the FDA Medical Bulletin and requested that fluoroquinolone package inserts be amended to include information on this risk.[69]
In 2005, the Illinois Attorney General filed a petition with the FDA seeking black box warnings and "Dear Doctor" letters emphasizing the risk of tendon rupture; the FDA responded that it had not yet been able to reach a decision on the matter.[70] In 2006, Public Citizen, supported by the Illinois Attorney General, renewed its demand of ten years prior for a black box warning.[70][71] In January 2008, Public Citizen filed suit to compel the FDA to respond to their 2006 petition.[72][73] On July 7, the FDA ordered the makers of systemic-use fluoroquinolones to add a boxed warning regarding tendon rupture, and to develop a Medication Guide for patients.[74][75] The package inserts for Cipro (ciprofloxacin), Avelox (moxifloxacin), Proquin XR, Factive (gemifloxacin), Floxin (ofloxacin), Noroxin (norfloxacin) and Levaquin (levofloxacin) were amended on September 8, 2008 to include these new warnings.[76] Bayer, which manufactures Cipro, Avelox and Proquin XR, issued a Dear Healthcare Professional letter on October 22 concerning these changes.[77] Ortho-McNeil, the manufacturers of Levaquin, issued a similar letter in November.[78] through the Health Care Notification Network, a registration-only website that distributes drug alerts to licensed healthcare professionals.
Review of the FDA website indicates that the majority of the generic versions of the fluoroquinolones have not been updated to include this Black Box Warning as of July 2009. And there are numerous reports that this information has not been dessiminated to the pharmacist, the products continue to contain the previous labels that are absent of this warning, and the Medication Guide has not been made available to the pharmicist or physician for distribution.
Social and economic impact
Spontaneous reports of adverse drug reactions associated with cinoxacin, as well as other drugs found within the fluoroquinolone class, are repeatedly made on many Internet forums and medication feedback sites related to prescription drugs worldwide.[79][80] [81][82][83][84][85][86] These adverse drug reactions are easily and likely often misdiagnosed as seizure disorder or regular CNS or psychiatric symptoms and the diagnosis of quinolone toxicity or adverse reaction missed. Research conducted in Italy has shown that quinolones such as cinoxacin are one of the top causes of CNS disturbances in general practice.[87] Another Italian study done in 2008 showed a far greater risk of an adverse reaction occurring with cinoxacin (cinoxacin was related to the highest ROR value) as compared to the other quinolone drugs.[88]
Increased hospitalizations attributed to adverse drug reactions alone account for billions of dollars each year within the US healthcare system. Severe reactions do occur with the fluoroquinolone class and can add significantly to the cost of care. Antibacterial adverse effects account for nearly 25% of all adverse drug reactions amongst hospitalized patients. “Indirect costs as a result of reduced quality of life or loss of productivity are certainly not reflected in the acquisition costs of antimicrobials.”[89]
The adverse drug reaction profile of cinoxacin and other fluoroquinolone drugs has spawned a grass root movement of those so affected to lobby for Black Box Warnings and Dear Doctor Letters as well as the petitioning of the FDA for the removal of some fluoroquinolone drugs from clinical practice.[90][91][92][93][94][95][96][97]
Package insert links
See also
- Fluoroquinolone toxicity
- Fluoroquinolone
- Quinolone
References
- ^ http://health.cd-writer.com/c3/p1561/treatment_for/cinobac_discontinued_in_the_uk.html
- ^ Saunders Comprehensive Veterinary Dictionary 3rd Edition, by D.C. Blood, V.P. Studdert and C.C. Gay, Elsevier
- ^ Z Arztl Fortbild (Jena). 1995 Jun;89(3):279-86 [Antibiotic treatment of complicated urinary tract infections][Article in German] Peters HJ. Urologische Abteilung, St. Elisabeth-Krankenhaus Köln-Hohenlind.
- ^ Pharmaceutical manufacturing encyclopedia, Volume 2 By Marshall Sittig see page 346
- ^ http://www.123jump.com/10K_Reports/WPI/1997/1997.htm
- ^ http://www.getfilings.com/o0001016843-98-000129.html
- ^ http://sec.edgar-online.com/watson-pharmaceuticals-inc/10-k405-annual-report-regulation-s-k-item-405/2000/03/30/section3.aspx
- ^ http://markets.financialcontent.com/edgar?accesscode=101706202000601
- ^ http://download.veritasmedicine.com/PDF/CR002392_CSR.pdf
- ^ Adverse drug reaction monitoring of ciprofloxacin in pediatric practice. sudden death after intravenous ciprofloxacin Indian Pediatr. 1992 Feb;29(2):181-8. Karande SC, Kshirsagar NA. Department of Pharmacology, Seth G.S. Medical College, Parel, Bombay
- ^ a b Dolui SK, Das M, Hazra A (2007). "Ofloxacin-induced reversible arthropathy in a child". Journal of Postgraduate Medicine 53 (2): 144–5. doi:10.4103/0022-3859.32220. PMID 17495385.
- ^ Division of Special Pathogen and Immunologic Drug Products Summary of Clinical Review of Studies Submitted in Response to a Pediatric Written Request
- ^ Chalumeau M, Tonnelier S, D'Athis P, et al. (June 2003). "Fluoroquinolone safety in pediatric patients: a prospective, multicenter, comparative cohort study in France". Pediatrics 111 (6 Pt 1): e714–9. doi:10.1542/peds.111.6.e714. PMID 12777590. http://pediatrics.aappublications.org/cgi/content/full/111/6/e714. Retrieved 2009-06-29.
- ^ 62 Meeting of the Anti-Infective Drugs Advisory Committee
- ^ A Study to Compare the Efficacy and Safety of Levofloxacin in the Treatment of Children With Community-Acquired Pneumonia in the Hospital or Outpatient Setting http://download.veritasmedicine.com/PDF/CR002392_CSR.pdf
- ^ A Study of Levofloxacin in Treating Children With a Rapid and Severe Onset of Infection and Inflammation of the Middle Ear That is Difficult to Treat http://download.veritasmedicine.com/PDF/CR002389_CSR.pdf
- ^ Shepard CW, Soriano-Gabarro M, Zell ER, et al. (October 2002). "Antimicrobial postexposure prophylaxis for anthrax: adverse events and adherence". Emerging Infectious Diseases 8 (10): 1124–32. PMC 2730317. PMID 12396927. http://www.cdc.gov/ncidod/EID/vol8no10/02-0349.htm. Retrieved 2009-06-30.
- ^ 62 Meeting of the Anti-Infective Drugs Advisory Committee http://fqresearch.org/pdf_files/62nd_fda_meeting.pdf
- ^ Drlica K, Zhao X (September 1, 1997). "DNA gyrase, topoisomerase IV, and the 4-quinolones". Microbiol Mol Biol Rev. 61 (3): 377–92. PMC 232616. PMID 9293187. http://mmbr.asm.org/cgi/pmidlookup?view=long&pmid=9293187.
- ^ http://www.drugbank.ca/drugs/DB00827 see mechanism of action heading
- ^ Hussy P, Maass G, Tümmler B, Grosse F, Schomburg U (June 1986). "Effect of 4-quinolones and novobiocin on calf thymus DNA polymerase alpha primase complex, topoisomerases I and II, and growth of mammalian lymphoblasts". Antimicrobial agents and chemotherapy 29 (6): 1073–8. PMC 180502. PMID 3015015. http://aac.asm.org/cgi/reprint/29/6/1073.pdf.
- ^ Hosomi JA. Maeda Y. Oomori T. Irikura and T. Yokota (1988). "Mutagenicity of norfloxacin and AM-833 in bacteria and mammalian cells". Rev. Infect. Dis 10 (Suppl. 1): S148–S149.
- ^ Forsgren A, Bredberg A, Pardee AB, Schlossman SF, Tedder TF (May 1987). "Effects of ciprofloxacin on eucaryotic pyrimidine nucleotide biosynthesis and cell growth". Antimicrobial Agents and Chemotherapy 31 (5): 774–9. PMC 174831. PMID 3606077. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=174831. Retrieved 2009-06-30.
- ^ Gootz TD, Barrett JF, Sutcliffe JA (January 1990). "Inhibitory effects of quinolone antibacterial agents on eucaryotic topoisomerases and related test systems". Antimicrobial Agents and Chemotherapy 34 (1): 8–12. PMC 171510. PMID 2158274. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=171510. Retrieved 2009-06-30.
- ^ Lawrence JW, Darkin-Rattray S, Xie F, Neims AH, Rowe TC (February 1993). "4-Quinolones cause a selective loss of mitochondrial DNA from mouse L1210 leukemia cells". Journal of Cellular Biochemistry 51 (2): 165–74. doi:10.1002/jcb.240510208. PMID 8440750.
- ^ Elsea SH, Osheroff N, Nitiss JL (July 5, 1992). "Cytotoxicity of quinolones toward eukaryotic cells. Identification of topoisomerase II as the primary cellular target for the quinolone CP-115,953 in yeast" (PDF). The Journal of Biological Chemistry 267 (19): 13150–3. PMID 1320012. http://www.jbc.org/cgi/pmidlookup?view=long&pmid=1320012. Retrieved 2009-06-30.
- ^ Suto MJ, Domagala JM, Roland GE, Mailloux GB, Cohen MA (December 1992). "Fluoroquinolones: relationships between structural variations, mammalian cell cytotoxicity, and antimicrobial activity". Journal of Medicinal Chemistry 35 (25): 4745–50. doi:10.1021/jm00103a013. PMID 1469702.
- ^ Enzmann H, Wiemann C, Ahr HJ, Schlüter G (April 1999). "Damage to mitochondrial DNA induced by the quinolone Bay y 3118 in embryonic turkey liver". Mutation research 425 (2): 213–24. doi:10.1016/S0027-5107(99)00044-5. PMID 10216214.
- ^ Kashida Y, Sasaki YF, Ohsawa K, et al. (October 2002). "Mechanistic study on flumequine hepatocarcinogenicity focusing on DNA damage in mice". Toxicological Sciences : an Official Journal of the Society of Toxicology 69 (2): 317–21. doi:10.1093/toxsci/69.2.317. PMID 12377980. http://toxsci.oxfordjournals.org/cgi/content/full/69/2/317. Retrieved 2009-06-30.
- ^ Thomas A, Tocher J, Edwards DI (May 1990). "Electrochemical characteristics of five quinolone drugs and their effect on DNA damage and repair in Escherichia coli". The Journal of Antimicrobial Chemotherapy 25 (5): 733–44. doi:10.1093/jac/25.5.733. PMID 2165050. http://jac.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=2165050. Retrieved 2009-06-30.
- ^ "Fluoroquinolones and Quinolones". The American Academy of Optometry (British Chapter). http://www.academy.org.uk/pharmacy/fluoroq.htm. Retrieved on 29 January 2009
- ^ Yaseen A. Al-Soud; Najim A. Al-Masoudi (2003). "A new class of dihaloquinolones bearing N'-aldehydoglycosylhydrazides, mercapto-1,2,4-triazole, oxadiazoline and a-amino ester precursors: synthesis and antimicrobial activity". J. Braz. Chem. Soc 14 (5). doi:10.1590/S0103-50532003000500014. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-50532003000500014&lng=es&nrm=iso&tlng=es. "Nevertheless, some quinolones cause injury to the chromosome of eukaryotic cells.21,22 These findings prompted us to optimize the substituent at C-3, by...."
- ^ Yaseen A. Al-Soud a and Najim A. Al-Masoudi (2003). "A New Class of Dihaloquinolones Bearing N’-Aldehydoglycosylhydrazides, Mercapto-1,2,4-triazole, Oxadiazoline and α-Amino Ester Precursors: Synthesis and Antimicrobial Activity". J. Braz. Chem. Soc 14 (5): 790–796. http://jbcs.sbq.org.br/jbcs/2003/v14_n5/13-048-02.pdf. "Although the current quinolones are not considered to be potent inhibitors of eucaryotic topoisomerases, some effects on these and other enzymes involved with DNA replication have been observed".
- ^ Sissi C, Palumbo M (November 2003). "The quinolone family: from antibacterial to anticancer agents". Current Medicinal Chemistry 3 (6): 439–50. doi:10.2174/1568011033482279. PMID 14529452. "The present review focuses on the structural modifications responsible for the transformation of an antibacterial into an anticancer agent. Indeed, a distinctive feature of drugs based on the quinolone structure is their remarkable ability to target different type II topoisomerase enzymes. In particular, some congeners of this drug family display high activity not only against bacterial topoisomerases, but also against eukaryotic topoisomerases and are toxic to cultured mammalian cells and in vivo tumor models"
- ^ Owens Rc, Jr; Ambrose, PG (Jul 2005). "Antimicrobial safety: focus on fluoroquinolones.". Clinical Infectious Diseases 41 Suppl 2: S144–57. doi:10.1086/428055. ISSN 1058-4838. PMID 15942881.
- ^ a b Iannini, PB (Jun 2007). "The safety profile of moxifloxacin and other fluoroquinolones in special patient populations.". Current medical research and opinion 23 (6): 1403–13. doi:10.1185/030079907X188099. ISSN 0300-7995. PMID 17559736.
- ^ U S Food and Drug Administration (8 July 2008). "FDA Requests Boxed Warnings on Fluoroquinolone Antimicrobial Drugs" (PDF). USA: FDA. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116919.htm. Retrieved 5 September 2009.
- ^ ^ US Food and Drug Administration (2008). "Fluoroquinolone Antimicrobial Drugs [ciprofloxacin (marketed as Cipro and generic ciprofloxacin), ciprofloxacin extended release (marketed as Cipro XR and Proquin XR), gemifloxacin (marketed as Factive), levofloxacin (marketed as Levaquin), moxifloxacin (marketed as Avelox), norfloxacin (marketed as Noroxin), and ofloxacin (marketed as Floxin and generic ofloxacin)]". USA. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm084316.htm. Retrieved 5 September 2009.
- ^ ^ Renata Albrecht (14 July 2004). "NDA 19-537/S-053, S-054, NDA 20-780/S-017, S-018" (PDF). USA. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2004/19537s053,054,20780s017,018ltr.pdf. Retrieved 5 September 2009. ^ Zehnder, D; Hoigné, R; Neftel, KA; Sieber, R (November 1995).
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2001/20634s15s21s22ltr.pdf
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2004/20635s037,20634s036ltr.pdf
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2000/20635S7,8LTR.PDF
- ^ www.fqresearch.org/pub_med_levaquin/clostridum_difficicile_pub_med_levaquin.doc
- ^ Petitjeans F, Nadaud J, Perez JP, et al. (December 2003). "A case of rhabdomyolysis with fatal outcome after a treatment with levofloxacin". European Journal of Clinical Pharmacology 59 (10): 779–80. doi:10.1007/s00228-003-0688-x. PMID 14576967.
- ^ Acute rhabdomyolysis associated with ofloxacin/levofloxacin therapy. Hsiao SH, Chang CM, Tsao CJ, Lee YY, Hsu MY, Wu TJ. Ann Pharmacother. 2005 Jan;39(1):146-9. Epub 2004 Nov 23. Review. PMID: 15562138
- ^ Korzets A, Gafter U, Dicker D, Herman M, Ori Y (November 2006). "Levofloxacin and rhabdomyolysis in a renal transplant patient". Nephrology Dialysis Transplantation 21 (11): 3304–5. doi:10.1093/ndt/gfl396. PMID 16968728.
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2007/020634s042,020635s045,021721s010ltr.pdf
- ^ ^ http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2004/20634s033,034,20635s033,034ltr.pdf
- ^ ^ a b Iannini, PB (Jun 2007). "The safety profile of moxifloxacin and other fluoroquinolones in special patient populations.". Current medical research and opinion 23 (6): 1403–13. doi:10.1185/030079907X188099. ISSN 0300-7995. PMID 17559736.
- ^ ^ Owens Rc, Jr; Ambrose (Jul 2005). "Antimicrobial safety: focus on fluoroquinolones.". Clinical Infectious Diseases 41 Suppl 2: S144–57. doi:10.1086/428055. ISSN 1058-4838. PMID 15942881.
- ^ Saint F, Gueguen G, Biserte J, Fontaine C, Mazeman E (September 2000). "[Rupture of the patellar ligament one month after treatment with fluoroquinolone]". Revue de chirurgie orthopedique et reparatrice de l'appareil moteur 86 (5): 495–7. PMID 10970974.
- ^ ^ "Public Citizen Warns of Cipro Dangers". USA: Consumer affairs. 30 August 2006. http://www.consumeraffairs.com/news04/2006/08/pubcit_cipro.html. Retrieved 7 September 2009.
- ^ ^ "FDA orders 'black box' label on some antibiotics". http://www.cnn.com/2008/HEALTH/07/08/antibiotics.risk/index.html. Retrieved 2008-07-08.
- ^ A comparison of cinoxacin and nalidixic acid in the treatment of chronic urinary tract infections [Article in German] Briedigkeit H, Schimmelpfennig R, Buder R, Precht K, Dröseler H.
- ^ Anaphylactic reaction to cinoxacin: report of one case associated with inferior acute myocardial infarction. Quercia O, Rafanelli S, Emiliani F, Stefanini GF. Unità Operativa di Medicina Interna Ospedale di Faenza, Ravenna, Italy.
- ^ BMJ. 1988 Dec 3;297(6661):1434-5. Anaphylactic reactions to cinoxacin.Stricker BH, Slagboom G, Demaeseneer R, Slootmaekers V, Thijs I, Olsson S. Netherlands Centre for Monitoring of Adverse Reactions to Drugs, Rijswijk.
- ^ Toxicol Lett. 1983 Jan;15(1):49-56. Effect of cinoxacin on cellular metabolism and p-aminohippurate transport in kidney cortical slices in terms of its nephrotoxic action. Gemba M, Komamura T, Matsushima Y, Itoh T, Miyata K, Nakamura M.
- ^ An unusual form of crystal-forming chronic interstitial nephritis following long-term exposure to tosufloxacin tosilate. Okada H, Watanabe Y, Kotaki S, Ikeda N, Takane H, Kanno Y, Sugahara S, Ban S, Nagata M, Suzuki H. Department of Nephrology, Saitama Medical College, Saitama, Japan.
- ^ Urology. 1984 Jan;23(1):101-7. Review of adverse reactions associated with cinoxacin and other drugs used to treat urinary tract infections. Burt RA.
- ^ Dermatologica. 1990;181(2):98-103. Demonstration of quinolone phototoxicity in vitro. Przybilla B, Georgii A, Bergner T, Ring J.
- ^ Drug Intell Clin Pharm. 1982 Dec;16(12):916-21.Cinoxacin (Cinobac, Eli Lilly & Co.). Guay DR.
- ^ a b http://www.drugbank.ca/drugs/DB00827
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/label/2002/18067s29lbl.pdf
- ^ Antimicrob Agents Chemother. 1979 Feb;15(2):165-70. Pharmacology of cinoxacin in humans.Black HR, Israel KS, Wolen RL, Brier GL, Obermeyer BD, Ziege EA, Wolny JD.
- ^ Bailey RR, Natale R, Linton AL (October 1972). "Nalidixic acid arthralgia". Can Med Assoc J 107 (7): 604 passim. PMC 1940945. PMID 4541768. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1940945.
- ^ Bailey RR, Kirk JA, Peddie BA (July 1983). "Norfloxacin-induced rheumatic disease". N Z Med J 96 (736): 590. PMID 6223241.
- ^ Szarfman A, Chen M, Blum MD (January 1995). "More on fluoroquinolone antibiotics and tendon rupture" (letter). N Engl J Med 332 (3): 193. doi:10.1056/NEJM199501193320319. PMID 7800023.
- ^ "Petition to Require a Warning on All Fluoroquinolone Antibiotics (HRG Publication #1399)". Public Citizen. August 1, 1996. http://www.citizen.org/publications/release.cfm?ID=6595. Retrieved on December 27, 2008.
- ^ "Reports of adverse events with fluoroquinolones". FDA Medical Bulletin 26 (3). October 1996. http://www.fda.gov/medbull/oct96/adverse.html.[dead link] Retrieved on December 27, 2008. alternate link: http://www.fqresearch.org/text_documents/FDA_Medical_Bulletin_1996.doc
- ^ a b "Madigan, Public Citizen, petition FDA for "black box" warning regarding potential adverse effects of certain popular antibiotics" (Press release). Office of the Illinois Attorney General. August 29, 2006. http://www.illinoisattorneygeneral.gov/pressroom/2006_08/20060829.html. Retrieved 2008-12-27. Full text of the 2005 petition and FDA response available from the Fluoroquinolone Toxicity Research Foundation, a U.S. consumer advocacy group.
- ^ "Public Citizen Petitions the FDA to Include a Black Box Warning on Fluoroquinolone Antibiotics (HRG Publication #1781)". Public Citizen. August 29, 2006. http://www.citizen.org/publications/release.cfm?ID=7453. Retrieved 2008-12-27.
- ^ "Public Citizen v. Food and Drug Administration (FDA) (Fluoroquinolone)". Public Citizen. January 3, 2008. http://www.citizen.org/litigation/forms/cases/CaseDetails.cfm?cID=444. Retrieved 2008-12-27.
- ^ Ravn, Karen (August 18, 2008). "Behind the FDA’s ‘black box’ warnings". Los Angeles Times. http://articles.latimes.com/2008/aug/18/health/he-closer18. Retrieved 2008-12-27.
- ^ "FDA Requests Boxed Warnings on Fluoroquinolone Antimicrobial Drugs" (Press release). U.S. Food and Drug Administration. 2008-07-08. http://www.fda.gov/bbs/topics/NEWS/2008/NEW01858.html. Retrieved 2008-10-11.
- ^ http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116919.htm
- ^ The complete labeling history of each drug is available from Drugs@FDA. Medication Guides are available from the FDA's MedWatch system.
- ^ MacCarthy, Paul (October 22, 2008). "Important Change in the Avelox (moxifloxacin hydrochloride) and Cipro (ciprofloxacin) Complete Prescribing Information – Addition of Boxed Warning and Medication Guide Regarding Tendinitis and Tendon Rupture" (PDF). Bayer HealthCare Pharmaceuticals. http://www.cipro.com/html/pdf/dhpl.pdf. Retrieved 2008-12-27.
- ^ Rosenthal, Norman (November 2008). "Important Change in the LEVAQUIN (Ievofloxacin) Complete Prescribing Information -Addition of Boxed Warning and Medication Guide Regarding Tendinitis and Tendon Rupture" (PDF). Ortho-McNeil Janssen Scientific Affairs, LLC. http://www.fqresearch.org/pdf_files/Levaquin_11_2008_ortho_mcneil_dear_dr_letter.pdf. Retrieved 2008-12-27.
- ^ http://www.rxlist.com
- ^ http://groups.yahoo.com/group/fqtoxicity
- ^ http://www.favc.info
- ^ www.medicationsense.com
- ^ http://www.citizen.org
- ^ www.FluoroquinoloneAntibiotic.com
- ^ http://www.askapatient.com/
- ^ http://www.aaavam.com/ see also http://www.aaavam.com/index_01.html
- ^ http://www.em-news.com/pt/re/emmednews/pdfhandler.00132981-200810000-00023.pdf;jsessionid=JNJGnJrSnxkP9r3mcySnGQJGZ5qDNRJv18N8bJvkhJ41877mWQM2!1321082991!181195629!8091!-1
- ^ Pharmacol Res. 2008 Sep-Oct;58(3-4):202-7. Epub 2008 Jul 23. Links Allergic reactions to oral drugs: A case/non-case study from an Italian spontaneous reporting database (GIF).Salvo F, Polimeni G, Cutroneo PM, Leone R, Confortic A, Moretti U, Motola D, Tuccori M, Caputi AP. Department of Clinical and Experimental Medicine and Pharmacology, School of Medicine, University of Messina, Messina, Italy. fsalvo@unime.it
- ^ Beringer PM, Wong-Beringer A, Rho JP (January 1998). "Economic aspects of antibacterial adverse effects". PharmacoEconomics 13 (1 Pt 1): 35–49. doi:10.2165/00019053-199813010-00004. PMID 10175984.
- ^ In The United States District Court For The District Of Columbia Public Citizen, Inc. VS. Food And Drug Administration January 3, 2008
- ^ Office Of The Attorney General State Of Illinois Lisa Madigan Citizen Petition to Include a Black Box Warning on Fluoroquinolone Antibiotics May 18, 2005
- ^ Public Citizen’s Petition to Include a Black Box Warning on Fluoroquinolone Antibiotics (HRG Publication #1781) August 29, 2006
- ^ Public Citizen's Petition to Require a Warning on All Fluoroquinolone Antibiotics (HRG Publication #1399) August 1, 1996
- ^ Public Citizen's Petition to Ban the Antibiotic Gatifloxacin (Tequin) (HRG Publication #1768)
- ^ Public Citizen's Petition to immediately ban the antibiotic Trovafloxacin (Trovan). (HRG Publication #1485) Date: June 3, 1999
- ^ Public Citizen's Petition to immediately stop the distribution of dangerous, misleading prescription drug information to the public. HRG Publication #1442 Date: June 9, 1998
- ^ June 2004, A petition To the United States Congress to immediately take action to protect consumers from the reckless and negligent abuses of the FDA and the following Pharmaceutical Companies: Bayer, Ortho-McNeill, Pfizer, Merck, Bristol-Myers Squibb, Sanofi Winthrop, Bertek Pharmaceuticals – Rhone-Poulenc Rorer and Barr. These companies manufacture and distribute fluoroquinolone antibiotics in the United States in a manner that fails to warn of serious adverse event risks, and downplays and fails to warn physicians of the serious risks associated with fluoroquinolone therapy.
External links
- Cinoxacin at the Open Directory Project
Antibacterials: nucleic acid inhibitors (J01E, J01M) Antifolates
(inhibits
purine metabolism,
thereby inhibiting
DNA and RNA synthesis)Sulfonamides
(DHPS inhibitor)Other/ungroupedCombinationsTopoisomerase
inhibitors/
quinolones/
(inhibits
DNA replication)1st g.Cinoxacin‡ • Flumequine • Nalidixic acid • Oxolinic acid • Pipemidic acid • Piromidic acid • Rosoxacin2nd g.Ciprofloxacin# • Enoxacin‡ • Fleroxacin‡ • Lomefloxacin • Nadifloxacin • Ofloxacin • Norfloxacin • Pefloxacin • Rufloxacin3rd g.4th g.Besifloxacin • Clinafloxacin† • Garenoxacin • Gemifloxacin • Moxifloxacin • Gatifloxacin‡ • Sitafloxacin • Trovafloxacin‡/Alatrofloxacin‡ • PrulifloxacinVet.Related (DG)Anaerobic DNA
inhibitorsNitrofuran derivativesRNA synthesis Categories:- Antimicrobials
- Cinnolines
- Benzodioxoles
Wikimedia Foundation. 2010.
