- Peripheral neuropathy
-
"Neuropathy" redirects here. For other uses, see Neuropathy (disambiguation).Not to be confused with Nephropathy.
Peripheral neuropathy Classification and external resources 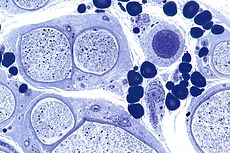
Micrograph showing a vasculitic peripheral neuropathy. Plastic embedded. Toluidine blue stain.ICD-10 G64, G90.0 ICD-9 356.0, 356.8 DiseasesDB 9850 MeSH D010523 Peripheral neuropathy is the term for damage to nerves of the peripheral nervous system,[1] which may be caused either by diseases of or trauma to the nerve or the side-effects of systemic illness.
The four cardinal patterns of peripheral neuropathy are polyneuropathy, mononeuropathy, mononeuritis multiplex and autonomic neuropathy. The most common form is (symmetrical) peripheral polyneuropathy, which mainly affects the feet and legs. The form of neuropathy may be further broken down by cause, or the size of predominant fiber involvement, i.e., large fiber or small fiber peripheral neuropathy. Frequently the cause of a neuropathy cannot be identified and it is designated idiopathic.
Neuropathy may be associated with varying combinations of weakness, autonomic changes, and sensory changes. Loss of muscle bulk or fasciculations, a particular fine twitching of muscle, may be seen. Sensory symptoms encompass loss of sensation and "positive" phenomena including pain. Symptoms depend on the type of nerves affected (motor, sensory, or autonomic) and where the nerves are located in the body. One or more types of nerves may be affected. Common symptoms associated with damage to the motor nerve are muscle weakness, cramps, and spasms. Loss of balance and coordination may also occur. Damage to the sensory nerve can produce tingling, numbness, and pain. Pain associated with this nerve is described in various ways such as the following: sensation of wearing an invisible "glove" or "sock", burning, freezing, or electric-like, extreme sensitivity to touch. The autonomic nerve damage causes problems with involuntary functions leading to symptoms such as abnormal blood pressure and heart rate, reduced ability to perspire, constipation, bladder dysfunction (e.g., incontinence), and sexual dysfunction.[2]
Contents
Classification
Peripheral neuropathy may be classified according to the number of nerves affected or the type of nerve cell affected (motor, sensory, autonomic), or the process affecting the nerves (e.g. inflammation in neuritis).
Mononeuropathy
See also: Compression neuropathyMononeuropathy is a type of neuropathy that only affects a single nerve.[3] It is diagnostically useful to distinguish them from polyneuropathies, because the limitation in scope makes it more likely that the cause is a localized trauma or infection.
The most common cause of mononeuropathy is by physical compression of the nerve, known as compression neuropathy. Carpal tunnel syndrome is one example of this. The "pins-and-needles" sensation of one's "foot falling asleep" (paresthesia) is caused by a compression mononeuropathy, albeit a temporary one which can be resolved merely by moving around and adjusting to a more appropriate position. Direct injury to a nerve, interruption of its blood supply (ischemia), or inflammation can also cause mononeuropathy.
Mononeuritis multiplex
Mononeuritis multiplex is simultaneous or sequential involvement of individual noncontiguous nerve trunks, either partially or completely, evolving over days to years and typically presents with acute or subacute loss of sensory and motor function of individual peripheral nerves. The pattern of involvement is asymmetric, however, as the disease progresses, deficit(s) becomes more confluent and symmetrical, making it difficult to differentiate from polyneuropathy. Therefore, attention to the pattern of early symptoms is important.
Mononeuritis multiplex may also cause pain, which is characterized as deep, aching pain that is worse at night, is frequently in the lower back, hip, or leg. In people with diabetes mellitus, mononeuritis multiplex is typically encountered as acute, unilateral, severe thigh pain followed by anterior muscle weakness and loss of knee reflex.
Electrodiagnostic studies will show multifocal sensory motor axonal neuropathy.
It is caused by, or associated with, several medical conditions:
- diabetes mellitus
- vasculitides: polyarteritis nodosa, Wegener granulomatosis, and Churg-Strauss syndrome
- immune-mediated diseases like rheumatoid arthritis, lupus erythematosus (SLE), and sarcoidosis
- infections: leprosy, lyme disease, HIV
- amyloidosis
- cryoglobulinemia
- chemical agents, including trichloroethylene and dapsone
- rarely, the sting of certain jellyfish, such as the sea nettle
Polyneuropathy
Main article: PolyneuropathyPolyneuropathy is a pattern of nerve damage which is quite different from mononeuropathy. The term "peripheral neuropathy" is sometimes used loosely to refer to polyneuropathy. In a polyneuropathy, many nerve cells in different parts of the body are affected, without regard to the nerve through which they pass. Not all nerve cells are affected in any particular case. In distal axonopathy, one common pattern, the cell bodies of neurons remain intact, but the axons are affected in proportion to their length. Diabetic neuropathy is the most common cause of this pattern. In demyelinating polyneuropathies, the myelin sheath around axons is damaged, which affects the ability of the axons to conduct electrical impulses. The third and least common pattern affects the cell bodies of neurones directly. This usually picks out either the motor neurones (known as motor neurone disease) or the sensory neurones (known as sensory neuronopathy or dorsal root ganglionopathy).
The effect of this is to cause symptoms in more than one part of the body, often on left and right sides symmetrically. As for any neuropathy, the chief symptoms include weakness or clumsiness of movement (motor); unusual or unpleasant sensations such as tingling or burning; reduction in the ability to feel texture, temperature, etc.; and impaired balance when standing or walking (sensory). In many polyneuropathies, these symptoms occur first and most severely in the feet. Autonomic symptoms may also occur, such as dizziness on standing up, erectile dysfunction and difficulty controlling urination.
Polyneuropathies are usually caused by processes that affect the body as a whole. Diabetes and impaired glucose tolerance are the most common causes. Other causes relate to the particular type of polyneuropathy, and there are many different causes of each type, including inflammatory diseases such as lyme disease, vitamin deficiencies, blood disorders, and toxins (including alcohol and certain prescribed drugs). Most types of polyneuropathy progress fairly slowly, over months or years, but rapidly progressive polyneuropathy also occurs. It is important to recognize that glucose levels in the blood can spike to nerve-damaging levels after eating even though fasting blood sugar levels and average blood glucose levels can still remain below normal levels (currently typically considered below 100 for fasting blood plasma and 6.0 for HGBA1c, the test commonly used to measure average blood glucose levels over an extended period). Studies have shown that many of the cases of peripheral small fiber neuropathy with typical symptoms of tingling, pain and loss of sensation in the feet and hands are due to glucose intolerance before a diagnosis of diabetes or pre-diabetes. Such damage is often reversible, particularly in the early stages, with diet, exercise and weight loss.17
The treatment of polyneuropathies is aimed firstly at eliminating or controlling the cause, secondly at maintaining muscle strength and physical function, and thirdly at controlling symptoms such as neuropathic pain.
Autonomic neuropathy
Autonomic neuropathy is a form of polyneuropathy which affects the non-voluntary, non-sensory nervous system (i.e., the autonomic nervous system) affecting mostly the internal organs such as the bladder muscles, the cardiovascular system, the digestive tract, and the genital organs. These nerves are not under a person's conscious control and function automatically. Autonomic nerve fibers form large collections in the thorax, abdomen and pelvis outside spinal cord, however they have connections with the spinal cord and ultimately the brain. Most commonly autonomic neuropathy is seen in persons with long-standing diabetes mellitus type 1 and 2. In most but not all cases, autonomic neuropathy occurs alongside other forms of neuropathy, such as sensory neuropathy.
Autonomic neuropathy is one cause of malfunction of the autonomic nervous system, but not the only one; some conditions affecting the brain or spinal cord can also cause autonomic dysfunction, such as multiple system atrophy, and therefore cause similar symptoms to autonomic neuropathy.
The signs and symptoms of autonomic neuropathy include the following:
- urinary bladder conditions: bladder incontinence or urine retention
- gastrointestinal tract: dysphagia, abdominal pain, nausea, vomiting, malabsorption, fecal incontinence, gastroparesis, diarrhea, constipation
- cardiovascular system: disturbances of heart rate (tachycardia, bradycardia), orthostatic hypotension, inadequate increase of heart rate on exertion
- other: hypoglycemia unawareness, genital impotence, sweat disturbances
Neuritis
Neuritis is a general term for inflammation of a nerve[4] or the general inflammation of the peripheral nervous system. Symptoms depend on the nerves involved, but may include pain, paresthesia (pins & needles), paresis (weakness), hypoesthesia (numbness), anesthesia, paralysis, wasting, and disappearance of the reflexes. Causes include:
- Physical injury
One common cause of neuritis and subsequent inflammation of the nerves to the toes is the wearing of high-heeled shoes or ill-fitting shoes that bind the toes painfully. This can cause temporary numbness and pain in the affected toes for several days.
- Chemical injury
- Radiation
- Underlying conditions causing localized neuritis (affecting a single nerve):
- Diphtheria
- Localized injury
- Diabetes
- Underlying conditions causing polyneuritis (affecting multiple nerves):
- Beriberi
- Vitamin B12 deficiency
- Vitamin B6 excess[5]
- Metabolic diseases
- Diabetes
- Herpes zoster
- Hypothyroidism
- Porphyria
- Infections, bacterial and/or viral
- Autoimmune disease, especially Multiple Sclerosis
- Cancer
- Alcoholism
- Wartenbergs migratory sensory neuropathy
Types of neuritis include:
- Polyneuritis or Multiple neuritis (not to be confused with multiple sclerosis)
- Brachial neuritis
- Optic neuritis
- Vestibular neuritis
- Cranial neuritis, often representing as Bell's Palsy
- Arsenic neuritis
Signs and symptoms
Those with diseases or dysfunctions of their peripheral nerves can present with problems in any of the normal peripheral nerve functions.
In terms of sensory function, there are commonly loss of function (negative) symptoms, which include numbness, tremor, and gait abnormality.
Gain of function (positive) symptoms include tingling, pain, itching, crawling, and pins and needles. Pain can become intense enough to require use of opioid (narcotic) drugs (i.e., morphine, oxycodone).
Skin can become so hypersensitive that patients are prohibited from having anything touch certain parts of their body, especially the feet. People with this degree of sensitivity cannot have a bedsheet touch their feet or wear socks or shoes, and eventually become housebound.
Motor symptoms include loss of function (negative) symptoms of weakness, tiredness, heaviness, and gait abnormalities; and gain of function (positive) symptoms of cramps, tremor, and muscle twitch (fasciculations).
There is also pain in the muscles (myalgia), cramps, etc., and there may also be autonomic dysfunction.
During physical examination, specifically a neurological examination, those with generalized peripheral neuropathies most commonly have distal sensory or motor and sensory loss, though those with a pathology (problem) of the peripheral nerves may be perfectly normal; may show proximal weakness, as in some inflammatory neuropathies like Guillain–Barré syndrome; or may show focal sensory disturbance or weakness, such as in mononeuropathies. Ankle jerk reflex is classically absent in peripheral neuropathy.
Causes
The causes are broadly grouped as follows:
- Genetic diseases: Friedreich's ataxia, Charcot-Marie-Tooth syndrome [6]
- Metabolic/Endocrine: diabetes mellitus,[7] chronic renal failure, porphyria, amyloidosis, liver failure, hypothyroidism
- Toxic causes: Drugs (vincristine, metronidazole, phenytoin, nitrofurantoin, isoniazid, ethyl alcohol), organic metals, heavy metals, excess intake of vitamin B6 (pyridoxine)
- Fluoroquinolone toxicity: Irreversible neuropathy is a serious adverse reaction of fluoroquinolone drugs [8]
- Inflammatory diseases: Guillain-Barré syndrome, systemic lupus erythematosis, leprosy, Sjögren's syndrome, Lyme Disease, sarcoidosis,[9]
- Vitamin deficiency states: Vitamin B12 (cyanocobalamin), vitamin A, vitamin E, vitamin B1 (thiamin)
- Physical trauma: compression, pinching, cutting, projectile injuries (i.e. gunshot wound), strokes including prolonged occlusion of blood flow, electric discharge, including lightning strikes
- Others: shingles, malignant disease, HIV,[10] radiation, chemotherapy[11]
Many of the diseases of the peripheral nervous system may present similarly to muscle problems (myopathies), and so it is important to develop approaches for assessing sensory and motor disturbances in patients so that a physician may make an accurate diagnosis.
Treatment
Many treatment strategies for peripheral neuropathy are symptomatic. Some current research in animal models has shown that neurotrophin-3 can oppose the demyelination present in some peripheral neuropathies.[12]
A range of drugs that act on the central nervous system such as drugs originally intended as antidepressants and antiepileptic drugs have been found to be useful in managing neuropathic pain. Commonly used treatments include using a tricyclic antidepressant (such as amitriptyline) and antiepileptic therapies such as gabapentin or sodium valproate. These have the advantage that besides being effective in many cases they are relatively low cost.
A great deal of research has been done between 2005 and 2010 which indicates that synthetic cannabinoids and inhaled cannabis are effective treatments for a range of neuropathic disorders.[13] Research has demonstrated that the synthetic oral cannabinoid Nabilone is an effective adjunct treatment option for neuropathic conditions, especially for people who are resistant, intolerant, or allergic to common medications.[14] Orally, opiate derivatives were found to be more effective than cannabis for most people.[15] Smoked cannabis has been found to provide relief from HIV-associated sensory neuropathy.[16] Smoked cannabis was also found to relieve neuropathy associated with CRPS type I, spinal cord injury, peripheral neuropathy, and nerve injury.[17]
Pregabalin (
 /prɨˈɡæbəlɨn/) is an anticonvulsant drug used for neuropathic pain. It has also been found effective for generalized anxiety disorder. It was designed as a more potent successor to gabapentin but is significantly more expensive, especially now that the patent on gabapentin has expired and gabapentin is available as a generic drug. Pregabalin is marketed by Pfizer under the trade name Lyrica.
/prɨˈɡæbəlɨn/) is an anticonvulsant drug used for neuropathic pain. It has also been found effective for generalized anxiety disorder. It was designed as a more potent successor to gabapentin but is significantly more expensive, especially now that the patent on gabapentin has expired and gabapentin is available as a generic drug. Pregabalin is marketed by Pfizer under the trade name Lyrica.Duloxetine, a serotonin-norepinephrine reuptake inhibitor, is also being used to reduce neuropathic pain.
TENS (Transcutaneous Electrical Nerve Stimulation) therapy may be effective and safe in the treatment of diabetic peripheral neuropathy. A recent review of three trials involving 78 patients found some improvement in pain scores after 4 and 6 but not 12 weeks of treatment, and an overall improvement in neuropathic symptoms at 12 weeks.[18] A second review of four trials found significant improvement in pain and overall symptoms, with 38% of patients in one trial becoming asymptomatic. The treatment remains effective even after prolonged use, but symptoms return to baseline within a month of treatment cessation.[19]
References
- ^ "Peripheral Neuropathy Fact Sheet: National Institute of Neurological Disorders and Stroke (NINDS)". http://www.ninds.nih.gov/disorders/peripheralneuropathy/detail_peripheralneuropathy.htm. Retrieved 2008-11-30.
- ^ http://www.neurologychannel.com/neuropathy/symptoms.shtml
- ^ "Dorlands Medical Dictionary:mononeuropathy". http://www.mercksource.com/pp/us/cns/cns_hl_dorlands_split.jsp?pg=/ppdocs/us/common/dorlands/dorland/five/000067367.htm.
- ^ "neuritis" at Dorland's Medical Dictionary
- ^ http://emedicine.medscape.com/article/819426-overview
- ^ Gabriel JM, Erne B, Pareyson D, Sghirlanzoni A, Taroni F, Steck AJ (1997). "Gene dosage effects in hereditary peripheral neuropathy. Expression of peripheral myelin protein 22 in Charcot-Marie-Tooth disease type 1A and hereditary neuropathy with liability to pressure palsies nerve biopsies". Neurology 49 (6): 1635–40. PMID 9409359.
- ^ Kiziltan ME, Akalin MA, Sahin R, Uluduz D (2007). "Peripheral neuropathy in patients with diabetes mellitus presenting as Bell's palsy". Neuroscience Letters 427 (3): 138. doi:10.1016/j.neulet.2007.09.029. PMID 17933462.
- ^ Cohen JS (December 2001). "Peripheral Neuropathy Associated with Fluoroquinolones" (PDF). Ann Pharmacother 35 (12): 1540–7. doi:10.1345/aph.1Z429. PMID 11793615. http://fqvictims.org/fqvictims/News/neuropathy/Neuropathy.pdf.
- ^ Heck AW, Phillips LH 2nd (1989). "Sarcoidosis and the nervous system". Neurol Clin 7 (3): 641–54. PMID 2671639.
- ^ Gonzalez-Duarte A, Cikurel K, Simpson DM (2007). "Managing HIV peripheral neuropathy". Current HIV/AIDS reports 4 (3): 114–8. doi:10.1007/s11904-007-0017-6. PMID 17883996.
- ^ Wilkes G (2007). "Peripheral neuropathy related to chemotherapy". Seminars in oncology nursing 23 (3): 162–73. doi:10.1016/j.soncn.2007.05.001. PMID 17693343.
- ^ Liu N, Varma S, Tsao D, Shooter EM, Tolwani RJ (2007). "Depleting endogenous neurotrophin-3 enhances myelin formation in the Trembler-J mouse, a model of a peripheral neuropathy". J. Neurosci. Res. 85 (13): 2863–9. doi:10.1002/jnr.21388. PMID 17628499.
- ^ http://www.cannabis-med.org/data/pdf/en_2010_01_special.pdf
- ^ Skrabek RQ, Galimova L, Ethans K, Perry D (2008). "Nabilone for the treatment of pain in fibromyalgia". J. Pain 9 (2): 164–73. doi:10.1016/j.jpain.2007.09.002. PMID 17974490.
- ^ Frank B, Serpell MG, Hughes J, Matthews JN, Kapur D (2008). "Comparison of analgesic effects and patient toleration of nabilone and dihydrocodeine for chronic neuropathic pain: randomized, crossover, double blind study". BMJ 336 (7637): 119–201.
- ^ Abrams DI, Jay CA, Shade SB, Vizozo H, Reda H, Press S, Kelly ME, Rowbotham Mc, Petersen KL (2007). "Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trail". J. Neurology 68 (7): 515–21. doi:10.1212/01.wnl.0000253187.66183.9c. PMID 17296917.
- ^ Wilsey B, Marcotte T, Tsodikov A, Millman J, Bentley H, Gouaux B, Fishman S (2008). "A randomized, placebo-controlled, crossover trail of cannabis cigarettes in neuropathic pain". J. Pain 9 (6): 506–21. doi:10.1016/j.jpain.2007.12.010. PMID 18403272.
- ^ Jin DM, Xu Y, Geng DF, Yan TB (July 2010). "Effect of transcutaneous electrical nerve stimulation on symptomatic diabetic peripheral neuropathy: a meta-analysis of randomized controlled trials". Diabetes Res. Clin. Pract. 89 (1): 10–5. doi:10.1016/j.diabres.2010.03.021. PMID 20510476.
- ^ Pieber K, Herceg M, Paternostro-Sluga T (April 2010). "Electrotherapy for the treatment of painful diabetic peripheral neuropathy: a review". J Rehabil Med 42 (4): 289–95. doi:10.2340/16501977-0554. PMID 20461329.
Further reading
- Latov, Norman (2007). Peripheral Neuropathy: When the Numbness, Weakness, and Pain Won't Stop. New York: American Academy of Neurology Press Demos Medical. ISBN 193260359X.
External links
- The Foundation for Peripheral Neuropathy
- The Canadian Neuropathy Association
- National Diabetes Information Clearinghouse at National Institute of Diabetes and Digestive and Kidney Diseases
- The Neuropathy Association
- Reference centre for rare neuropathies
Pathology: Medical conditions and ICD code (A/B, 001–139) Infectious disease/Infection: Bacterial disease (G+, G-) · Virus disease · Parasitic disease (Protozoan infection, Helminthiasis, Ectoparasitic infestation) · Mycosis · Zoonosis(C/D,
140–239 &
279–289)Cancer (C00–D48, 140–239)Myeloid hematologic (D50–D77, 280–289)(E, 240–278) (F, 290–319) (G, 320–359) (H, 360–389) (I, 390–459) (J, 460–519) (K, 520–579) Stomatognathic disease (Tooth disease) · Digestive disease (Esophageal, Stomach, Enteropathy, Liver, Pancreatic)(L, 680–709) (M, 710–739) (N, 580–629) Urologic disease (Nephropathy, Urinary bladder disease) · Male genital disease · Breast disease · Female genital disease(O, 630–679) (P, 760–779) (Q, 740–759) (R, 780–799) (S/T, 800–999) Nervous system pathology, PNS, somatic (G50–G64, 350–357) Nerve, nerve root, plexus V (Trigeminal neuralgia, Anesthesia dolorosa) · VII (Facial nerve paralysis, Bell's palsy, Melkersson–Rosenthal syndrome, Parry–Romberg syndrome, Central seven) · XI (Accessory nerve disorder)Lower limbGeneralPolyneuropathies/Polyradiculoneuropathy OtherAutonomic diseases, Dysautonomia, autonomic- neuropathy (G90, 337) HSAN Orthostatic intolerance Other Drugs used for the treatment of fibromyalgia and neuropathic pain Antidepressants OthersAnticonvulsants Carbamazepine • Divalproex sodium • Gabapentin • Lacosamide • Lamotrigine • Oxcarbazepine • Phenytoin • Pregabalin • Sodium valproate • Topiramate • Valproic acidMiscellaneous CannabinoidsOthersCategories:- Peripheral nervous system disorders
Wikimedia Foundation. 2010.
