- Trauma (medicine)
-
For other uses, see Trauma.
Trauma Classification and external resources 
Hospital corpsmen and medical officers of the United States Navy assess an intubated patient with a gunshot woundICD-10 T79 ICD-9 900-957 DiseasesDB 28858 MedlinePlus 000024 eMedicine trauma MeSH D014947 Trauma refers to "a body wound or shock produced by sudden physical injury, as from violence or accident."[1] It can also be described as "a physical wound or injury, such as a fracture or blow."[2] Major trauma (defined by an Injury Severity Score of greater than 15)[3] can result in secondary complications such as circulatory shock, respiratory failure and death. Resuscitation of a trauma patient often involves multiple management procedures. Trauma is the sixth leading cause of death worldwide, accounting for 10% of all mortality, and is a serious public health problem with significant social and economic costs.
Contents
Classification
Trauma can be classified by the affected area of the body[4] (percentages of total incidence[5]):
- Polytrauma (40%)
- Head injury (30%)
- Chest trauma (20%)
- Abdominal trauma (10%)
- Extremity trauma (2%)
- Facial trauma
- Spinal cord injury
- Genitourinary system trauma
- Pelvic trauma
- Soft tissue injury
Trauma may also be classified by the affected demographic group (for example, trauma in the pregnant, pediatric, or geriatric patient).[4] They may also be classified by the type of force applied to the body, such as blunt trauma versus penetrating trauma.
Causes and risk factors
Blunt trauma is the leading cause of traumatic death in the United States.[6] Most cases of blunt trauma are caused by motor vehicle accidents.[6] Falls, a subset of blunt trauma, are the second most common cause of traumatic death.[7] In most cases a fall of greater than three times the victim's height is defined as a severe fall.[7] Penetrating trauma is caused when a foreign object such as a bullet or a knife enters a tissue of the body, creating an open wound. In the United States most deaths caused by penetrating trauma occur in urban areas and 80% of these deaths are caused by firearms.[8] Blast injury is a complex cause of polytrauma. It commonly includes both blunt and penetrating trauma and may also be accompanied by a burn injury.
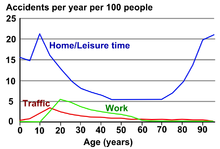
By identifying risk factors present within a community and creating solutions to decrease the incidence of injury, trauma referral systems can help to enhance the overall health of its population.[9] Ingestion of alcohol and illicit drugs are risk factors for trauma, particularly traffic collisions, violence and abuse.[5] Long-acting benzodiazepines increase the risk of trauma in elderly people.[5]
Diagnosis
Radiograph of a close-range shotgun blast injury to the knee. Birdshot pellets are visible within and around the shattered patella, distal femur and proximal tibia.
Physical examination
The purpose of the primary survey is to identify life-threatening problems. Upon completion of the primary survey, the secondary survey is begun. This may occur during transport or upon arrival at the hospital. The secondary survey consists of a systematic assessment of the abdominal, pelvic and thoracic area, complete inspection of the body surface to find all injuries, and a neurological examination. The purpose of the secondary survey is to identify all injuries so that they may be treated. A missed injury is one which is not found during the initial assessment (for example, as a patient is brought into a hospital's emergency department), but rather manifests itself at a later point in time.[10]
Imaging
X-rays of the chest and pelvis are commonly performed in major trauma.[5] Focused assessment with sonography for trauma (FAST), can also be used. Computed tomography (CT) scans are the gold standard in imaging in major trauma.[11] They however may only be performed in people with a relatively stable blood pressure, heart rate, and sufficient oxygenation.[5] Full-body CT scans known as pan-scans improve survival in those who have suffered major trauma.[12] The scans are done using intravenous radiocontrast but not oral contrast.[13] There are concerns of radiation exposure and concerns regarding negative effects of contrast on the kidneys. However some centers routinely do CTs with contrast before verifying renal function even in the elderly and have not found negative side effects with respect to the kidneys.[11] With modern imaging technology a complete scan can be performed in less than 10 minutes.[5] In the emergency department in the United States CT or MRI imaging is done in 15% of people who present with injuries as of 2007 (up from 6% in 1998).[14] In those who poor blood pressure or a fast heart rate from a presumed abdominal bleeding delaying surgery for abdominal CT imaging may worsen outcomes.[15]
Surgical techniques
Surgical techniques, such as diagnostic peritoneal lavage, placement of a thoracostomy tube, or pericardiocentesis are often used in cases of severe blunt trauma to the chest or abdomen, especially in the setting of deteriorating hemodynamic stability. In those who are hypotensive due to presumed internal abdominal bleeding transfer to the operating room for a laporotomy is the preferred method of determining a definitive diagnosis.[5]
Management
 A Navy corpsmen listens for the correct tube placement on an intubated trauma victim during a search and rescue (SAR) exercise
A Navy corpsmen listens for the correct tube placement on an intubated trauma victim during a search and rescue (SAR) exercise
People who have severe trauma frequently require specialized physicians and equipment. Designated trauma centers have improved outcomes compared to non designated centers.[5] The transfer directly to a trauma center is associated with improved outcomes compared to transfer to a non trauma center.[16]
Stabilization and transportation
Further information: Trauma centerIn the prehospital setting the use of stabilization techniques improve the chances of a person surviving the transport to the nearest trauma-equipped hospital. After ensuring their own safety and taking isolation precautions, a primary survey is performed, consisting of checking and treating airway, breathing, and circulation (called the ABC's) then an assessment of the level of consciousness.[10] To prevent further injury, unnecessary movement of the spine is minimized by securing the neck with a cervical collar, and the back with a long spine board with head supports, or other medical transport device such as a Kendrick extrication device, before moving the person.[17] Unless the person is in imminent danger of death, first responders will typically "load and go," transporting immediately to the nearest appropriate facility.[10] Helicopter EMS transport reduces mortality compared to ground based transport in adult trauma patients.[18]
Rapid transportation of those who are severely injured is associated with improved outcomes.[5] In the prehospital environment, the availability of advanced life support does not improve outcomes for major trauma, when compared with basic life support.[19][20] The evidence is also inconclusive with respect to support for prehospital intravenous fluid resuscitation and some evidence has found it may be harmful.[21]
People who have suffered trauma may require specialized care, including surgery and blood transfusion. Outcomes are better if this occurs as quickly as possible thus the so called golden hour of trauma. This is not a strict deadline, but recognizes that many deaths which can be prevented by appropriate care occurring in a relatively short time after injury.[22]
Community-based trauma referral systems seek to decrease overall injury-related morbidity and mortality and years of life lost within a population by ensuring the provision of optimal care during both the acute and late phases of injury.[9] The care of acutely injured people is a public health issue that involves bystanders and community members, health care professionals, and health care systems. It encompasses prehospital assessment and care by emergency medical services personnel, emergency department assessment, treatment, and stabilization, and in-hospital care among all age groups.[23] An established trauma system network is also an important component of community disaster preparedness, facilitating the care of victims of natural disasters or terrorist attacks.[9] In those with cardiac arrest due to trauma cardiopulmonary resuscitation (CPR) is considered futile but still recommended.[24]
Intravenous fluids
Traditionally high volume intravenous fluids were given in people with hemodynamic instability due to trauma. This is still appropriate for those with isolated extremity, thermal or head injuries.[25] The current evidence however supports limiting the use of fluids for penetrating thorax and abdominal injuries allowing mild hypotension to persist (known as permissive hypotension).[4][25] A target mean arterial pressure of 60mmHg or a systolic blood pressure of 90 mmHg is recommended.[26] If blood products are needed a greater relative use of fresh frozen plasma and platelets to packed red blood cells has been found to result in improved survival and less overall blood product usage.[27] A ratio of one:one:one is recommended.[26]
Blood substitutes such as hemoglobin-based oxygen carriers and perfluorocarbon emulsions are in development. As of June 2008 however there are none available for commercial use in North America or Europe.[28][29] The only countries where these products are available for general use is South Africa and Russia.[28]
Medications
In people who are bleeding due to trauma tranexamic acid decreases mortality.[30][31] Factor VII may also be appropriate in certain cases associated with severe bleeding[25] such as those who have bleeding disorders.[5] While it decreases blood use it does not appear to decrease mortality.[32]
Surgery
Further information: Trauma surgeryDamage control surgery is employed in the management of trauma.[5] This involves performing the least number of procedures to save life and limb.[5] Less critical procedures are left until the person is more stable.[5]
Prognosis
Death from trauma have been classically described as occurring during three peaks: immediately, early, and late. The immediate deaths are usually due to apnea, severe brain or high spinal cord injury, and rupture of the heart or large blood vessels. The early deaths occur within minutes to hours and are often due to a subdural hematoma, epidural hematoma, hemothorax, pneumothorax, ruptured spleen, liver laceration, or pelvic fractures. This is known as the golden hour. The late deaths occur days or weeks after the injury.[10] This classical distribution however may no longer be occurring in the United States due to improvements in care.[5]
Long term prognosis is also frequently complicated by pain with over half of people having moderately severe pain one year later.[33] Many also experience a reduced quality of life years later.[34] 20% of people who sustain a traumatic injury will sustain some form of disability.[35] Physical trauma can lead to development of post-traumatic stress disorder (PTSD).[36] However, one study found no correlation between the severity of trauma and the development of PTSD.[37]
Epidemiology
Further information: List of preventable causes of death Deaths from injuries per 100,000 inhabitants in 2004[38]
Deaths from injuries per 100,000 inhabitants in 2004[38] no data< 2525-5050-7575-100100-125125-150150-175175-200200-225225-250250-275> 275
no data< 2525-5050-7575-100100-125125-150150-175175-200200-225225-250250-275> 275Trauma is the sixth leading cause of death (accounting for 10% of all mortality) worldwide, and the fifth leading cause of significant disability.[3] In people between the ages of 1–45 years, trauma is the leading cause of death.[3][4][22][35][39] The primary causes of death are central nervous system injury, followed by exsanguination.[3]
Research
See also: TraumatologyPatients who were admitted into an ICU and received a trauma diagnosis causes a negative change in their health related quality of life with a potential to create anxiety and symptoms of depression.[40]
In children
Main article: Pediatric traumaAccidents are the leading cause of death in children 1–14 years of age.[35] In the US approximatively 16,000,000 children go to an emergency department due to some form of injury every year.[35] Male children are more frequently injured then female children by a ratio of two to one.[35] The top five worldwide unintentional injuries in children are as follows:[41]
Cause Number of deaths resulting Traffic collision 260,000 per year
Drowning 175,000 per year
Burns 96,000 per year
Falls 47,000 per year
Toxins 45,000 per year
An important part of managing trauma in children is weight estimation. A number of methods to estimate weight exist including the: Broselow tape, Leffler formula, and Theron formula.[42]
In pregnancy
Trauma occurs in 6-7% of all pregnancies and is the leading cause of maternal death. Trauma during pregnancy is a serious issue as the mothers will have an increased heart rate and increased blood pressure to accommodate the child, these hemodynamic changes will alter the presentation of shock.[4][43]
There are diagnostic issues during pregnancy as ionizing radiation can cause birth defects[4]
References
- ^ "Trauma". Dictionary.com. Dictionary.com, LLC. 2010. http://dictionary.reference.com/browse/trauma. Retrieved 2010-10-31.
- ^ Elizabeth Martin, ed (2010). "Concise Medical Dictionary". Concise Medical Dictionary (Eighth ed.). Market House Books Ltd.
- ^ a b c d Søreide K (2009). "Epidemiology of major trauma". The British journal of surgery 96 (7): 697–8. doi:10.1002/bjs.6643. PMID 19526611. http://www.ingentaconnect.com/content/jws/bjs/2009/00000096/00000007/art00001.
- ^ a b c d e f Marx, J (2010). Rosen's emergency medicine: concepts and clinical practice 7th edition. Philadelphia: Mosby/Elsevier. pp. 243–842. ISBN 9780323054720.
- ^ a b c d e f g h i j k l m n Bonatti, H; Calland, JF (2008). "Trauma". Emergency Medicine Clinics of North America 26 (3): 625–48. doi:10.1016/j.emc.2008.05.001. PMID 18655938.
- ^ a b DiPrima Jr., PA. McGraw-Hill's EMT-Basic. McGraw-Hill. pp. 227–33. ISBN 978-0-07-149679-7.
- ^ a b Dickenson ET, Limmer D, O'Keefe MF (2009). Emergency Care. ISBN 978-0-13-500523-1.
- ^ Medzon R, Mitchell EJ (2005). Introduction to Emergency Medicine. Philadelphia: Lippincott Williams & Willkins. pp. 393–431. ISBN 078173200x.
- ^ a b c Hoyt, DB; Coimbra, R (2007). "Trauma systems". Surgical Clinics of North America 87 (1): 21–35, v–vi. doi:10.1016/j.suc.2006.09.012. PMID 17127121.
- ^ a b c d Committee on Trauma, American College of Surgeons (2008). ATLS: Advanced Trauma Life Support Program for Doctors (8th ed.). Chicago: American College of Surgeons. ISBN 9781880696316.
- ^ a b McGillicuddy EA, Schuster KM, Kaplan LJ, et al. (2010). "Contrast-induced nephropathy in elderly trauma patients". J Trauma 68 (2): 294–7. doi:10.1097/TA.0b013e3181cf7e40. PMID 20154540.
- ^ Huber-Wagner S, Lefering R, Qvick LM, et al. (2009). "Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study". Lancet 373 (9673): 1455–61. doi:10.1016/S0140-6736(09)60232-4. PMID 19321199.
- ^ Allen TL, Mueller MT, Bonk RT, Harker CP, Duffy OH, Stevens MH (2004). "Computed tomographic scanning without oral contrast solution for blunt bowel and mesenteric injuries in abdominal trauma". J Trauma 56 (2): 314–22. doi:10.1097/01.TA.0000058118.86614.51. PMID 14960973.
- ^ Korley FK, Pham JC, Kirsch TD (2010). "Use of advanced radiology during visits to US emergency departments for injury-related conditions,1998-2007". JAMA 304 (13): 1465–71. doi:10.1001/jama.2010.1408. PMID 20924012.
- ^ Neal MD, Peitzman AB, Forsythe RM, et al. (February 2011). "Over reliance on computed tomography imaging in patients with severe abdominal injury: is the delay worth the risk?". J Trauma 70 (2): 278–84. doi:10.1097/TA.0b013e31820930f9. PMID 21307722.
- ^ Nirula R, Maier R, Moore E, Sperry J, Gentilello L (2010). "Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer's effect on mortality". J Trauma 69 (3): 595–9; discussion 599–601. doi:10.1097/TA.0b013e3181ee6e32. PMID 20838131.
- ^ Karbi, OA; Caspari, DA; Tator, CH (1988). "Extrication, immobilization and radiologic investigation of patients with cervical spine injuries". Canadian Medical Association Journal 139 (7): 617–21. PMC 1268249. PMID 3046734. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1268249.
- ^ Sullivent, EE; Faul, M, Wald, MM (2011 Jul-Sep). "Reduced mortality in injured adults transported by helicopter emergency medical services". Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors 15 (3): 295–302. doi:10.3109/10903127.2011.569849. PMID 21524205.
- ^ Stiell IG, Nesbitt LP, Pickett W, et al. (2008). "The OPALS Major Trauma Study: impact of advanced life-support on survival and morbidity". CMAJ 178 (9): 1141–52. doi:10.1503/cmaj.071154. PMC 2292763. PMID 18427089. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2292763.
- ^ Liberman M, Roudsari BS (2007). "Prehospital trauma care: what do we really know?". Curr Opin Crit Care 13 (6): 691–6. doi:10.1097/MCC.0b013e3282f1e77e. PMID 17975392.
- ^ Dretzke J, Sandercock J, Bayliss S, Burls A (2004). "Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients". Health Technol Assess 8 (23): iii, 1–103. PMID 15193210.
- ^ a b "Tabers Cyclopedic Medical Dictionary". Tabers Cyclopedic Medical Dictionary. Philadelphia: F.A. Davis Company. 2009. pp. 2366–7\author=Davis FA. ISBN 978-0-8036-1559-5.
- ^ "Centers for Disease Control and Prevention Injury Prevention and Control: Injury Response: Acute Injury Care". http://www.cdc.gov/injuryresponse/acute_injury.html.
- ^ Vanden Hoek, TL; Morrison, LJ, Shuster, M, Donnino, M, Sinz, E, Lavonas, EJ, Jeejeebhoy, FM, Gabrielli, A (2010-11-02). "Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation 122 (18 Suppl 3): S829–61. doi:10.1161/CIRCULATIONAHA.110.971069. PMID 20956228.
- ^ a b c Roppolo LP, Wigginton JG, Pepe PE (2010). "Intravenous fluid resuscitation for the trauma patient". Curr Opin Crit Care 16 (4): 283–8. doi:10.1097/MCC.0b013e32833bf774. PMID 20601865.
- ^ a b Tintinalli, Judith E. (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. pp. 176. ISBN 0-07-148480-9.
- ^ Greer SE, Rhynhart KK, Gupta R, Corwin HL (2010). "New developments in massive transfusion in trauma". Curr Opin Anaesthesiol 23 (2): 246–50. doi:10.1097/ACO.0b013e328336ea59. PMID 20104173.
- ^ a b "UpToDate Inc.". http://www.uptodate.com/online/content/topic.do?topicKey=transfus/11560&selectedTitle=1~8&source=search_result. Retrieved 2010-11-13.
- ^ Spahn DR, Kocian R (2005). "Artificial O2 carriers: status in 2005". Curr. Pharm. Des. 11 (31): 4099–114. doi:10.2174/138161205774913354. PMID 16378514. http://www.bentham-direct.org/pages/content.php?CPD/2005/00000011/00000031/0011B.SGM.
- ^ Crash-2 Trial, Collaborators; Shakur, H; Roberts, R; Bautista, R; Caballero, J; Coats, T; Dewan, Y; El-Sayed, H et al. (2010). "Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial". The Lancet 376 (9734): 23–32. doi:10.1016/S0140-6736(10)60835-5. PMID 20554319.
- ^ Cap, AP; Baer, DG, Orman, JA, Aden, J, Ryan, K, Blackbourne, LH (2011 Jul). "Tranexamic acid for trauma patients: a critical review of the literature". The Journal of trauma 71 (1 Suppl): S9–14. doi:10.1097/TA.0b013e31822114af. PMID 21795884.
- ^ Hauser CJ, Boffard K, Dutton R, et al. (September 2010). "Results of the CONTROL trial: efficacy and safety of recombinant activated Factor VII in the management of refractory traumatic hemorrhage". J Trauma 69 (3): 489–500. doi:10.1097/TA.0b013e3181edf36e. PMID 20838118.
- ^ Rivara FP, Mackenzie EJ, Jurkovich GJ, Nathens AB, Wang J, Scharfstein DO (2008). "Prevalence of pain in patients 1 year after major trauma". Arch Surg 143 (3): 282–7; discussion 288. doi:10.1001/archsurg.2007.61. PMID 18347276.
- ^ Ulvik A, Kvåle R, Wentzel-Larsen T, Flaatten H (2008). "Quality of life 2-7 years after major trauma". Acta Anaesthesiol Scand 52 (2): 195–201. doi:10.1111/j.1399-6576.2007.01533.x. PMID 18005377.
- ^ a b c d e Peitzman AB, Rhodes M, Schwab CW, Yealy DM, Fabian TC, ed (2008). "Pediatric Trauma". The Trauma Manual (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 499–514. ISBN 0781762758. http://www.amazon.com/Trauma-Manual-Surgery-Lippincott-Formerly/dp/0781762758.
- ^ "309.81 Posttraumatic Stress Disorder". Diagnostic and Statistical Manual of Mental Disorders. Washington, USA: American Psychiatric Association. 1994. pp. 424–429. http://www.cirp.org/library/psych/ptsd2/.
- ^ Feinstein, A; Dolan, Ray (1991). "Predictors of post-traumatic stress disorder following physical trauma: an examination of the stressor criterion". Psychological Medicine (Cambridge University Press) 21 (1): 85–91. doi:10.1017/S0033291700014689. PMID 2047509.
- ^ "Death and DALY estimates for 2004 by cause for WHO Member States" (xls). World Health Organization. 2004. http://www.who.int/entity/healthinfo/global_burden_disease/gbddeathdalycountryestimates2004.xls. Retrieved 2010-11-13.
- ^ Peters S, Nicolas V, Heyer CM (2010). "Multidetector computed tomography-spectrum of blunt chest wall and lung injuries in polytraumatized patients". Clin Radiol 65 (4): 333–8. doi:10.1016/j.crad.2009.12.008. PMID 20338402.
- ^ Ringdal M, Plos K, Lundberg D, Johansson L, Bergbom I (2009). "Outcome after injury: memories, health-related quality of life, anxiety, and symptoms of depression after intensive care". J Trauma 66 (4): 1226–33. doi:10.1097/TA.0b013e318181b8e3. PMID 19088550.
- ^ BBC News Online (December 10, 2008). "UN raises child accidents alarm". BBC News. London: BBC. http://news.bbc.co.uk/2/hi/in_depth/7776127.stm. Retrieved 2010-10-31.
- ^ So TY, Farrington E, Absher RK (2009). "Evaluation of the accuracy of different methods used to estimate weights in the pediatric population". Pediatrics 123 (6): e1045–51. doi:10.1542/peds.2008-1968. PMID 19482737.
- ^ Campbell, John Creighton (2000). Basic trauma life support for paramedics and other advanced providers. Upper Saddle River, N.J: Brady/Prentice Hall Health. pp. 239–47. ISBN 0-13-084584-1.
Further reading
- Editorial Board, Army Medical Department Center & School, ed (2004). Emergency War Surgery (3rd ed.). Washington, DC: Borden Institute. http://www.bordeninstitute.army.mil/other_pub/ews.html.
- Zajtchuk, R; Bellamy, RF; Grande, CM, eds (1995). Textbook of Military Medicine, Part IV: Surgical Combat Casualty Care. 1: Anesthesia and Perioperative Care of the Combat Casualty. Washington, DC: Borden Institute. http://www.bordeninstitute.army.mil/published_volumes/anesthesia/anesthesia.html.
External links
- International Trauma Conferences (registered trauma charity providing trauma education for medical professionals worldwide)
- Trauma.org (trauma resources for medical professionals)
- Emergency Medicine Research and Perspectives (emergency medicine procedure videos)
- American Trauma Society
- Society of Trauma Nurses
- Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine
- Definitive Surgical Trauma Skills
- After the Injury- Children's Hospital Of Philadelphia
General wounds and injuries (T08-T35, 870-949) General Wound/
traumaBlister (Blood blister • Coma blister • Delayed blister • Edema blister • Fracture blister • Friction blister • Sucking blister)
Bruise/Hematoma/Ecchymosis (Battle's sign, Raccoon eyes, Black eye, Subungual hematoma, Cullen's sign, Grey Turner's sign, Retroperitoneal hemorrhage)
Animal bite: Insect bite · Spider biteAnimal bite: Snakebite · Lizard bite
Ballistic traumaForeign body In alimentary tract (Bezoar)Other By region Health science > Medicine > Emergency medicine Procedures Acute Care of at-Risk Newborns (ACoRN) · Advanced cardiac life support (ACLS) · Advanced Trauma Life Support (ATLS) · Cardiopulmonary resuscitation (CPR) · First aid · Neonatal Resuscitation Program (NRP) · Pediatric Advanced Life Support (PALS) · Basic Life SupportEquipment Bag valve mask (BVM) · Chest tube · Defibrillation (AED, ICD) · Electrocardiogram (ECG/EKG) · Intraosseous infusion (IO) · Intravenous therapy (IV) · Tracheal intubation · Nasopharyngeal airway (NPA) · Oropharyngeal airway (OPA) · Pocket maskDrugs Other  Book:Emergency medicine ·
Book:Emergency medicine ·  Category:Emergency medicine ·
Category:Emergency medicine ·  Portal:MedicineCategories:
Portal:MedicineCategories:- Medical emergencies
- Traumatology
- Causes of death
Wikimedia Foundation. 2010.