- Drowning
-
Drowning / Near Drowning Classification and external resources 
Vasily Perov: The drowned, 1867ICD-10 T75.1 ICD-9 994.1 DiseasesDB 3957 MedlinePlus 000046 eMedicine emerg/744 MeSH C23.550.260.393 Drowning is death from asphyxia due to suffocation caused by water entering the lungs and preventing the absorption of oxygen leading to cerebral hypoxia.[1]
Near drowning is the survival of a drowning event involving unconsciousness or water inhalation and can lead to serious secondary complications, including death, after the event.[1][2]
According to the World Health Organization, drowning is the 3rd leading cause of unintentional injury death worldwide, accounting for 7% of all injury related deaths (est. 388,000 deaths by drowning in 2004, excluding those due to natural disasters), with 96% of these deaths occurring in low- and middle-income countries.[3] In many countries, drowning is one of the leading causes of death for children under 12 years old. For example, in the United States, it is the second leading cause of death (after motor vehicle crashes) in children 12 and younger.[4] The rate of drowning in populations around the world varies widely according to their access to water, the climate and the national swimming culture.
Drowning itself is quick and silent, although it may be preceded by distress which is more visible.[5] A person drowning is unable to shout or call for help, or seek attention, as they cannot obtain enough air. The instinctive drowning response is the final set of autonomic reactions in the 20 – 60 seconds before sinking underwater, and to the untrained eye can look similar to calm safe behavior.[5][6] Lifeguards and other persons trained in rescue learn to recognize drowning people by watching for these instinctive movements.[5]
Drowning occurs more frequently in males and the young.[4] Surveys indicate that 10% of children under 5 have experienced a situation with a high risk of drowning.
Contents
Classification
Experts differentiate between distress and drowning. They also divide drowning into passive and secondary:
- Distress - these are people in trouble and distress, but who still have the ability to keep afloat, signal for help and take actions.
- Drowning - these are people suffocating and in imminent danger of death within seconds, and fall into two categories:
-
- Passive drowning - people who suddenly sink or have sunk due to a change in their circumstances. Examples include people who drown in an accident, or due to sudden loss of consciousness or sudden medical condition.
-
Active drowning - people such as non-swimmers and the exhausted or hypothermic at the surface, who are unable to hold their mouth above water and are suffocating due to lack of air. Instinctively, people in such cases perform well known behaviors in the last 20 - 60 seconds before being submerged, representing the body's last efforts to obtain air.
Notably such people are unable to call for help, talk, reach for rescue equipment, or alert swimmers even feet away, and they may drown quickly and silently close to other swimmers or safety.
Behavior, signs and symptoms
Main article: Instinctive drowning responseDrowning is most often quick and unspectacular. Its media depictions as a loud, violent struggle have much more in common with distressed non-swimmers, who may well drown but have not yet begun. In particular, an asphyxiating person is seldom able to call for help.[7] The instinctive drowning response covers many signs or behaviors associated with drowning or near-drowning:
- Head low in the water, mouth at water level
- Head tilted back with mouth open
- Eyes glassy and empty, unable to focus
- Eyes open, with fear evident on the face
- Hyperventilating or gasping
- Trying to swim in a particular direction but not making headway
- Trying to roll over on the back to float
- Uncontrollable movement of arms and legs, rarely out of the water.
Pia notes that drowning begins at the point a person is unable to keep their mouth above water; inhalation of water takes place at a later stage.[8] Most victims demonstrating the instinctive drowning response do not show prior evidence of distress.[8]
Cause
Most drownings occur when the victim is in water (90% in freshwater (rivers, lakes and pools), 10% in seawater). Drownings in other fluids are rare, and are often related to industrial accidents.[citation needed]
People have drowned in as little as 30 mm of water lying face down, in one case in a wheel rut.[citation needed] Children have drowned in baths, buckets and toilets; inebriates or those under the influence of drugs have died in puddles.
Drowning can take place in other circumstances than those in popular awareness, for instance:
- Deep water blackout - caused by latent hypoxia upon ascent from depth, where the partial pressure of oxygen in the lungs under pressure at the bottom of a deep free-dive is adequate to support consciousness but drops below the blackout threshold as the water pressure decreases on the ascent. It usually strikes upon arriving near the surface as the pressure approaches normal atmospheric pressure.
- Shallow water blackout - caused by hyperventilation prior to swimming or diving. The primary urge to breathe (more precisely: to exhale) is triggered by rising carbon dioxide (CO2) levels in the bloodstream.[9] The body detects CO2 levels very accurately and relies on this to control breathing.[9] Hyperventilation artificially depletes this, but leaves the diver susceptible to sudden loss of consciousness without warning from hypoxia. There is no bodily sensation that warns a diver of an impending blackout, and victims (often capable swimmers swimming under the surface in shallow water) become unconscious and drown quietly without alerting anyone to the fact that there is a problem; they are typically found on the bottom.
- Secondary drowning - Inhaled fluid can act as an irritant inside the lungs. Physiological responses to even small quantities include the extrusion of liquid into the lungs (pulmonary edema) over the following hours, but this reduces the ability to exchange air and can lead to a person "drowning in their own body fluid". Certain poisonous vapors or gases (as for example in chemical warfare), or vomit can have a similar effect. The reaction can take place up to 72 hours after a near drowning incident, and may lead to a serious condition or death.
Pathophysiology
Clinical background
A continued lack of oxygen in the brain, known as hypoxia, will quickly render a victim unconscious usually around a blood partial pressure of oxygen of 25-30 mmHg. An unconscious victim rescued with an airway still sealed from Laryngospasm (involuntary sealing of the throat) stands a good chance of a full recovery. Artificial respiration is also much more effective without water in the lungs. At this point the victim stands a good chance of recovery if attended to within minutes.
Overview
A continued lack of oxygen in the brain, hypoxia, will quickly render a victim unconscious usually around a blood partial pressure of oxygen of 25-30mmHg. An unconscious victim rescued with an airway still sealed from laryngospasm stands a good chance of a full recovery. Artificial respiration is also much more effective without water in the lungs. At this point the victim stands a good chance of recovery if attended to within minutes. Latent hypoxia is a special condition leading to unconsciousness where the partial pressure of oxygen in the lungs under pressure at the bottom of a deep free-dive is adequate to support consciousness but drops below the blackout threshold as the water pressure decreases on the ascent, usually close to the surface as the pressure approaches normal atmospheric pressure. A blackout on ascent like this is called a deep water blackout.
The brain cannot survive long without oxygen and the continued lack of oxygen in the blood combined with the cardiac arrest will lead to the deterioration of brain cells causing first brain damage and eventually brain death from which recovery is generally considered impossible.
A lack of oxygen or chemical changes in the lungs may cause the heart to stop beating; this cardiac arrest stops the flow of blood and thus stops the transport of oxygen to the brain. Cardiac arrest used to be the traditional point of death but at this point there is still a chance of recovery. The brain will die after approximately six minutes without oxygen but special conditions may prolong this (see 'cold water drowning' below).
As well as the direct effect of oxygen deprivation, there are also dangerous effects on blood chemistry if water is taken into the lungs. The mechanism for this is different for fresh and seawater.
-
- Freshwater taken into the lungs will be pulled into the pulmonary circulation by osmosis. The dilution of blood leads to hemolysis (bursting of red blood cells). The resulting elevation of plasma K+ (potassium) level and depression of Na+ (sodium) level alter the electrical activity of the heart often causing ventricular fibrillation. In animal experiments this effect was shown to be capable of causing cardiac arrest in 2 to 3 minutes. Acute renal failure can also result from hemoglobin from the burst blood cells accumulating in the kidneys, and cardiac arrest can also result if cold freshwater taken into the bloodstream sufficiently cools the heart.
-
- Sea water is hypertonic to blood (more salty). It poses the opposite danger. Osmosis will instead pull water from the bloodstream into the lungs, thickening the blood. In animal experiments the thicker blood requires more work from the heart leading to cardiac arrest in 8 to 10 minutes.
Autopsies on human drowning victims show no indications of these effects and there appears to be little difference between drownings in salt water and fresh water. After death, rigor mortis will set in and remains for about two days, depending on many factors including water temperature.
Body's reaction to submersion
Submerging the face in water colder than about 21 °C (70 °F) triggers the mammalian diving reflex, found in mammals, and especially in marine mammals such as whales and seals. This reflex protects the body by putting it into energy saving mode to maximize the time it can stay under water. The strength of this reflex is greater in colder water and has three principal effects:
- Bradycardia, a slowing of the heart rate by up to 50% in humans.
- Peripheral vasoconstriction, the restriction of the blood flow to the extremities to increase the blood and oxygen supply to the vital organs, especially the brain.
- Blood Shift, the shifting of blood to the thoracic cavity, the region of the chest between the diaphragm and the neck, to avoid the collapse of the lungs under higher pressure during deeper dives.
The reflex action is automatic and allows both a conscious and an unconscious person to survive longer without oxygen under water than in a comparable situation on dry land. The exact mechanism for this effect has been debated and may be a result of brain cooling similar to the protective effects seen in patients treated with deep hypothermia.[10][11]
Oxygen deprivation
A conscious victim will hold his or her breath (see Apnea) and will try to access air, often resulting in panic, including rapid body movement. This uses up more oxygen in the blood stream and reduces the time to unconsciousness. The victim can voluntarily hold his or her breath for some time, but the breathing reflex will increase until the victim will try to breathe, even when submerged.
The breathing reflex in the human body is weakly related to the amount of oxygen in the blood but strongly related to the amount of carbon dioxide (see Hypercapnia). During apnea, the oxygen in the body is used by the cells, and excreted as carbon dioxide. Thus, the level of oxygen in the blood decreases, and the level of carbon dioxide increases. Increasing carbon dioxide levels lead to a stronger and stronger breathing reflex, up to the breath-hold breakpoint, at which the victim can no longer voluntarily hold his or her breath. This typically occurs at an arterial partial pressure of carbon dioxide of 55 mm Hg, but may differ significantly from individual to individual and can be increased through training.
The breath-hold break point can be suppressed or delayed either intentionally or unintentionally. Hyperventilation before any dive, deep or shallow, flushes out carbon dioxide in the blood resulting in a dive commencing with an abnormally low carbon dioxide level; a potentially dangerous condition known as hypocapnia. The level of carbon dioxide in the blood after hyperventilation may then be insufficient to trigger the breathing reflex later in the dive and a blackout may occur without warning and before the diver feels any urgent need to breathe. This can occur at any depth and is common in distance breath-hold divers in swimming pools. Hyperventilation is often used by both deep and distance free-divers to flush out carbon dioxide from the lungs to suppress the breathing reflex for longer. It is important not to mistake this for an attempt to increase the body's oxygen store. The body at rest is fully oxygenated by normal breathing and cannot take on any more. Breath holding in water should always be supervised by a second person, as by hyperventilating, one increases the risk of shallow water blackout because insufficient carbon dioxide levels in the blood fail to trigger the breathing reflex.
Water inhalation
If water enters the airways of a conscious victim, the victim will try to cough up the water or swallow it, thus inhaling more water involuntarily. Upon water entering the airways, both conscious and unconscious victims experience laryngospasm, that is the larynx or the vocal cords in the throat constrict and seal the air tube. This prevents water from entering the lungs. Because of this laryngospasm, water enters the stomach in the initial phase of drowning and very little water enters the lungs. Unfortunately, this can interfere with air entering the lungs, too. In most victims, the laryngospasm relaxes some time after unconsciousness and water can enter the lungs causing a "wet drowning". However, about 10-15% of victims maintain this seal until cardiac arrest. This is called "dry drowning", as no water enters the lungs. In forensic pathology, water in the lungs indicates that the victim was still alive at the point of submersion. Absence of water in the lungs may be either a dry drowning or indicates a death before submersion.
Management
Rescue involves bringing the persons mouth and nose above the water surface. A drowning person may cling to the rescuer and try to pull himself out of the water, submerging the rescuer in the process. Thus it is advised that the rescuer approach with a buoyant object, or from behind, twisting the person's arm on the back to restrict movement. If the rescuer does get pushed under water, they should dive downwards to escape the person.
After a successful approach, negatively buoyant objects such as a weight belt are removed. The priority is then to transport the person to the water's edge in preparation for removal from the water. The person is turned on their back with a secure grip used to tow from behind. If the person is cooperative they may be towed in a similar fashion held at the armpits. If the person is unconscious they may be pulled in a similar fashion held at the chin and cheeks, ensuring that the mouth and nose are well above the water.
Special care has to be taken for people with suspected spinal injuries, and a back board (spinal board) may be needed for the rescue. In water, CPR is ineffective, and the goal should be to bring the person to a stable ground quickly and then to start CPR. Once on ground chest compressions are performed if the patient is pulseless, and if they are not breathing rescue breaths.[12] 100% oxygen is neither recommended nor discouraged.[13] Treatment for hypothermia may also be necessary.
The Heimlich maneuver is not recommended;[14] the technique may have relevance in situations where airways are obstructed by solids but not fluids. Performing the manoeuver on drowning people not only delays ventilation but may induce vomiting, which if aspirated will place the patient in a far worse situation. Moreover, the use of the Heimlich manoeuver in any choking situation involving solids or fluids has become controversial and is generally no longer taught. For more information on this debate refer to the article Henry Heimlich.
Because of the mammalian diving reflex (see above), person submerged in cold water and apparently drowned may revive after a relatively long period. Rescuers retrieving an apparently dead person from water significantly below body temperature should not consider the rescued person dead until he or she is warm and dead.[citation needed]
Surveillance
Many pools and designated bathing areas either have lifeguards, a pool safety camera system for local or remote monitoring, or computer aided drowning detection. However, bystanders play an important role in drowning detection and either intervention or the notification of authorities by phone or alarm.
Epidemiology
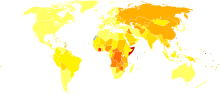 Disability-adjusted life year for drowning per 100,000 inhabitants in 2004.[15]
Disability-adjusted life year for drowning per 100,000 inhabitants in 2004.[15] no data< 100100-150150-200200-250250-300300-350350-400400-450450-500500-600600-700> 700
no data< 100100-150150-200200-250250-300300-350350-400400-450450-500500-600600-700> 700In the United States in 2006, 1100 people under 20 years of age died from drowning.[16] Typically the United Kingdom suffers 450 drownings per annum or 1 per 150,000 of population whereas the United States suffers 6,500 drownings or around 1 per 50,000 of population. In Asia, according to a study by The Alliance for Safe Children, suffocation and drowning were the most easily preventable causes of death for children under five years of age;[17][18] a 2008 report by the organization found that in Bangladesh, for instance, 46 children drown each day.[19]
People who drown are more likely to be male, young or adolescent.[4] Surveys indicate that 10% of children under 5 have experienced a situation with a high risk of drowning. About 175,000 children die through drowning every year.[20] The causes of drowning cases in the US from 1999 to 2006 are as follows[21]:
31.0% Drowning and submersion while in natural water
27.9% Unspecified drowning and submersion
14.5% Drowning and submersion while in swimming pool
9.4% Drowning and submersion while in bathtub
7.2% Drowning and submersion following fall into natural water
6.3% Other specified drowning and submersion
2.9% Drowning and submersion following fall into swimming pool
0.9% Drowning and submersion following fall into bathtubSociety and culture
In Europe, drowning was used as capital punishment. In fact, during the Middle Ages, a sentence of death was read using the words "cum fossa et furca," or "with drowning-pit and gallows." Furthermore, drowning was used as a way to determine if a woman was a witch. The idea was that witches would float and innocent women would drown. For more details, see trial by drowning. It is understood that drowning was used as the least brutal form of execution, and was therefore reserved primarily for women, although favoured men were executed in this way as well.
Drowning survived as a method of execution in Europe until the 17th and 18th centuries. England had abolished the practice by 1623, Scotland by 1685, Switzerland in 1652, Austria in 1776, Iceland in 1777, and Russia by the beginning of the 1800s. France revived the practice during the French Revolution (1789–1799) and was carried out by Jean-Baptiste Carrier at Nantes.[22]
References
- ^ a b Lunetta, P. & Modell, J.H. (2005): Macropathological, Microscopical, and Laboratory Findings in Drowning Victims. In: Tsokos, M. (ed.): Forensic Pathology Reviews, Vol. 3. Humana Pres Inc.; Totowa, NJ, pp.: 4-77.
- ^ Dueker CW, Brown SD (eds) (1999). "Near Drowning Workshop. 47th Undersea and Hyperbaric Medical Society Workshop". UHMS Publication Number WA292. (Undersea and Hyperbaric Medical Society): 63. http://archive.rubicon-foundation.org/8024. Retrieved 2009-04-26.
- ^ "Fact sheet N°347, November 2010: "Drowning"". World Health organization. http://www.who.int/mediacentre/factsheets/fs347/en/index.html. Retrieved 2010-12-30.
- ^ a b c Centers for Disease Control, Resources for TV Writers and Producers
- ^ a b c Vittone, Aviation Survival Technician First Class Mario; Pia, Francesco Ph.D. (Fall 2006). ""It Doesn't Look Like They're Drowning": How To Recognize the Instinctive Drowning Response". On Scene (journal of US Coastguard search and rescue). p. 14. http://www.uscg.mil/hq/cg5/cg534/On%20Scene/OSFall06.pdf. Retrieved 2010-12-29.
- ^ O'Connell, Claire (2010-08-03). "What stops people shouting and waving when drowning?". Irish Times. http://www.irishtimes.com/newspaper/health/2010/0803/1224276085079.html. Retrieved 2010-12-29.
- ^ Mario Vittoine, Francesco Pia: "It Doesn’t Look Like They’re Drowning: How To Recognize the Instinctive Drowning Response", On Scene, Fall 2006, p. 14.
- ^ a b Fletemeyer, John; Pia (Chapter author) (1999). "Chapter 14 ("Reflections on Lifeguard surveillance programs")". Drowning: new perspectives on intervention and prevention, Volume 1998. pp. 234. ISBN 9781574442236. http://books.google.com/?id=Xcnwm8zE24QC&dq=drowning+new+perspectives+on+intervention+and+prevention.
- ^ a b Lindholm P, Lundgren CE (2006). "Alveolar gas composition before and after maximal breath-holds in competitive divers". Undersea & Hyperbaric Medicine : Journal of the Undersea and Hyperbaric Medical Society, Inc 33 (6): 463–7. PMID 17274316. http://archive.rubicon-foundation.org/5053. Retrieved 2010-12-30.
- ^ Lundgren, Claus EG; Ferrigno, Massimo (eds). (1985). Physiology of Breath-hold Diving. 31st Undersea and Hyperbaric Medical Society Workshop. UHMS Publication Number 72(WS-BH)4-15-87.. Undersea and Hyperbaric Medical Society. http://archive.rubicon-foundation.org/7992. Retrieved 2009-04-24.
- ^ Mackensen GB, McDonagh DL, Warner DS (March 2009). "Perioperative hypothermia: use and therapeutic implications". J. Neurotrauma 26 (3): 342–58. doi:10.1089/neu.2008.0596. PMID 19231924.
- ^ "Statements on Positioning a Patient on a sloping Beach". International Life Saving Federation. http://www.ilsf.org/medical/statements/sloping-beach-positioning. Retrieved 2009-01-25.
- ^ "2005 ILCOR resuscitation guidelines" (PDF). Circulation 112 (22 supplement). November 29, 2005. doi:10.1161/CIRCULATIONAHA.105.166480 (inactive 2008-06-28). http://circ.ahajournals.org/cgi/reprint/112/22_suppl/III-115.pdf. Retrieved 2008-02-17. "There is insufficient evidence to recommend for or against the use of oxygen by the first aid provider."
- ^ http://www.nlm.nih.gov/medlineplus/ency/article/000046.htm
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html. Retrieved Nov. 11, 2009.
- ^ "Policy Statement--Prevention of Drowning -- COMMITTEE ON INJURY, VIOLENCE, AND POISON PREVENTION, 10.1542/peds.2010-1264 -- Pediatrics". http://pediatrics.aappublications.org/cgi/content/abstract/peds.2010-1264v1.
- ^ "Drowning, Homicide and Suicide Leading Killers for Children in Asia". The Salem News. 11 March 2008. http://www.salem-news.com/articles/march112008/asia_child_killers_031108.php. Retrieved 5 October 2010.
- ^ "UNICEF Says Injuries A Fatal Problem For Asian Children". All Headline News. 13 March 2008. http://www.allheadlinenews.com/articles/7010320559. Retrieved 5 October 2010.
- ^ "Children Drowning, Drowning Children". The Alliance for Safe Children. http://tasc-gcipf.org/downloads/Drowning%20in%20Bangladesh.pdf. Retrieved 6 October 2010.
- ^ "Traffic Accidents Top Cause Of Fatal Child Injuries". NPR: National Public Radio. December 10, 2008.
- ^ http://www.cdc.gov/injury/wisqars/index.html
- ^ (web site) 1911 Encyclopedia: Drowning and life-saving. April 21, 2008. http://www.1911encyclopedia.org/Drowning_and_life_saving. Retrieved 2008-04-21.
External links
- Drowning prevention information from Seattle Children's Hospital.
- Information on search and recovery of drowning victims
- Canadian Red Cross: Drowning Research: Drownings in Canada, 10 Years of Research Module 2 - Ice & Cold Water Immersion* Canadian Lifesaving Society Canadian National Drowning Report (1991-2000)
- Training video and example of drowning behaviors (Audio missing during 0:17 - 0:58 of the video)
- World Health Organization fact-sheet on drowning with statistics (latest as of December 2010)
- Proceedings and results of World Congress on Drowning, 2002
- Report into Lifeguard effectiveness, also covering drowning facts and risks - CDC, 2001
Underwater diving Types: 
Specialities: Equipment: Disciplines: Professional diving · Police diving · Military diving · Underwater photography · Underwater videographyHazards: Related: Lifesaving and lifeguarding International standards bodies 
National societies Topics Awards Equipment Consequences of external causes (T66–T78, 990–995) Temperature/radiation reduced temperature: Hypothermia · Immersion foot syndromes (Trench foot • Tropical immersion foot • Warm water immersion foot) · Chilblains · Frostbite · Cold intolerance • Acrocyanosis • Erythrocyanosis crurumradiation: Radiation poisoning · Radiation burn · Chronic radiation keratosis • Eosinophilic, polymorphic, and pruritic eruption associated with radiotherapy • Radiation acne • Radiation cancer • Radiation recall reaction • Radiation-induced erythema multiforme • Radiation-induced hypertrophic scar • Radiation-induced keloid • Radiation-induced morpheaAir Food Maltreatment Emesis Adverse effect Other Ungrouped
skin conditions
resulting from
physical factorsDermatosis neglecta • Pinch mark • Pseudoverrucous papules and nodules • Sclerosing lymphangiitis • Tropical anhidrotic asthenia • UV-sensitive syndromeenvironmental skin conditions: Electrical burn • frictional/traumatic/sports (Black heel and palm • Equestrian perniosis • Jogger's nipple • Pulling boat hands • Runner's rump • Surfer's knots • Tennis toe • Vibration white finger • Weathering nodule of ear • Wrestler's ear • Coral cut • Painful fat herniation ) • Uranium dermatosis
iv use (Skin pop scar • Skin track • Slap mark • Pseudoacanthosis nigricans • Narcotic dermopathy)Categories:- Swimming
- Medical emergencies
- Diving medicine
- Causes of death
- Suicide methods
- Execution methods
Wikimedia Foundation. 2010.

