- Snakebite
-
For other uses, see Snakebite (disambiguation).
Snakebite Classification and external resources 
Cobra Naja najaICD-10 T63.0, T14.1, W59 (nonvenomous), X20 (venomous) ICD-9 989.5, E905.0, E906.2 DiseasesDB 29733 MedlinePlus 000031 eMedicine med/2143 MeSH D012909 A snakebite is an injury caused by a bite from a snake, often resulting in puncture wounds inflicted by the animal's fangs and sometimes resulting in envenomation. Although the majority of snake species are non-venomous and typically kill their prey with constriction rather than venom, venomous snakes can be found on every continent except Antarctica.[1] Snakes often bite their prey as a method of hunting, but also for defensive purposes against predators. Since the physical appearance of snakes may differ, there is often no practical way to identify a species and professional medical attention should be sought.[2][3]
The outcome of snake bites depends on numerous factors, including the species of snake, the area of the body bitten, the amount of venom injected, and the health conditions of the victim. Feelings of terror and panic are common after a snakebite and can produce a characteristic set of symptoms mediated by the autonomic nervous system, such as a racing heart and nausea.[4][5] Bites from non-venomous snakes can also cause injury, often due to lacerations caused by the snake's teeth, or from a resulting infection. A bite may also trigger an anaphylactic reaction, which is potentially fatal. First aid recommendations for bites depend on the snakes inhabiting the region, as effective treatments for bites inflicted by some species can be ineffective for others.
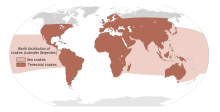
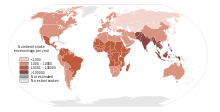
The number of fatalities attributed to snake bites varies greatly by geographical area. Although deaths are relatively rare in Australia, Europe and North America,[1][6][7] the morbidity and mortality associated with snake bites is a serious public health problem in many regions of the world, particularly in rural areas lacking medical facilities. Further, while South Asia, Southeast Asia, and sub-Saharan Africa report the highest number of bites, there is also a high incidence in the Neotropics and other equatorial and subtropical regions.[1][6][7] Each year tens of thousands of people die from snake bites,[1] yet the risk of being bitten can be lowered with preventive measures, such as wearing protective footwear and avoiding areas known to be inhabited by dangerous snakes.
Contents
Signs and symptoms
 Severe gangrene following Bothrops asper envenomation. The victim was an 11-year-old boy, bitten two weeks earlier in Ecuador, but treated only with antibiotics.[11]
Severe gangrene following Bothrops asper envenomation. The victim was an 11-year-old boy, bitten two weeks earlier in Ecuador, but treated only with antibiotics.[11]
The most common symptoms of all snakebites are overwhelming fear, panic, and emotional instability, which may cause symptoms such as nausea and vomiting, diarrhea, vertigo, fainting, tachycardia, and cold, clammy skin.[4][5] Television, literature, and folklore are in part responsible for the hype surrounding snakebites, and a victim may have unwarranted thoughts of imminent death.
Dry snakebites, and those inflicted by a non-venomous species, can still cause severe injury to the victim. There are several reasons for this: a snakebite which is not treated properly may become infected (as is often reported by the victims of viper bites whose fangs are capable of inflicting deep puncture wounds), the bite may cause anaphylaxis in certain people, and the snake's saliva and fangs may harbor many dangerous microbial contaminants, including Clostridium tetani. If neglected, an infection may spread and potentially kill the victim.
Most snakebites, whether by a venomous snake or not, will have some type of local effect. There is minor pain and redness in over 90% of cases, although this varies depending on the site.[4] Bites by vipers and some cobras may be extremely painful, with the local tissue sometimes becoming tender and severely swollen within 5 minutes.[7] This area may also bleed and blister and can eventually lead to tissue necrosis. Other common initial symptoms of pitviper and viper bites include lethargy, bleeding, weakness, nausea, and vomiting.[4][7] Symptoms may become more life-threatening over time, developing into hypotension, tachypnea, severe tachycardia, severe internal bleeding, altered sensorium, kidney failure and respiratory failure.[4][7]
Interestingly, bites caused by the Mojave rattlesnake, kraits, coral snake, and the speckled rattlesnake reportedly cause little or no pain despite being serious injuries.[4] Victims may also describe a "rubbery," "minty," or "metallic" taste if bitten by certain species of rattlesnake.[4] Spitting cobras and rinkhalses can spit venom in their victims' eyes. This results in immediate pain, ophthalmoparesis, and sometimes blindness.[12][13]
Some Australian elapids and most viper envenomations will cause coagulopathy, sometimes so severe that a person may bleed spontaneously from the mouth, nose, and even old, seemingly-healed wounds.[7] Internal organs may bleed, including the brain and intestines and will cause ecchymosis (bruising) of the victim's skin.
Venom emitted from elapids, including sea snakes, kraits, cobras, king cobra, mambas, and many Australian species, contain toxins which attack the nervous system, causing neurotoxicity.[4][7][14] The victim may present with strange disturbances to their vision, including blurriness. Paresthesia throughout the body, as well as difficulty speaking and breathing, may be reported.[4] Nervous system problems will cause a huge array of symptoms, and those provided here are not exhaustive. If the victim is not treated immediately they may die from respiratory failure.
Venom emitted from some types of cobras, almost all vipers, some Australian elapids and some sea snakes causes necrosis of muscle tissue.[7] Muscle tissue will begin to die throughout the body, a condition known as rhabdomyolysis. Rhabdomyolysis can result in damage to the kidneys as a result of myoglobin accumulation in the renal tubules. This, coupled with hypotension, can lead to acute renal failure, and, if left untreated, eventually death.[7]
Pathophysiology
Since envenomation is completely voluntary, all venomous snakes are capable of biting without injecting venom into their victim. Snakes may deliver such a "dry bite" rather than waste their venom on a creature too large for them to eat.[15] However, the percentage of dry bites varies between species: 50% of bites from the normally timid coral snake do not result in envenomation, whereas only 25% of pitviper bites are dry.[4] Furthermore, some snake genera, such as rattlesnakes, significantly increase the amount of venom injected in defensive bites compared to predatory strikes.[16]
Some dry bites may also be the result of imprecise timing on the snake's part, as venom may be prematurely released before the fangs have penetrated the victim's flesh.[15] Even without venom, some snakes, particularly large constrictors such as those belonging to the Boidae and Pythonidae families, can deliver damaging bites; large specimens often cause severe lacerations as the victim or the snake itself pull away, causing the flesh to be torn by the needle-sharp recurved teeth embedded in the victim. While not as life-threatening as a bite from a venomous species, the bite can be at least temporarily debilitating and could lead to dangerous infections if improperly dealt with.
While most snakes must open their mouths before biting, African and Middle Eastern snakes belonging to the family Atractaspididae are able to fold their fangs to the side of their head without opening their mouth and jab at victims.[17]
Snake venom
Main articles: Snake venom and Snake toxinsIt has been suggested that snakes evolved the mechanisms necessary for venom formation and delivery sometime during the Miocene epoch.[18] During the mid-Tertiary, most snakes were large ambush predators belonging to the superfamily Henophidia, which use constriction to kill their prey. As open grasslands replaced forested areas in parts of the world, some snake families evolved to become smaller and thus more agile. However, subduing and killing prey became more difficult for the smaller snakes, leading to the evolution of snake venom.[18] Other research on Toxicofera, a hypothetical clade thought to be ancestral to most living reptiles, suggests an earlier time frame for the evolution of snake venom, possibly to the order of tens of millions of years, during the Late Cretaceous.[19]
Snake venom is produced in modified parotid glands normally responsible for secreting saliva. It is stored in structures called alveoli behind the animal's eyes, and ejected voluntarily through its hollow tubular fangs. Venom is composed of hundreds to thousands of different proteins and enzymes, all serving a variety of purposes, such as interfering with a prey's cardiac system or increasing tissue permeability so that venom is absorbed faster.
Venom in many snakes, such as pitvipers, affects virtually every organ system in the human body and can be a combination of many toxins, including cytotoxins, hemotoxins, neurotoxins, and myotoxins, allowing for an enormous variety of symptoms.[4][20] Earlier, the venom of a particular snake was considered to be one kind only i.e. either hemotoxic or neurotoxic, and this erroneous belief may still persist wherever the updated literature is hard to access. Although there is much known about the protein compositions of venoms from Asian and American snakes, comparatively little is known of Australian snakes.
The strength of venom differs markedly between species and even more so between families, as measured by LD50 in mice. Subcutaneous LD50 varies by over 140-fold within elapids and by more than 100-fold in vipers. The amount of venom produced also differs among species, with the Gaboon viper able to potentially deliver from 450–600mg of venom in a single bite, the most of any snake.[21] Opisthoglyphous colubrids have venom ranging from life-threatening (in the case of the boomslang) to barely noticeable (as in Tantilla).
Prevention
Sign at Sylvan Rodriguez Park in Houston, Texas warning of the presence of snakes.
Snakes are most likely to bite when they feel threatened, are startled, are provoked, or have no means of escape when cornered. Encountering a snake is always considered dangerous and it is recommended to leave the vicinity. There is no practical way to safely identify any snake species as appearances may vary dramatically.
Snakes are likely to approach residential areas when attracted by prey, such as rodents. Practising regular pest control can reduce the threat of snakes considerably. It is beneficial to know the species of snake that are common in local areas, or while travelling or hiking. Areas of the world such as Africa, Australia, the Neotropics, and southern Asia are inhabited by many highly dangerous species. Being wary of snake presence and ultimately avoiding it when known is strongly recommended.
When in the wilderness, treading heavily creates ground vibrations and noise, which will often cause snakes to flee from the area. However, this generally only applies to North America as some larger and more aggressive snakes in other parts of the world, such as king cobras [22] and black mambas,[23] will protect their territories. When dealing with direct encounters it is best to remain silent and motionless. If the snake has not yet fled it is important to step away slowly and cautiously.
The use of a flashlight when engaged in camping activities, such as gathering firewood at night, can be helpful. Snakes may also be unusually active during especially warm nights when ambient temperatures exceed 21 °C (70 °F). It is advised not to reach blindly into hollow logs, flip over large rocks, and enter old cabins or other potential snake hiding-places. When rock climbing, it is not safe to grab ledges or crevices without examining them first, as snakes are cold-blooded and often sunbathe atop rock ledges.
Pet owners of domestic animals or snakes should be aware that a snake is capable of causing injury and that it is necessary to always act with caution. When handling snakes it is never wise to consume alcoholic beverages. In the United States more than 40% of snakebite victims intentionally put themselves in harm's way by attempting to capture wild snakes or by carelessly handling their dangerous pets—40% of that number had a blood alcohol level of 0.1 percent or more.[24]
It is also important to avoid snakes that appear to be dead, as some species will actually roll over on their backs and stick out their tongue to fool potential threats. A snake's detached head can immediately act by reflex and potentially bite. The induced bite can be just as severe as that of a live snake.[4][25] Dead snakes are also incapable of regulating the venom they inject, so a bite from a dead snake can often contain large amounts of venom.[26]
Treatment
It is not an easy task determining whether or not a bite by any species of snake is life-threatening. A bite by a North American copperhead on the ankle is usually a moderate injury to a healthy adult, but a bite to a child's abdomen or face by the same snake may be fatal. The outcome of all snakebites depends on a multitude of factors: the size, physical condition, and temperature of the snake, the age and physical condition of the victim, the area and tissue bitten (e.g., foot, torso, vein or muscle), the amount of venom injected, the time it takes for the person to find treatment, and finally the quality of that treatment.[4][27]
Snake identification
Identification of the snake is important in planning treatment in certain areas of the world, but is not always possible. Ideally the dead snake would be brought in with the person, but in areas where snake bite is more common, local knowledge may be sufficient to recognize the snake. However, in regions where polyvalent antivenoms are available, such as North America, identification of snake is not a high priority item. Attempting to catch or kill the offending snake also puts one at risk for re-envenomation or creating a second victim, and generally is not recommended.
The three types of venomous snakes that cause the majority of major clinical problems are vipers, kraits, and cobras. Knowledge of what species are present locally can be crucial, as is knowledge of typical signs and symptoms of envenomation by each type of snake. A scoring systems can be used to try and determine the biting snake based on clinical features,[28] but these scoring systems are extremely specific to particular geographical areas.
First aid
Snakebite first aid recommendations vary, in part because different snakes have different types of venom. Some have little local effect, but life-threatening systemic effects, in which case containing the venom in the region of the bite by pressure immobilization is desirable. Other venoms instigate localized tissue damage around the bitten area, and immobilization may increase the severity of the damage in this area, but also reduce the total area affected; whether this trade-off is desirable remains a point of controversy. Because snakes vary from one country to another, first aid methods also vary.
However, most first aid guidelines agree on the following:
- Protect the person and others from further bites. While identifying the species is desirable in certain regions, risking further bites or delaying proper medical treatment by attempting to capture or kill the snake is not recommended.
- Keep the person calm. Acute stress reaction increases blood flow and endangers the person. Panic is infectious and compromises judgment.
- Call for help to arrange for transport to the nearest hospital emergency room, where antivenom for snakes common to the area will often be available.
- Make sure to keep the bitten limb in a functional position and below the victim's heart level so as to minimize blood returning to the heart and other organs of the body.
- Do not give the person anything to eat or drink. This is especially important with consumable alcohol, a known vasodilator which will speed up the absorption of venom. Do not administer stimulants or pain medications to the victim, unless specifically directed to do so by a physician.
- Remove any items or clothing which may constrict the bitten limb if it swells (rings, bracelets, watches, footwear, etc.)
- Keep the person as still as possible.
- Do not incise the bitten site.
Many organizations, including the American Medical Association and American Red Cross, recommend washing the bite with soap and water. Australian recommendations for snake bite treatment recommend against cleaning the wound. Traces of venom left on the skin/bandages from the strike can be used in combination with a snake bite identification kit to identify the species of snake. This speeds determination of which antivenom to administer in the emergency room.[29]
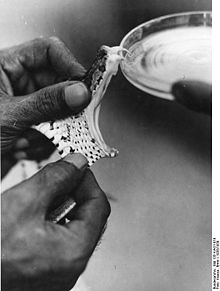
Pressure immobilization
In 1979, Australia's National Health and Medical Research Council formally adopted pressure immobilization as the preferred method of first aid treatment for snakebites in Australia.[30] As of 2009, clinical evidence for pressure immobilization remains limited, with current evidence based almost entirely on anecdotal case reports.[30] This has led most international authorities to question its efficacy.[30] Despite this, all reputable first aid organizations in Australia recommend pressure immobilization treatment; however, it is not widely adhered to, with one study showing that only a third of snakebite people attempt pressure immobilization.[30]
Pressure immobilization is not appropriate for cytotoxic bites such as those inflicted by most vipers,[31][32][33] but may be effective against neurotoxic venoms such as those of most elapids.[34][35][36] Developed by medical researcher Struan Sutherland in 1978,[37] the object of pressure immobilization is to contain venom within a bitten limb and prevent it from moving through the lymphatic system to the vital organs. This therapy has two components: pressure to prevent lymphatic drainage, and immobilization of the bitten limb to prevent the pumping action of the skeletal muscles.
Pressure is preferably applied with an elastic bandage, but any cloth will do in an emergency. Bandaging begins two to four inches above the bite (i.e. between the bite and the heart), winding around in overlapping turns and moving up towards the heart, then back down over the bite and past it towards the hand or foot. Then the limb must be held immobile: not used, and if possible held with a splint or sling. The bandage should be about as tight as when strapping a sprained ankle. It must not cut off blood flow, or even be uncomfortable; if it is uncomfortable, the person will unconsciously flex the limb, defeating the immobilization portion of the therapy. The location of the bite should be clearly marked on the outside of the bandages. Some peripheral edema is an expected consequence of this process.
Apply pressure immobilization as quickly as possible; if you wait until symptoms become noticeable you will have missed the best time for treatment. Once a pressure bandage has been applied, it should not be removed until the person has reached a medical professional. The combination of pressure and immobilization may contain venom so effectively that no symptoms are visible for more than 24 hours, giving the illusion of a dry bite.[citation needed] But this is only a delay; removing the bandage releases that venom into the person's system with rapid and possibly fatal consequences.
Antivenom
Until the advent of antivenom, bites from some species of snake were almost universally fatal.[38] Despite huge advances in emergency therapy, antivenom is often still the only effective treatment for envenomation. The first antivenom was developed in 1895 by French physician Albert Calmette for the treatment of Indian cobra bites. Antivenom is made by injecting a small amount of venom into an animal (usually a horse or sheep) to initiate an immune system response. The resulting antibodies are then harvested from the animal's blood.
Antivenom is injected into the person intravenously, and works by binding to and neutralizing venom enzymes. It cannot undo damage already caused by venom, so antivenom treatment should be sought as soon as possible. Modern antivenoms are usually polyvalent, making them effective against the venom of numerous snake species. Pharmaceutical companies which produce antivenom target their products against the species native to a particular area. Although some people may develop serious adverse reactions to antivenom, such as anaphylaxis, in emergency situations this is usually treatable and hence the benefit outweighs the potential consequences of not using antivenom.
Outmoded treatments
The following treatments have all been recommended at one time or another, but are now considered to be ineffective or outright dangerous. Many cases in which such treatments appear to work are in fact the result of dry bites.
- Application of a tourniquet to the bitten limb is generally not recommended. There is no convincing evidence that it is an effective first aid tool as ordinarily applied.[39] Tourniquets have been found to be completely ineffective in the treatment of Crotalus durissus bites,[40] but some positive results have been seen with properly applied tourniquets for cobra venom in the Philippines.[41] Uninformed tourniquet use is dangerous, since reducing or cutting off circulation can lead to gangrene, which can be fatal.[39] The use of a compression bandage is generally as effective, and much safer.
- Cutting open the bitten area, an action often taken prior to suction, is not recommended since it causes further damage and increases the risk of infection.
- Sucking out venom, either by mouth or with a pump, does not work and may harm the affected area directly.[42] Suction started after 3 minutes removes a clinically insignificant quantity—less than one thousandth of the venom injected—as shown in a human study.[43] In a study with pigs, suction not only caused no improvement but led to necrosis in the suctioned area.[44] Suctioning by mouth presents a risk of further poisoning through the mouth's mucous tissues.[45] The well-meaning family member or friend may also release bacteria into the victim's wound, leading to infection.
- Immersion in warm water or sour milk, followed by the application of snake-stones (also known as la Pierre Noire), which are believed to draw off the poison in much the way a sponge soaks up water.
- Application of potassium permanganate.
- Use of electroshock therapy. Although still advocated by some, animal testing has shown this treatment to be useless and potentially dangerous.[46][47][48][49]
In extreme cases, where the victims were in remote areas, all of these misguided attempts at treatment have resulted in injuries far worse than an otherwise mild to moderate snakebite. In worst case scenarios, thoroughly constricting tourniquets have been applied to bitten limbs, completely shutting off blood flow to the area. By the time the victims finally reached appropriate medical facilities their limbs had to be amputated.
Epidemiology
See also: List of fatal snake bites in the United States and List of fatal snake bites in AustraliaMost snakebites are caused by non-venomous snakes. Of the roughly 3,000 known species of snake found worldwide, only 15 percent are considered dangerous to humans.[1][4][50] Snakes are found on every continent except Antarctica.[1] The most diverse and widely distributed snake family, the colubrids, has approximately 700 venomous species,[51] but only five genera—boomslangs, twig snakes, keelback snakes, green snakes, and slender snakes—have caused human fatalities.[51]
Since reporting is not mandatory in many regions of the world,[1] snakebites often go unreported. Consequently, no accurate study has ever been conducted to determine the frequency of snakebites on the international level. However, some estimates put the number at 5.4 million snakebites, 2.5 million envenomings, resulting in perhaps 125,000 deaths.[1] Others estimate 1.2 to 5.5 million snakebites, 421,000 to 1.8 million envenomings, and 20,000 to 94,000 deaths.[1] Many people who survive bites nevertheless suffer from permanent tissue damage caused by venom, leading to disability.[7]
Most snake envenomings and fatalities occur in South Asia, Southeast Asia, and sub-Saharan Africa, with India reporting the most snakebite deaths of any country.[1] In India almost all of these deaths are caused by the Big Four, consisting of the Russell's viper, Indian cobra, saw-scaled viper, and the common krait. In Burma 80 percent of the approximately 1000 deaths each year from snake bite are caused by the Russell's Viper. Tea plantations sometimes are associated with some elapids such as the common cobras and the king cobra.
In the Neotropics, the lance-headed vipers inflict the majority of fatal bites, although of the many known species, only two, the common lancehead and terciopelo, are responsible for most cases.[7][52] The tropical rattlesnake is another important species.
In Africa, the puff adder is responsible for most fatalities,[53] although there are regional differences, with the saw-scaled viper inflicting more bites in Northern Africa, where the puff adder is not normally found.[52] Most bites occur in industrial plantations, which attract many types of snake prey. Banana plantations are associated with vipers such as night adders, while rubber and palm tree plantations attract elapids, including cobras and black mambas.[6] There are also highly venomous colubrids in Africa, such as the boomslang.
In the Middle East, the snakes responsible for most bites tend to be more venomous than European species, but deaths are rare, with some estimating perhaps 100 fatal bites annually.[6] The Palestine viper and Lebetine viper are the species involved in most bites.[6] Larger and more venomous elapids, such as the Egyptian cobra, can also be found throughout the Middle East.
In Europe, nearly all of the snakes responsible for venomous bites belong to the viper family, and of these, the coastal viper, nose-horned viper, asp viper, and Lataste's viper inflict the majority of bites.[6] Although Europe has a population of some 731 million people, snake bites only kill about 30 people each year, largely due to wide access to health care services and antivenom, as well as the relatively mild potency of many native species' venom.[6]
In Australia, the only continent where venomous snakes constitute the majority of species,[54] the Taipan, tiger snake and Eastern brown snake inflict virtually all reported venomous bites,[6][54] with the latter responsible for perhaps 60% of deaths caused by snakebite.[54] Although Australian snakes are highly venomous, wide access to antivenom has made deaths exceedingly rare, with only a few fatalities each year.
Most of the Pacific Islands are free of terrestrial snakes;[6] however, sea snakes are common in the Indian Ocean and tropical Pacific Ocean, but are not found in the Atlantic Ocean or the Caribbean, Mediterranean or Red Seas.[14] While the majority of species live close to shorelines or coral reefs, the yellow-bellied sea snake can be found in the open ocean.[14] Over 50% of bites inflicted by sea snakes, which are generally not aggressive, occur when fishermen attempt to remove snakes which have become tangled in fishing nets.[14][55] Symptoms may appear in as little as 5 minutes or take 8 hours to develop, depending on the species and region of the body bitten.[14] Although sea snakes are highly venomous, about 80% of reported bites end up being dry.[14][56] The advent of antivenom and advances in emergency medicine have reduced fatalities to about 3% of snakebite cases.[14]
Of the 120 known indigenous snake species in North America, only 20 are venomous to human beings, all belonging to the families Viperidae and Elapidae.[4] However, in the United States, every state except Maine, Alaska, and Hawaii is home to at least one of 20 venomous snake species.[4] Most snakebite related deaths in the United States are attributed to Eastern and Western diamondback rattlesnake bites.[4] Further, the majority of bites in the United States occur in the southwestern part of the country, in part because rattlesnake populations in the eastern states are much lower.[57] The state of North Carolina has the highest frequency of reported snakebites, averaging approximately 19 bites per 100,000 persons.[20] The national average is roughly 4 bites per 100,000 persons.[20]
Worldwide, snakebites occur most frequently in the summer season when snakes are active and humans are outdoors.[1][58] Agricultural and tropical regions report more snakebites than anywhere else.[1][52] Victims are typically male and between 17 and 27 years of age.[4][58][59] Children and the elderly are the most likely to die.[4][27]
-
Bites by the European adder, which is widespread and found throughout much of Europe and Russia, are relatively common; however, fatalities are very rare.
-
Startled snakes often take a defensive posture, such as this cottonmouth, and may hiss and bare their fangs in a threatening manner.
-
The yellow-lipped sea krait is a timid but highly venomous sea snake common throughout Indo-Pacific oceanic waters.
Society and culture
See also: Serpent (symbolism) According to tradition, Cleopatra VII famously committed suicide by snakebite to her left breast, as seen in this 1911 painting by Hungarian artist Gyula Benczúr.
According to tradition, Cleopatra VII famously committed suicide by snakebite to her left breast, as seen in this 1911 painting by Hungarian artist Gyula Benczúr.
Snakes were both revered and worshipped and feared by early civilizations. The ancient Egyptians recorded prescribed treatments for snakebites as early as the Thirteenth dynasty in the Brooklyn Papyrus, which includes at least seven venomous species common to the region today, such as the horned vipers.[60] In Judaism, the Nehushtan was a pole with a snake made of copper wrapped around it, similar in appearance to the Rod of Asclepius. The object was considered sacred with the power to heal bites caused by the snakes which had infested the desert, with victims merely having to touch it in order to save themselves from imminent death.
Historically, snakebites were seen as a means of execution in some cultures. In medieval Europe, a form of capital punishment was to throw people into snake pits, leaving victims to die from multiple venomous bites. A similar form of punishment was common in Southern Han during China's Five Dynasties and Ten Kingdoms Period and in India.[61] Snakebites were also used as a form of suicide, most notably by Egyptian queen Cleopatra VII, who reportedly died from the bite of an asp—likely an Egyptian cobra[60][62]—after hearing of Mark Antony's death.
Snakebite as a surreptitious form of murder has been featured in stories such as Sir Arthur Conan Doyle's The Adventure of the Speckled Band, but actual occurrences are virtually unheard of, with only a few documented cases.[61][63][64] It has been suggested that Boris III of Bulgaria, who was allied to Nazi Germany during World War II, may have been killed with snake venom,[61] although there is no definitive evidence. At least one attempted suicide by snakebite has been documented in medical literature involving a puff adder bite to the hand.[65]
Footnotes
- ^ a b c d e f g h i j k l Kasturiratne, A.; Wickremasinghe A. R., de Silva N., Gunawardena N. K., Pathmeswaran A., et al. (2008). "The Global Burden of Snakebite: A Literature Analysis and Modelling Based on Regional Estimates of Envenoming and Deaths". PloS Medicine 5 (11): e218. doi:10.1371/journal.pmed.0050218. PMC 2577696. PMID 18986210. http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.0050218;jsessionid=66B81B3E56F5DABADB52D86E51BE334F. Retrieved 2009-06-24.
- ^ Snake Venom Detection Kit: Detection and Identification of Snake Venom. CSL Limited. 2007. http://www.csl.com.au/docs/92/398/SVDK_Product_Leaflet.pdf. Retrieved 2009-11-24. "The physical identification of Australian and Papua New Guinean snakes is notoriously unreliable. There is often marked colour variation between juvenile and adult snakes and wide size, shape and colour variation between snakes of the same species. Reliable snake identification requires expert knowledge of snake anatomy, a snake key and the physical handling of the snake"[dead link]
- ^ White, Julian (2006). Snakebite & Spiderbite: Management Guidelines. Adelaide: Department of Health, Government of South Australia. pp. 1–71. ISBN 0730895513. http://www.health.sa.gov.au/DesktopModules/SSSA_Documents/LinkClick.aspx?tabid=57&mid=403&table=SSSA_Documents&field=ItemID&id=257&link=C%3A%5CDocuments+and+Settings%5Cdhc000033%5CDesktop%5CA+HEAT+(Store)%5CSA+Snakebite+Guide+screenres.pdf. Retrieved 2009-11-24. "The colour of brown snakes is very variable and misleading for identification purposes. They may be brown, red brown, grey, very dark brown and may be plain in color, have speckling, stripes or bands, or have a dark or black head"
- ^ a b c d e f g h i j k l m n o p q r s Gold, Barry S.; Richard C. Dart, Robert A. Barish (1 April 2002). "Bites of venomous snakes". The New England Journal of Medicine 347 (5): 347–56. doi:10.1056/NEJMra013477. ISSN 00284793. PMID 12151473. http://content.nejm.org/cgi/content/full/347/5/347?ijkey=/Romzox5/Yq3A&keytype=ref&siteid=nejm. Retrieved 2009-06-25.
- ^ a b Kitchens C, Van Mierop L (1987). "Envenomation by the Eastern coral snake (Micrurus fulvius fulvius). A study of 39 victims". JAMA 258 (12): 1615–18. doi:10.1001/jama.258.12.1615. PMID 3625968.
- ^ a b c d e f g h i Chippaux, J.P. (1998). "Snake-bites: appraisal of the global situation". Bulletin of the World Health Organization 76 (5): 515–24. PMC 2305789. PMID 9868843. http://www.kingsnake.com/aho/pdf/menu6/chippaux1998.pdf. Retrieved 2009-07-03.
- ^ a b c d e f g h i j k Gutiérrez, José María; Bruno Lomonte, Guillermo León, Alexandra Rucavado, Fernando Chaves, Yamileth Angulo (2007). "Trends in Snakebite Envenomation Therapy: Scientific, Technological and Public Health Considerations". Current Pharmaceutical Design 13 (28): 2935–50. doi:10.2174/138161207782023784. PMID 17979738. http://www.icp.ucr.ac.cr/~blomonte/2007_Antivenenos_CurrPharmDesign_Gutierrez_therapy_review.pdf. Retrieved 2009-07-01.
- ^ a b MedlinePlus > Snake bites From Tintinalli JE, Kelen GD, Stapcynski JS, eds. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York, NY: McGraw Hill; 2004. Update Date: 2/27/2008. Updated by: Stephen C. Acosta, MD, Department of Emergency Medicine, Portland VA Medical Center, Portland, OR. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. Retrieved on 19 mars, 2009
- ^ Health-care-clinic.org > Snake Bite First Aid - Snakebite Retrieved on 21 mars, 2009
- ^ Snake bite image example at MDconsult > Patient Education > Wounds, Cuts and Punctures, First Aid for
- ^ http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0030150
- ^ Warrell, David A.; L. David Ormerod (1976). "Snake Venom Ophthalmia and Blindness Caused by the Spitting Cobra (Naja Nigricollis) in Nigeria". The American Society of Tropical Medicine and Hygiene 25 (3): 525–9. PMID 1084700. http://www.ajtmh.org/cgi/content/abstract/25/3/525. Retrieved 2009-09-05.
- ^ Ismail, Mohammad; Abdullah M. Al-Bekairi, Ayman M. El-Bedaiwy, Mohammad A. Abd-El Salam (1993). "The ocular effects of spitting cobras: I. The ringhals cobra (Hemachatus haemachatus) Venom-Induced corneal opacification syndrome". Clinical Toxicology 31 (1): 31–41. doi:10.3109/15563659309000372. PMID 8433414.
- ^ a b c d e f g Phillips, Charles M. (2002). "Sea snake envenomation". Dermatologic Therapy 15 (1): 58–61(4). doi:10.1046/j.1529-8019.2002.01504.x. http://www.kingsnake.com/aho/pdf/menu6/phillips2002.pdf. Retrieved 2009-07-24.
- ^ a b Young, Bruce A.; Cynthia E. Lee, Kylle M. Daley (2002). "Do Snakes Meter Venom?". BioScience 52 (12): 1121–26. doi:10.1641/0006-3568(2002)052[1121:DSMV]2.0.CO;2. http://caliber.ucpress.net/doi/abs/10.1641/0006-3568(2002)052%5B1121:DSMV%5D2.0.CO%3B2. Retrieved 2009-09-18. "The second major assumption that underlies venom metering is the snake's ability to accurately assess the target"
- ^ Young, Bruce A.; Krista Zahn (2001). "Venom flow in rattlesnakes: mechanics and metering". Journal of Experimental Biology 204 (Pt 24): 4345–4351. ISSN 0022-0949. PMID 11815658. http://jeb.biologists.org/cgi/reprint/204/24/4345.pdf. Retrieved 2009-09-18. "With the species and size of target held constant, the duration of venom flow, maximum venom flow rate and total venom volume were all significantly lower in predatory than in defensive strikes"
- ^ Deufel, Alexandra; David Cundall (2003). "Feeding in Atractaspis (Serpentes: Atractaspididae): a study in conflicting functional constraints". Zoology 106 (1): 43–61. doi:10.1078/0944-2006-00088. PMID 16351890. http://www.minotstateu.edu/biology/pdf/AtractaspisReprint.pdf. Retrieved 2009-08-25.
- ^ a b Jackson, Kate (2003). "The evolution of venom-delivery systems in snakes". Zoological Journal of the Linnean Society 137 (3): 337–354. doi:10.1046/j.1096-3642.2003.00052.x. http://www.kingsnake.com/aho/pdf/menu2/jackson2002.pdf. Retrieved 2009-07-25.
- ^ Fry, Bryan G.; Nicolas Vidal, Janette A. Norman, Freek J. Vonk, Holger Scheib, S. F. Ryan Ramjan, Sanjaya Kuruppu, Kim Fung, S. Blair Hedges, Michael K. Richardson, Wayne. C. Hodgson, Vera Ignjatovic, Robyn Summerhayes, Elazar Kochva (2006). "Early evolution of the venom system in lizards and snakes". Nature 439 (7076): 584–8. doi:10.1038/nature04328. PMID 16292255. http://www.venomdoc.com/downloads/2005_BGF_Nature_squamate_venom.pdf. Retrieved 2009-09-18.
- ^ a b c Russell, Findlay E. (1980). "Snake Venom Poisoning in the United States". Annual Review of Medicine 31: 247–59. doi:10.1146/annurev.me.31.020180.001335. PMID 6994610.
- ^ Spawls, Stephen; Bill Branch (1997). The Dangerous Snakes of Africa. Johannesburg: Southern Book Publishers. p. 192. ISBN 1868125750.
- ^ "National geographic- KING COBRA". http://animals.nationalgeographic.com/animals/reptiles/king-cobra/. "They are fiercely aggressive when cornered (line 28-29)"
- ^ "National geographic-BLACK MAMBA". http://animals.nationalgeographic.com/animals/reptiles/black-mamba.html. "when threatened, highly aggressive (line 2-3)"
- ^ Kurecki B, Brownlee H (1987). "Venomous snakebites in the United States". JournAL of Family Practice 25 (4): 386–92. PMID 3655676.
- ^ Gold B, Barish R (1992). "Venomous snakebites. Current concepts in diagnosis, treatment, and management". Emerg Med Clin North Am 10 (2): 249–67. PMID 1559468.
- ^ Suchard, JR; LoVecchio F. (1999). "Envenomations by Rattlesnakes Thought to Be Dead". The New England Journal of Medicine 340 (24): 1930. doi:10.1056/NEJM199906173402420. ISSN 0028-4793. PMID 10375322. http://content.nejm.org/cgi/content/extract/340/24/1930. Retrieved 2009-09-05.
- ^ a b Gold BS, Wingert WA (1994). "Snake venom poisoning in the United States: a review of therapeutic practice". South. Med. J. 87 (6): 579–89. doi:10.1097/00007611-199406000-00001. PMID 8202764.
- ^ Pathmeswaran A, Kasturiratne A, Fonseka M, Nandasena S, Lalloo D, de Silva H (2006). "Identifying the biting species in snakebite by clinical features: an epidemiological tool for community surveys". Trans R Soc Trop Med Hyg 100 (9): 874–8. doi:10.1016/j.trstmh.2005.10.003. PMID 16412486.
- ^ Chris Thompson. "Treatment of Australian Snake Bites". Australian anaesthetists' website. http://www.usyd.edu.au/anaes/venom/snakebite.html.
- ^ a b c d Currie, Bart J.; Elizabeth Canale, Geoffrey K. Isbister (2008). "Effectiveness of pressure-immobilization first aid for snakebite requires further study". Emergency Medicine Australasia 20 (3): 267–270(4). doi:10.1111/j.1742-6723.2008.01093.x. PMID 18549384.
- ^ Rogers I, Celenza T (2002). "Simulated field experience in the use of the Sam splint for pressure immobilization of snakebite". Wilderness Environ Med 13 (2): 184–5. PMID 12092977. http://www.wemjournal.org/wmsonline/?request=get-document&issn=1080-6032&volume=013&issue=02&page=0184.[dead link]
- ^ Bush S, Green S, Laack T, Hayes W, Cardwell M, Tanen D (2004). "Pressure immobilization delays mortality and increases intracompartmental pressure after artificial intramuscular rattlesnake envenomation in a porcine model" (PDF). Ann Emerg Med 44 (6): 599–604. doi:10.1016/j.annemergmed.2004.06.007. PMID 15573035. http://www.llu.edu/llu/faculty/whayes/documents/2004_bush_et_al._pressure-immob.pdf. Retrieved 2006-06-25.[dead link]
- ^ Sutherland S, Coulter A (1981). "Early management of bites by the eastern diamondback rattlesnake (Crotalus adamanteus): studies in monkeys (Macaca fascicularis)". Am J Trop Med Hyg 30 (2): 497–500. PMID 7235137.
- ^ Rogers I, Winkel K (2005). "Struan Sutherland's "Rationalisation of first-aid measures for elapid snakebite"--a commentary". Wilderness Environ Med 16 (3): 160–3. PMID 16209471. http://www.wemjournal.org/wmsonline/?request=get-document&issn=1080-6032&volume=016&issue=03&page=0160. Retrieved 2006-06-25.
- ^ Sutherland S (1992). "Deaths from snake bite in Australia, 1981-1991". Med J Aust 157 (11-12): 740–6. PMID 1453996.
- ^ Sutherland S, Leonard R (1995). "Snakebite deaths in Australia 1992-1994 and a management update". Med J Aust 163 (11-12): 616–8. PMID 8538559.
- ^ Sutherland S, Coulter A, Harris R (1979). "Rationalisation of first-aid measures for elapid snakebite". Lancet 1 (8109): 183–5. doi:10.1016/S0140-6736(79)90580-4. PMID 84206. http://www.wemjournal.org/wmsonline/?request=get-document&issn=1080-6032&volume=016&issue=03&page=0164.[dead link]
- ^ White, Julian (November 1991). "Oxyuranus microlepidotus". Chemical Safety Information from Intergovernmental Organizations. http://www.inchem.org/documents/pims/animal/taipan.htm. Retrieved 24 July 2009. "Without appropriate antivenom treatment up to 75% of taipan bites will be fatal. Indeed, in the era prior to specific antivenom therapy, virtually no survivors of taipan bite were recorded."
- ^ a b Theakston RD (1997). "An objective approach to antivenom therapy and assessment of first-aid measures in snake bite" (PDF). Ann. Trop. Med. Parasitol. 91 (7): 857–65. doi:10.1080/00034989760626. PMID 9625943. http://www.kingsnake.com/aho/pdf/menu6/theakston1997.pdf.
- ^ Amaral CF, Campolina D, Dias MB, Bueno CM, Rezende NA (1998). "Tourniquet ineffectiveness to reduce the severity of envenoming after Crotalus durissus snake bite in Belo Horizonte, Minas Gerais, Brazil". Toxicon 36 (5): 805–8. doi:10.1016/S0041-0101(97)00132-3. PMID 9655642. http://linkinghub.elsevier.com/retrieve/pii/S0041-0101(97)00132-3.
- ^ Watt G, Padre L, Tuazon ML, Theakston RD, Laughlin LW (1988). "Tourniquet application after cobra bite: delay in the onset of neurotoxicity and the dangers of sudden release". Am. J. Trop. Med. Hyg. 38 (3): 618–22. PMID 3275141.
- ^ Holstege CP, Singletary EM (2006). "Images in emergency medicine. Skin damage following application of suction device for snakebite". Annals of emergency medicine 48 (1): 105, 113. doi:10.1016/j.annemergmed.2005.12.019. PMID 16781926.
- ^ Alberts M, Shalit M, LoGalbo F (2004). "Suction for venomous snakebite: a study of "mock venom" extraction in a human model". Ann Emerg Med 43 (2): 181–6. doi:10.1016/S0196-0644(03)00813-8. PMID 14747805.
- ^ Bush SP, Hegewald KG, Green SM, Cardwell MD, Hayes WK (2000). "Effects of a negative pressure venom extraction device (Extractor) on local tissue injury after artificial rattlesnake envenomation in a porcine model". Wilderness & environmental medicine 11 (3): 180–8. PMID 11055564.
- ^ Riggs BS, Smilkstein MJ, Kulig KW, et al. Rattlesnake envenomation with massive oropharyngeal edema following incision and suction (Abstract). Presented at the AACT/AAPCC/ABMT/CAPCC Annual Scientific Meeting, Vancouver, Canada, September 27 October 2, 1987.
- ^ Russell F (1987). "Another warning about electric shock for snakebite". Postgrad Med 82 (5): 32. PMID 3671201.
- ^ Ryan A (1987). "Don't use electric shock for snakebite". Postgrad Med 82 (2): 42. PMID 3497394.
- ^ Howe N, Meisenheimer J (1988). "Electric shock does not save snakebitten rats". Ann Emerg Med 17 (3): 254–6. doi:10.1016/S0196-0644(88)80118-5. PMID 3257850.
- ^ Johnson E, Kardong K, Mackessy S (1987). "Electric shocks are ineffective in treatment of lethal effects of rattlesnake envenomation in mice". Toxicon 25 (12): 1347–9. doi:10.1016/0041-0101(87)90013-4. PMID 3438923.
- ^ Russell, F. E. (1990). "When a snake strikes". Emerg Med 22 (12): 33–4, 37–40, 43.
- ^ a b Mackessy, Stephen P. (2002). "Biochemistry and pharmacology of colubrid snake venoms". Journal of Toxicology: Toxin Reviews 21 (1–2): 43–83. doi:10.1081/TXR-120004741. http://www.unco.edu/nhs/biology/faculty_staff/mackessy/colubrid.pdf. Retrieved 2009-09-26. "Estimates of the number of venomous colubrids approach 700 species. Most may not produce a venom capable of causing serious damage to humans, but at least five species (Dispholidus typus, Thelotornis capensis, Rhabdophis tigrinus, Philodryas olfersii and Tachymenis peruviana) have caused human fatalities"
- ^ a b c Gutiérrez, José María; R. David G. Theakston, David A. Warrell (6 June 2006). "Confronting the Neglected Problem of Snake Bite Envenoming: The Need for a Global Partnership". PLoS Medicine 3 (6): e150. doi:10.1371/journal.pmed.0030150. PMC 1472552. PMID 16729843. http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.0030150. Retrieved 2009-06-30.
- ^ Mallow, David; David Ludwig, Goran Nilson (2004). True Vipers: Natural History and Toxinology of Old World Vipers. Malabar, FL: Krieger Publishing Company. ISBN 0894648772.
- ^ a b c Mirtschin, P.J.; R. Shineb, T.J. Niasa, N.L. Dunstana, B.J. Hougha, M. Mirtschina (2002). "Influences on venom yield in Australian tigersnakes (Notechis scutatus) and brownsnakes (Pseudonaja textilis: Elapidae, Serpentes)". Toxicon 40 (11): 1581–92. doi:10.1016/S0041-0101(02)00175-7. PMID 12419509. http://www.kingsnake.com/aho/pdf/menu5/mirtschin2002.pdf. Retrieved 2009-07-03.
- ^ Thomas, Craig; Susan Scott (1997). All Stings Considered: First Aid and Medical Treatment of Hawaii's Marine Injuries. Honolulu, HI: University of Hawaii Press. pp. 72–76. ISBN 0824819004.
- ^ Tu, AG; Fulde GE (1987). "Sea snake bites". Clinics in Dermatology 5 (3): 118–26. doi:10.1016/S0738-081X(87)80018-4. ISSN 0738-081X. PMID 3311337.
- ^ Russell, Findlay E (1983). Snake Venom Poisoning. Great Neck, NY: Scholium International. p. 163. ISBN 0-87936-015-1.
- ^ a b Wingert W, Chan L (1 January 1988). "Rattlesnake bites in southern California and rationale for recommended treatment". West J Med 148 (1): 37–44. PMC 1026007. PMID 3277335. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1026007. Retrieved 2006-05-26.
- ^ Parrish H (1966). "Incidence of treated snakebites in the United States". Public Health Rep 81 (3): 269–76. PMC 1919692. PMID 4956000. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1919692.
- ^ a b Schneemann, M.; R. Cathomas, S.T. Laidlaw, A.M. El Nahas, R.D.G. Theakston, and D.A. Warrell (2004). "Life-threatening envenoming by the Saharan horned viper (Cerastes cerastes) causing micro-angiopathic haemolysis, coagulopathy and acute renal failure: clinical cases and review". QJM: an International Journal of Medicine 97 (11): 717–27. doi:10.1093/qjmed/hch118. PMID 15496528. http://qjmed.oxfordjournals.org/cgi/reprint/97/11/717.pdf. Retrieved 2009-09-04. "This echoed the opinion of the Egyptian physicians who wrote the earliest known account of the treatment of snake bite, the Brooklyn Museum Papyri, dating perhaps from 2200 BC. They regarded bites by horned vipers 'fy' as non-lethal, as the victims could be saved."
- ^ a b c Anil, Aggrawal (2004). "Homicide with snakes: A distinct possibility and its medicolegal ramifications". Anil Aggrawal's Internet Journal of Forensic Medicine and Toxicology 4 (2). ISSN 0972-8074. http://geradts.com/anil/ij/vol_004_no_002/others/pg001.html. Retrieved 2009-09-04.
- ^ Crawford, Amy (April 1, 2007). "Who Was Cleopatra? Mythology, propaganda, Liz Taylor and the real Queen of the Nile". Smithsonian.com. http://www.smithsonianmag.com/history-archaeology/biography/cleopatra.html. Retrieved 4 September 2009.
- ^ Warrell, D.A. (2009). "Commissioned article: management of exotic snakebites". QJM: an International Journal of Medicine 102 (9): 593–601. doi:10.1093/qjmed/hcp075. ISSN 1460-2393. PMID 19535618.
- ^ Straight, Richard C.; James L. Glenn (1994). "Human fatalities caused by venomous animals in Utah, 1900-90". Great Basin Naturalist 53 (4): 390–4. https://ojs.lib.byu.edu/ojs/index.php/wnan/article/viewFile/545/1430. Retrieved 2009-09-04. "A third unusual death was a tragic fatality (1987), recorded as a homicide, which resulted when a large rattlesnake (G. v. lutosus) bit a 22-month-old girl after the snake had been placed around her neck (Washington County). The child died in approximately 5 h."
- ^ Strubel, T.; A. Birkhofer, F. Eyer, K.D. Werber, H. Förstl (2008). "Suizidversuch durch Schlangenbiss: Kasuistik und Literaturübersicht [Attempted suicide by snake bite: Case report and literature survey]" (in German). Der Nervenarzt 79 (5): 604–6. doi:10.1007/s00115-008-2431-4. ISSN 1433-0407. PMID 18365165. "Ein etwa 20-jähriger Arbeiter wurde nach dem Biss seiner Puffotter (Bitis arietans) in die Hand auf die toxikologische Intensivstation aufgenommen. Zunächst berichtet der Patient, dass es beim „Melken“ der Giftschlange zu dem Biss gekommen sei, erst im weiteren Verlauf räumt er einen Suizidversuch ein. Als Gründe werden Einsamkeit angeführt sowie unerträgliche Schmerzen im Penis."
References
- Campbell, Jonathan A.; William W. Lamar (2004). The Venomous Reptiles of the Western Hemisphere, Ithaca, NY: Cornell University Press.
- Spawls, Stephen; Bill Branch (1995). The Dangerous Snakes of Africa: Natural History - Species Directory - Venoms and Snakebite, Sanibel Island, FL: Ralph Curtis Publishing.
- Sullivan JB, Wingert WA, Norris Jr RL. North American Venomous Reptile Bites. Wilderness Medicine: Management of Wilderness and Environmental Emergencies, 1995; 3: 680–709.
- Thorpe, Roger S.; Wolfgang Wuster, Anita Malhotra (1996). Venomous Snakes: Ecology, Evolution, and Snakebite, Oxford, England: Oxford University Press.
External links
General wounds and injuries (T08-T35, 870-949) General Wound/
traumaBlister (Blood blister • Coma blister • Delayed blister • Edema blister • Fracture blister • Friction blister • Sucking blister)
Bruise/Hematoma/Ecchymosis (Battle's sign, Raccoon eyes, Black eye, Subungual hematoma, Cullen's sign, Grey Turner's sign, Retroperitoneal hemorrhage)
Animal bite: Insect bite · Spider biteAnimal bite: Snakebite · Lizard bite
Ballistic traumaForeign body In alimentary tract (Bezoar)Other By region Poisonings, toxicities, and overdoses (T36–T65, 960–989) (history) Inorganic Organic CHOPharmaceuticals cardiovascular systemBiological
(including venom,
toxin,
food poisoning)Fish/seafoodOther vertebratesList of biting or stinging arthropods: bee sting/bee venom (Apamin, Melittin) · spider venom (Latrotoxin/Latrodectism, Loxoscelism) · scorpion venom (Charybdotoxin)Animal bites and stings (X20, E900-E909) Animal bites and stings Arthropod bites and stings: Arachnid (Scorpion sting, Spider bite/Arachnidism) · Insect bites and stings (Pulicosis, Reduviid bite, Cimicosis, Ant sting, Bee sting) · Myriapoda (Centipede bite, Millipede burn)
Vertebrate: Dog bite · Snakebite · Lizard bite · Stingray injury · Stonefish sting · Shark attack · Crocodile attack · Bear attack · Wolf attack · Tiger attack · Cougar attack · Dingo attack · Killer whale attack
Other: Jellyfish sting/Jellyfish dermatitis (Coral dermatitis, Hydroid dermatitis, Portuguese man-of-war dermatitis, Sea anemone dermatitis, Seabather's eruption)Categories:- Parasitic infestations, stings, and bites of the skin
- Animal attacks
- Venomous animals
- Medical emergencies
- Venomous snakes
- Wilderness medical emergencies
Wikimedia Foundation. 2010.