- Hepatitis
-
Hepatitis Classification and external resources 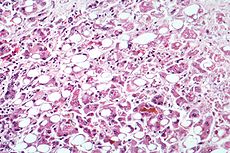
Alcoholic hepatitis evident by fatty change, cell necrosis, Mallory bodiesICD-10 K75.9 ICD-9 573.3 DiseasesDB 20061 MeSH D006505 Hepatitis (plural hepatitides) is a medical condition defined by the inflammation of the liver and characterized by the presence of inflammatory cells in the tissue of the organ. The name is from the Greek hepar (ἧπαρ), the root being hepat- (ἡπατ-), meaning liver, and suffix -itis, meaning "inflammation" (c. 1727).[1] The condition can be self-limiting (healing on its own) or can progress to fibrosis (scarring) and cirrhosis.
Hepatitis may occur with limited or no symptoms, but often leads to jaundice, anorexia (poor appetite) and malaise. Hepatitis is acute when it lasts less than six months and chronic when it persists longer. A group of viruses known as the hepatitis viruses cause most cases of hepatitis worldwide, but it can also be due to toxins (notably alcohol, certain medications, some industrial organic solvents and plants), other infections and autoimmune diseases.
Contents
Signs and symptoms
Acute
Initial features are of nonspecific flu-like symptoms, common to almost all acute viral infections and may include malaise, muscle and joint aches, fever, nausea or vomiting, diarrhea, and headache. More specific symptoms, which can be present in acute hepatitis from any cause, are: profound loss of appetite, aversion to smoking among smokers, dark urine, yellowing of the eyes and skin (i.e., jaundice) and abdominal discomfort. Physical findings are usually minimal, apart from jaundice in a third and tender hepatomegaly (swelling of the liver) in about 10%. Some exhibit lymphadenopathy (enlarged lymph nodes, in 5%) or splenomegaly (enlargement of the spleen, in 5%).[2]
Acute viral hepatitis is more likely to be asymptomatic in younger people. Symptomatic individuals may present after convalescent stage of 7 to 10 days, with the total illness lasting 2 to 6 weeks.[3]
A small proportion of people with acute hepatitis progress to acute liver failure, in which the liver is unable to clear harmful substances from the circulation (leading to confusion and coma due to hepatic encephalopathy) and produce blood proteins (leading to peripheral edema and bleeding). This may become life-threatening and occasionally requires a liver transplant.
Chronic
Chronic hepatitis often leads to nonspecific symptoms such as malaise, tiredness and weakness, and often leads to no symptoms at all. It is commonly identified on blood tests performed either for screening or to evaluate nonspecific symptoms. The occurrence of jaundice indicates advanced liver damage. On physical examination there may be enlargement of the liver.[4]
Extensive damage and scarring of liver (i.e. cirrhosis) leads to weight loss, easy bruising and bleeding tendencies, peripheral edema (swelling of the legs) and accumulation of ascites (fluid in the abdominal cavity). Eventually, cirrhosis may lead to various complications: esophageal varices (enlarged veins in the wall of the esophagus that can cause life-threatening bleeding) hepatic encephalopathy (confusion and coma) and hepatorenal syndrome (kidney dysfunction).
Acne, abnormal menstruation, lung scarring, inflammation of the thyroid gland and kidneys may be present in women with autoimmune hepatitis.[4]
Causes
Acute
- Viral hepatitis:
- Hepatitis A, B, C, D, and E.
- Yellow fever
- KIs-V
- adenoviruses
- Non-viral infection
- toxoplasma
- Leptospira
- Q fever[5]
- rocky mountain spotted fever[6]
- Alcohol
- Toxins: Amanita toxin in mushrooms, carbon tetrachloride, asafetida
- Drugs: Paracetamol, amoxycillin, antituberculosis medicines, minocycline and many others (see longer list below).
- Ischemic hepatitis (circulatory insufficiency)
- Pregnancy
- Auto immune conditions, e.g., Systemic Lupus Erythematosus (SLE)
- Metabolic diseases, e.g., Wilson's disease
Chronic
- Viral hepatitis: Hepatitis B with or without hepatitis D, hepatitis C (neither hepatitis A nor hepatitis E causes chronic hepatitis)
- Autoimmune
- Alcohol
- Drugs
- Non-alcoholic steatohepatitis
- Heredity
- Primary biliary cirrhosis and primary sclerosing cholangitis occasionally mimic chronic hepatitis[3]
Alcoholic hepatitis
Ethanol, mostly in alcoholic beverages, is a significant cause of hepatitis. Usually alcoholic hepatitis comes after a period of increased alcohol consumption. Alcoholic hepatitis is characterized by a variable constellation of symptoms, which may include feeling unwell, enlargement of the liver, development of fluid in the abdomen ascites, and modest elevation of liver blood tests. Alcoholic hepatitis can vary from mild with only liver test elevation to severe liver inflammation with development of jaundice, prolonged prothrombin time, and liver failure. Severe cases are characterized by either obtundation (dulled consciousness) or the combination of elevated bilirubin levels and prolonged prothrombin time; the mortality rate in both categories is 50% within 30 days of onset.
Alcoholic hepatitis is distinct from cirrhosis caused by long term alcohol consumption. Alcoholic hepatitis can occur in patients with chronic alcoholic liver disease and alcoholic cirrhosis. Alcoholic hepatitis by itself does not lead to cirrhosis, but cirrhosis is more common in patients with long term alcohol consumption. Patients who drink alcohol to excess are also more often than others found to have hepatitis C.[citation needed] The combination of hepatitis C and alcohol consumption accelerates the development of cirrhosis.
Drug induced
A large number of drugs can cause hepatitis:[7]
- Agomelatine (antidepressant)
- Allopurinol
- Amitriptyline (antidepressant)
- Amiodarone (antiarrhythmic)
- Atomoxetine [8]
- Azathioprine[9]
- Halothane (a specific type of anesthetic gas)
- Hormonal contraceptives
- Ibuprofen and indomethacin (NSAIDs)
- Isoniazid (INH), rifampicin, and pyrazinamide (tuberculosis-specific antibiotics)
- Ketoconazole (antifungal)
- Loratadine (antihistamine)
- Methotrexate (immune suppressant)
- Methyldopa (antihypertensive)
- Minocycline (tetracycline antibiotic)
- Nifedipine (antihypertensive)
- Nitrofurantoin (antibiotic)
- Paracetamol (acetaminophen in the United States) can cause hepatitis when taken in an overdose. The severity of liver damage may be limited by prompt administration of acetylcysteine.
- Phenytoin and valproic acid (antiepileptics)
- Troglitazone (antidiabetic, withdrawn in 2000 for causing hepatitis)
- Zidovudine (antiretroviral i.e., against HIV)
- Some herbs and nutritional supplements[10]
The clinical course of drug-induced hepatitis is quite variable, depending on the drug and the patient's tendency to react to the drug. For example, halothane hepatitis can range from mild to fatal as can INH-induced hepatitis. Hormonal contraception can cause structural changes in the liver. Amiodarone hepatitis can be untreatable since the long half life of the drug (up to 60 days) means that there is no effective way to stop exposure to the drug. Statins can cause elevations of liver function blood tests normally without indicating an underlying hepatitis. Lastly, human variability is such that any drug can be a cause of hepatitis.
Other toxins
Other Toxins can cause hepatitis:
- Amatoxin-containing mushrooms, including the Death Cap (Amanita phalloides), the Destroying Angel (Amanita ocreata), and some species of Galerina. A portion of a single mushroom can be enough to be lethal (10 mg or less of α-amanitin).
- White phosphorus, an industrial toxin and war chemical.
- Carbon tetrachloride ("tetra", a dry cleaning agent), chloroform, and trichloroethylene, all chlorinated hydrocarbons, cause steatohepatitis (hepatitis with fatty liver).
- Cylindrospermopsin, a toxin from the cyanobacterium Cylindrospermopsis raciborskii and other cyanobacteria.
Metabolic disorders
Some metabolic disorders cause different forms of hepatitis. Hemochromatosis (due to iron accumulation) and Wilson's disease (copper accumulation) can cause liver inflammation and necrosis.
Non-alcoholic steatohepatitis (NASH) is effectively a consequence of metabolic syndrome.
Obstructive
"Obstructive jaundice" is the term used to describe jaundice due to obstruction of the bile duct (by gallstones or external obstruction by cancer). If longstanding, it leads to destruction and inflammation of liver tissue.
Autoimmune
Anomalous presentation of human leukocyte antigen (HLA) class II on the surface of hepatocytes, possibly due to genetic predisposition or acute liver infection; causes a cell-mediated immune response against the body's own liver, resulting in autoimmune hepatitis.
Alpha 1-antitrypsin deficiency
In severe cases of alpha 1-antitrypsin deficiency (A1AD), the accumulated protein in the endoplasmic reticulum causes liver cell damage and inflammation.
Non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD) is the occurrence of fatty liver in people who have no history of alcohol use. It is most commonly associated with obesity (80% of all obese people have fatty liver). It is more common in women. Severe NAFLD leads to inflammation, a state referred to as non-alcoholic steatohepatitis (NASH), which on biopsy of the liver resembles alcoholic hepatitis (with fat droplets and inflammatory cells, but usually no Mallory bodies).
The diagnosis depends on medical history, physical exam, blood tests, radiological imaging and sometimes a liver biopsy. The initial evaluation to identify the presence of fatty infiltration of the liver is medical imaging, including such ultrasound, computed tomography (CT), or magnetic resonance (MRI). However, imaging cannot readily identify inflammation in the liver. Therefore, the differentiation between steatosis and NASH often requires a liver biopsy. It can also be difficult to distinguish NASH from alcoholic hepatitis when the patient has a history of alcohol consumption. Sometimes in such cases a trial of abstinence from alcohol along with follow-up blood tests and a repeated liver biopsy are required.
NASH is becoming recognized as the most important cause of liver disease second only to hepatitis C in numbers of patients going on to cirrhosis.[citation needed]
Ischemic hepatitis
Ischemic hepatitis is caused by decreased circulation to the liver cells. Usually this is due to decreased blood pressure (or shock), leading to the equivalent term "shock liver". Patients with ischemic hepatitis are usually very ill due to the underlying cause of shock. Rarely, ischemic hepatitis can be caused by local problems with the blood vessels that supply oxygen to the liver (such as thrombosis, or clotting of the hepatic artery which partially supplies blood to liver cells). Blood testing of a person with ischemic hepatitis will show very high levels of transaminase enzymes (AST and ALT), which may exceed 1000 U/L. The elevation in these blood tests is usually transient (lasting 7 to 10 days). It is rare that liver function will be affected by ischemic hepatitis.
See also
References
- ^ Online Etymology Dictionary
- ^ Ryder S, Beckingham I (2001). "Acute hepatitis". BMJ 322 (7279): 151–153. doi:10.1136/bmj.322.7279.151. PMC 1119417. PMID 11159575. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1119417.
- ^ a b V.G. Bain and M. Ma, Acute Viral Hepatitis, Chapter 14, First principle of gastroenterology (an online text book)
- ^ a b Chronic hepatitis at Merck Manual of Diagnosis and Therapy Home Edition
- ^ Figure 7.12 (Some causes of acute parenchymal damage), Parveen, M.D. Kumar (Editor), Michael, M.d. Clark (Editor) (2005). Clinical Medicine: with STUDENT CONSULT Access. Philadelphia, PA: W.B. Saunders Company. ISBN 0-7020-2763-4.
- ^ Scott Moses, MD, Acute Hepatitis causes, Family practice notebook.com
- ^ "Hepatitis as a result of chemicals and drugs". HealthAtoZ. Archived from the original on 2006-06-23. http://web.archive.org/web/20060623141402/http://www.healthatoz.com/healthatoz/Atoz/dc/caz/infc/hepa/hepres.jsp. Retrieved 2006-07-01.
- ^ Lim JR, Faught PR, Chalasani NP, Molleston JP (2006). "Severe liver injury after initiating therapy with atomoxetine in two children". J. Pediatr. 148 (6): 831–4. doi:10.1016/j.jpeds.2006.01.035. PMID 16769398.
- ^ Bastida G, Nos P, Aguas M, Beltrán B, Rubín A, Dasí F, Ponce J (2005). "Incidence, risk factors and clinical course of thiopurine-induced liver injury in patients with inflammatory bowel disease". Aliment Pharmacol Ther 22 (9): 775–82. doi:10.1111/j.1365-2036.2005.02636.x. PMID 16225485.
- ^ Nadir A, Reddy D, Van Thiel DH (2000). "Cascara sagrada-induced intrahepatic cholestasis causing portal hypertension: case report and review of herbal hepatotoxicity". Am. J. Gastroenterol. 95 (12): 3634–7. doi:10.1111/j.1572-0241.2000.03386.x. PMID 11151906.
External links
Inflammation Acute preformed: Lysosome granules · vasoactive amines (Histamine, Serotonin)
synthesized on demand: cytokines (IFN-γ, IL-8, TNF-α, IL-1) · eicosanoids (Leukotriene B4, Prostaglandins) · Nitric oxide · KininsChronic Processes Traditional: Rubor · Calor · Tumor · Dolor (pain) · Functio laesa
Modern: Acute-phase reaction/Fever · Vasodilation · Increased vascular permeability · Exudate · Leukocyte extravasation · ChemotaxisSpecific locations CNS (Encephalitis, Myelitis) · Meningitis (Arachnoiditis) · PNS (Neuritis) · eye (Dacryoadenitis, Scleritis, Keratitis, Choroiditis, Retinitis, Chorioretinitis, Blepharitis, Conjunctivitis, Iritis, Uveitis) · ear (Otitis, Labyrinthitis, Mastoiditis)CardiovascularCarditis (Endocarditis, Myocarditis, Pericarditis) · Vasculitis (Arteritis, Phlebitis, Capillaritis)upper (Sinusitis, Rhinitis, Pharyngitis, Laryngitis) · lower (Tracheitis, Bronchitis, Bronchiolitis, Pneumonitis, Pleuritis) · MediastinitisDigestivemouth (Stomatitis, Gingivitis, Gingivostomatitis, Glossitis, Tonsillitis, Sialadenitis/Parotitis, Cheilitis, Pulpitis, Gnathitis) · tract (Esophagitis, Gastritis, Gastroenteritis, Enteritis, Colitis, Enterocolitis, Duodenitis, Ileitis, Caecitis, Appendicitis, Proctitis) · accessory (Hepatitis, Cholangitis, Cholecystitis, Pancreatitis) · PeritonitisArthritis · Dermatomyositis · soft tissue (Myositis, Synovitis/Tenosynovitis, Bursitis, Enthesitis, Fasciitis, Capsulitis, Epicondylitis, Tendinitis, Panniculitis)
Osteochondritis: Osteitis (Spondylitis, Periostitis) · Chondritisfemale: Oophoritis · Salpingitis · Endometritis · Parametritis · Cervicitis · Vaginitis · Vulvitis · Mastitis
male: Orchitis · Epididymitis · Prostatitis · Balanitis · Balanoposthitis
pregnancy/newborn: Chorioamnionitis · OmphalitisCategories:- Hepatitis
- Inflammations
- Viral hepatitis:
Wikimedia Foundation. 2010.
