- Steatohepatitis
-
Steatohepatitis Classification and external resources 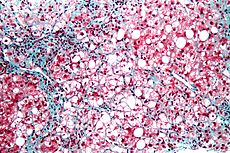
Micrograph of steatohepatitis. Liver biopsy. Trichrome stainICD-10 K70.1, K76.0 ICD-9 571.0, 571.8 DiseasesDB 29786 eMedicine article/170539 MeSH C06.552.241 Steatohepatitis (also known as fatty liver disease) is a type of liver disease, characterized by inflammation of the liver with concurrent fat accumulation in liver ("steato", meaning fat, "hepatitis", meaning inflammation of the liver). Mere deposition of fat in the liver is termed steatosis, and together these constitute fatty liver changes.
Classically seen in alcoholics as part of alcoholic liver disease, steatohepatitis also is frequently found in people with diabetes and obesity and it is related to metabolic syndrome. When not associated with excessive alcohol intake, it is referred to as non-alcoholic steatohepatitis, or NASH and is the progressive form of the relatively benign Non-alcoholic fatty liver disease.[1] Steatohepatitis of either etiology may progress to cirrhosis, and NASH is now believed to be a frequent cause of unexplained cirrhosis (at least in Western societies). NASH is also associated with Lysosomal Acid Lipase Deficiency.
Contents
Pathophysiology
Steatohepatitis is characterized microscopically by hepatic fat accumulation (steatosis), mixed lobular inflammation, ballooning degeneration of hepatocytes (sometimes with identifiable Mallory bodies), glycogenated hepatocyte nuclei, and pericellular fibrosis. The "chicken wire" pattern of the pericellular fibrosis, which affects portal areas only secondarily in later stages, is very characteristic and is identified on trichrome stains.
Treatment
Recent studies suggest that diet, exercise, and antiglycemic drugs may alter the course of the disease. A randomized controlled trial found that "pioglitazone led to metabolic and histologic improvement in subjects with nonalcoholic steatohepatitis".[2]
As of 2007, no treatment has yet emerged as the "gold standard". General recommendations include improving metabolic risk factors and reducing alcohol intake.[3]. However, Vitamin E can improve some symptoms of NASH and was superior to insulin sensitizer in one large study. In the Pioglitazone versus Vitamin E versus Placebo for the Treatment of Nondiabetic Patients with Nonalcoholic Steatohepatitis (PIVENS) trial, for patients with NASH but without diabetes mellitus, the use of very high dosages of vitamin E (800 IU/day) for four years was associated with a significantly higher rate of improvement than placebo (43% vs. 19%) in the primary outcome. The primary outcome was an improvement in certain histological features as measured by biopsy—but it did not improve fibrosis. Pioglitazone, an insulin sensitizer, improved some features of NASH but not the primary outcome, and resulted in a significant weight gain (mean 4.7 kilograms) which persisted after pioglitazone was discontinued.[4]
Prognosis
A retrospective cohort study concluded that "liver failure is the main cause of morbidity and mortality in NASH-associated cirrhosis. The prognosis is either similar or less severe than HCV-cirrhosis."[5]
History
NASH was first described in 1980 in a series of patients of the Mayo Clinic.[6] Its relevance and high prevalence were recognized mainly in the 1990s. Some think that NASH is a diagnosis of exclusion, and that many cases may be in fact be due to other causes.[7]
See also
- Alcoholic liver disease
- Non-alcoholic fatty liver disease
- Steatosis hepatitis
- Lysosomal acid lipase deficiency
- Hepatitis C Long-Term Outcomes of Cirrhosis in Nonalcoholic Steatohepatitis Compared With Hepatitis C
References
- ^ Vuppalanchi R, Chalasani N (January 2009). "Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis: Selected practical issues in their evaluation and management". Hepatology 49 (1): 306–17. doi:10.1002/hep.22603. PMC 2766096. PMID 19065650. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2766096.
- ^ Belfort R, Harrison SA, Brown K, et al. (2006). "A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis". N. Engl. J. Med. 355 (22): 2297–307. doi:10.1056/NEJMoa060326. PMID 17135584.
- ^ Adams LA, Angulo P (2006). "Treatment of non-alcoholic fatty liver disease". Postgrad Med J 82 (967): 315–22. doi:10.1136/pgmj.2005.042200. PMC 2563793. PMID 16679470. http://pmj.bmj.com/cgi/content/full/82/967/315.
- ^ Sanyal AJ, Chalasani N, Kowdley KV, et al. (May 2010). "Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis". N. Engl. J. Med. 362 (18): 1675–85. doi:10.1056/NEJMoa0907929. PMC 2928471. PMID 20427778. http://content.nejm.org/cgi/content/abstract/362/18/1675.
- ^ Hui JM, Kench JG, Chitturi S, et al. (2003). "Long-term outcomes of cirrhosis in nonalcoholic steatohepatitis compared with hepatitis C". Hepatology 38 (2): 420–7. doi:10.1053/jhep.2003.50320. PMID 12883486.
- ^ Ludwig J, Viggiano TR, McGill DB, Oh BJ (1980). "Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease". Mayo Clin Proc 55 (7): 434–438. PMID 7382552.
- ^ Cassiman D, Jaeken J (2008). "NASH may be trash". Gut 57 (2): 141–4. doi:10.1136/gut.2007.123240. PMID 18192446.
Categories:
Wikimedia Foundation. 2010.
