- Granuloma
-
"Granulomatous" and "Granulomatous reaction" redirect here. For the Interstitial granulomatous drug reaction, see Interstitial granulomatous drug reaction.
Granuloma Classification and external resources 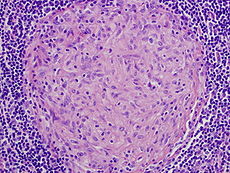
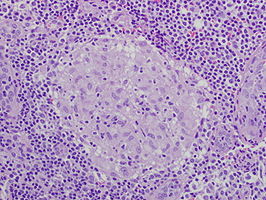
Picture of a granuloma (without necrosis) as seen through a microscope on a glass slide. The tissue on the slide is stained with two standard dyes (hematoxylin: blue, eosin: pink) to make it visible. The granuloma in this picture was found in a lymph node of a patient with Mycobacterium avium infectionICD-10 L92 ICD-9 686.1, 709.4 MeSH D006099 Granuloma is a medical term for a tiny collection of immune cells known as macrophages. Granulomas form when the immune system attempts to wall off substances that it perceives as foreign but is unable to eliminate. Such substances include infectious organisms such as bacteria and fungi as well as other materials such as keratin and suture fragments.[1][2][3] A granuloma is therefore a special type of inflammation that can occur in a wide variety of diseases. The adjective granulomatous means characterized by granulomas.
Contents
Definition
In medical practice, doctors occasionally use the term "granuloma" loosely to mean "a small nodule". Since a small nodule can represent anything from a harmless nevus to a malignant tumor, this usage of the term is not very specific. Similarly, radiologists often use the term granuloma when they see a calcified nodule on X-ray or CT scan of the chest. They make this assumption since granulomas often contain calcium, although the cells that form a granuloma are too tiny to be seen by a radiologist. The most accurate use of the term "granuloma" requires a pathologist to examine surgically removed and specially colored (stained) tissue under a microscope. The following is a more technical definition of a granuloma.
In pathology, a granuloma (classical Greek plural granulomata; modern anglicized plural granulomas) is an organized collection of macrophages.[4]
Macrophages (also known as histiocytes) are the cells that define a granuloma. They often, but not invariably, fuse to form multinucleated giant cells (Langhans giant cell).[5] The macrophages in granulomas are often referred to as "epithelioid". This term refers to the vague resemblance of these macrophages to epithelial cells. Epithelioid macrophages differ from ordinary macrophages in that they have elongated nuclei that often resemble the sole of a slipper or shoe. They also have larger nuclei than ordinary macrophages and their cytoplasm is typically more pink when stained with eosin. These changes are thought to be a consequence of "activation" of the macrophage by the offending antigen.
The other key term in the above definition is the word "organized" that refers to a tight, ball-like formation. The macrophages in these formations are typically so tightly clustered that the borders of individual cells are difficult to appreciate. Loosely dispersed macrophages are not considered to be granulomas.
All granulomas, regardless of cause, may contain additional cells and matrix. These include lymphocytes, neutrophils, eosinophils, multinucleated giant cells, fibroblasts and collagen (fibrosis). The additional cells are sometimes a clue to the cause of the granuloma. For example, granulomas with numerous eosinophils may be a clue to coccidioidomycosis or allergic bronchopulmonary fungal disease, and granulomas with numerous neutrophils suggest blastomycosis, Wegener's granulomatosis, aspiration pneumonia or cat-scratch disease.
In terms of the underlying cause, the difference between granulomas and other types of inflammation is that granulomas form in response to antigens that are resistant to "first-responder" inflammatory cells such as neutrophils and eosinophils. The antigen causing the formation of a granuloma is most often an infectious pathogen or a substance foreign to the body, but often the offending antigen is unknown (as in sarcoidosis).
Granulomas are seen in a wide variety of diseases, both infectious and non-infectious.[1] Infections that are characterized by granulomas include tuberculosis, leprosy, histoplasmosis, cryptococcosis, coccidioidomycosis, blastomycosis and cat scratch disease. Examples of non-infectious granulomatous diseases are sarcoidosis, Crohn's disease, berylliosis, Wegener's granulomatosis, Churg-Strauss syndrome, pulmonary rheumatoid nodules and aspiration of food and other particulate material into the lung.
An important feature of granulomas is whether or not they contain necrosis. Necrosis refers to dead cells that, under the microscope, appear as a mass of formless debris with no nuclei present. A related term, "caseation" (literally: turning to cheese) refers to a form of necrosis that, to the unaided eye (i.e., without a microscope), appears cheese-like ("caseous"), and is typically (but not uniquely) a feature of the granulomas of tuberculosis. The identification of necrosis in granulomas is important because granulomas with necrosis tend to have infectious causes. There are several exceptions to this general rule, but it nevertheless remains useful in day-to-day diagnostic pathology.
- Necrosis in granulomas
-
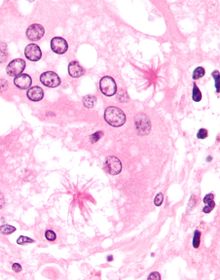
Granuloma with central necrosis in a lung of a person with tuberculosis. Note the Langhans-type giant cells (with many nuclei arranged in a horseshoe-like pattern at the edge of the cell) around the periphery of the granuloma. Langhans-type giant cells are seen in many types of granulomas, and are not specific for tuberculosis.
Diseases characterized by granulomas
Tuberculosis
The granulomas of tuberculosis tend to contain necrosis ("caseating tubercules"), but non-necrotizing granulomas may also be present. Multinucleated giant cells with nuclei arranged like a horseshoe (Langhans giant cell) are often present, but are not specific for tuberculosis. The diagnosis of tuberculosis requires identification of the causative organism by microbiologic cultures.
Leprosy
In leprosy, granulomas are found in the skin and tend to involve nerves. The appearance of the granulomas differs according to the precise type of leprosy.
Schistosomiasis
Some schistosome ova that are laid in intestinal and urinary veinules backwash into the liver via the portal vein causing granuloma formation in the liver.
Histoplasmosis
Granulomas are seen in most forms of histoplasmosis (acute histoplasmosis, histoplasmoma, chronic histoplasmosis). Histoplasma organisms can sometimes be demonstrated within the granulomas by biopsy or microbiological cultures.
Cryptococcosis
When Cryptococcus infection occurs in persons whose immune systems are intact, granulomatous inflammation is typically encountered. The granulomas can be necrotizing or non-necrotizing. Using a microscope and appropriate stains, organisms can be seen within the granulomas.
Cat-scratch disease
Cat-scratch disease is an infection caused by the bacterial organism Bartonella henselae, typically acquired by a scratch from a kitten infected with the organism. The granulomas in this disease are found in the lymph nodes draining the site of the scratch. They are characteristically "suppurative", i.e., pus forming, containing large numbers of neutrophils. Organisms are usually difficult to find within the granulomas using methods routinely used in pathology laboratories.
Sarcoidosis
Sarcoidosis is a disease of unknown cause characterized by granulomas in multiple organs and body sites [6], most commonly the lungs and lymph nodes within the chest cavity. Other common sites of involvement include the liver, spleen, skin and eyes. The granulomas of sarcoidosis are similar to the granulomas of tuberculosis and other infectious granulomatous diseases. However, in most cases of sarcoidosis, the granulomas do not contain necrosis and are surrounded by concentric scar tissue (fibrosis). Sarcoid granulomas often contain star-shaped structures termed asteroid bodies or lamellar structures termed Schaumann bodies. However, these structures are not specific for sarcoidosis [7]. Sarcoid granulomas can resolve spontaneously without complications or heal with residual scarring. In the lungs, this scarring can cause a condition known as pulmonary fibrosis that impairs breathing; in the heart, it can lead to rhythm disturbances, heart failure and even death.
Crohn's disease
Crohn's disease is an inflammatory condition of uncertain cause characterized by severe inflammation in the wall of the intestines and other parts of the abdomen. Within the inflammation in the gut wall, granulomas are often found, and are a clue to the diagnosis.[8]
Pneumocystis pneumonia
Pneumocystis infection in the lungs is usually not associated with granulomas, but rare cases are well documented to cause granuomatous inflammation. The diagnosis is established by finding Pneumocystis yeasts within the granulomas on lung biopsies [9].
Aspiration pneumonia
Aspiration pneumonia is typically caused by aspiration of bacteria from the oral cavity into the lungs, and does not result in the formation of granulomas. However, granulomas may form when food particles or other particulate substances like pill fragments are aspirated into the lungs. Patients typically aspirate food because they have esophageal, gastric or neurologic problems. Intake of drugs that depress neurologic function may also lead to aspiration. The resultant granulomas are typically found around the airways (bronchioles) and are often accompanied by foreign-body-type multinucleated giant cells, acute inflammation or organizing pneumonia. The finding of food particles in lung biopsies is diagnostic.[10]
Granulomas associated with vasculitis
Certain inflammatory diseases are characterised by a combination of granulomatous inflammation and vasculitis (inflammation of the blood vessels). Both the granulomas as well as the vasculitis tend to occur in association with necrosis. Classic examples of such diseases include Wegener's Granulomatosis and Churg-Strauss Syndrome.
References
- ^ a b Woodard BH, Rosenberg SI, Farnham R, Adams DO (1982). "Incidence and nature of primary granulomatous inflammation in surgically removed material". American Journal of Surgical Pathology 6 (2): 119–129. doi:10.1097/00000478-198203000-00004. PMID 7102892.
- ^ Hunter DC, Logie JR (1988). "Suture granuloma". British Journal of Surgery 75 (11): 1149–1150. doi:10.1002/bjs.1800751140. PMID 3208057.
- ^ Chen KT, Kostich ND, Rosai J (1978). "Peritoneal foreign body granulomas to keratin in uterine adenocanthoma". Archives of Pathology and Laboratory Medicine 102 (4): 174–177. PMID 580709.
- ^ Adams DO (1976). "The granulomatous inflammatory response. A review". American Journal of Pathology 84 (1): 164–191. PMC 2032357. PMID 937513. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2032357.
- ^ Janeway's Immunobiology. Garland Science. 2008. p. 372.
- ^ Iannuzzi M, Rybicki BA, Teirstein AS (2007). "Sarcoidosis". New England Journal of Medicine 357 (21): 2153–2165. doi:10.1056/NEJMra071714. PMID 18032765.
- ^ Mukhopadhyay S, Gal AA. (2010). "Granulomatous lung disease: an approach to the differential diagnosis". Archives of Pathology and Laboratory Medicine 134 (5): 669–690. doi:10.1043/1543-2165-134.5.667. PMID 20441499.
- ^ "Teen diagnoses her own disease in science class"
- ^ Hartel PH, Shilo K, Klassen-Fischer M, et al. (2010). "Granulomatous reaction to Pneumocystis jirovecii. clinicopathologic review of 20 cases". American Journal of Surgical Pathology 34 (5): 730–734. doi:10.1097/PAS.0b013e3181d9f16a. PMID 20414100.
- ^ Mukhopadhyay S, Katzenstein AL (2007). "Pulmonary disease due to aspiration of food and other particulate matter: a clinicopathologic study of 59 cases diagnosed on biopsy or resection specimens". American Journal of Surgical Pathology 31 (5): 752–759. doi:10.1097/01.pas.0000213418.08009.f9. PMID 17460460.
External links
- Atlas of Granulomatous Diseases Yale Rosen, M.D.
Cutaneous keratosis, ulcer, atrophy, and necrobiosis (L82–L94, 700–701.5) Epidermal thickening keratoderma: Keratoderma climactericum • Paraneoplastic keratoderma (Acrokeratosis paraneoplastica of Bazex ) • Aquagenic keratoderma · Drug-induced keratoderma · Paraneoplastic keratoderma • psoriasis (Keratoderma blennorrhagica)
keratosis: Seborrheic keratosis (Clonal seborrheic keratosis · Common seborrheic keratosis · Irritated seborrheic keratosis · Seborrheic keratosis with squamous atypia · Reticulated seborrheic keratosis · Dermatosis papulosa nigra) • Keratosis punctata of the palmar creases
other hyperkeratosis: Acanthosis nigricans (Confluent and reticulated papillomatosis) · Callus • Ichthyosis acquisita · Arsenical keratosis · Chronic scar keratosis · Hyperkeratosis lenticularis perstans · Hydrocarbon keratosis · Hyperkeratosis of the nipple and areola · Inverted follicular keratosis · Lichenoid keratosis · Multiple minute digitate hyperkeratosis · PUVA keratosis · Reactional keratosis · Stucco keratosis · Thermal keratosis · Viral keratosis · Warty dyskeratoma · Waxy keratosis of childhood
other hypertrophy: Keloid · Hypertrophic scar • Cutis verticis gyrata ·Necrobiosis/granuloma Granuloma annulare (Perforating, Generalized, Subcutaneous, Granuloma annulare in HIV disease, Localized granuloma annulare, Patch-type granuloma annulare) · Necrobiosis lipoidica · Annular elastolytic giant cell granuloma · Granuloma multiforme · Necrobiotic xanthogranuloma · Palisaded neutrophilic and granulomatous dermatitis · Rheumatoid nodulosis · Interstitial granulomatous dermatitis/Interstitial granulomatous drug reactionForeign body granulomaBeryllium granuloma • Mercury granuloma • Silica granuloma • Silicone granuloma • Zirconium granuloma • Soot tattoo • Tattoo • Carbon stainOther/ungroupedDermis/
localized CTDCutaneous lupus
erythematosusLocalized scleroderma (Localized morphea, Morphea–lichen sclerosus et atrophicus overlap, Generalized morphea, Atrophoderma of Pasini and Pierini, Pansclerotic morphea, Morphea profunda, Linear scleroderma)Lichen sclerosus · Anetoderma (Schweninger–Buzzi anetoderma, Jadassohn–Pellizzari anetoderma) · Atrophoderma of Pasini and Pierini · Acrodermatitis chronica atrophicans · Semicircular lipoatrophy · Follicular atrophoderma · Linear atrophoderma of MoulinKyrle disease · Reactive perforating collagenosis · Elastosis perforans serpiginosa · Perforating folliculitis · Acquired perforating dermatosisOtherCategories:
Wikimedia Foundation. 2010.