- Thyroiditis
-
Thyroiditis Classification and external resources 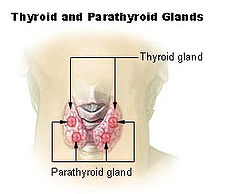
Above shows two parts of the thyroid that could potentially be affected if diagnosed with thyroiditis.ICD-10 E06 ICD-9 245 DiseasesDB 13095 eMedicine ped/2248 MeSH D013966 Thyroiditis is the inflammation of the thyroid gland. The thyroid gland is located on the front of the neck below the laryngeal prominence, and makes hormones that control metabolism.
Contents
Classification
Thyroiditis is a group of disorders that all cause thyroidal inflammation. Forms of the disease are Hashimoto's thyroiditis, the most commom cause of hypothyroidism in the US, postpartum thyroiditis, subacute thyroiditis, silent thyroiditis, drug-induced thyroiditis, radiation-induced thyroiditis, and acute thyroiditis.[1]
Each different type of this disease has its own causes, clinical features, diagnoses, durations, resolutions, conditions and risks.
Symptoms
There are many different symptoms for thyroiditis, none of which are exclusively limited to this disease. Many of the signs imitate symptoms of other diseases, so thyroiditis can sometimes be difficult to diagnose. Common hypothyroid symptoms manifest when thyroid cell damage is slow and chronic, and may include fatigue, weight gain, feeling "fuzzy headed," depression, dry skin, and constipation. Other, rarer symptoms include swelling of the legs, vague aches and pains, decreased concentration and so on. When conditions become more severe, depending on the type of thyroiditis, one may start to see puffiness around the eyes, slowing of the heart rate, a drop in body temperature, or even incipient heart failure. On the other hand, if the thyroid cell damage is acute, the thyroid hormone within the gland leaks out into the bloodstream causing symptoms of thyrotoxicosis, which is similar to those of hyperthyroidism. These symptoms include weight loss, irritability, anxiety, insomnia, fast heart rate, and fatigue. Elevated levels of thyroid hormone in the bloodstream cause both conditions, but thyrotoxicosis is the term used for with thyroiditis since the thyroid gland is not overactive, as in the case of hyperthyroidism.[2][3]
Causes
Thyroiditis is generally caused by an attack on the thyroid, resulting in inflammation and damage to the thyroid cells. This disease is often considered a malfunction of the immune system. Antibodies that attack the thyroid are what causes most types of thyroiditis. It can also be caused by an infection, like a virus or bacteria, which works in the same way as antibodies to cause inflammation in the glands.[4] Certain people make thyroid antibodies, and thyroiditis can be considered an autoimmune disease, because the body acts as if the thyroid gland is foreign tissue.[5] Some drugs, such as interferon and amiodarone, can also cause thyroiditis because they have a tendency to damage thyroid cells.
Diagnosis/investigation
The most common and helpful way to diagnose thyroiditis is first for a physician to palpate the thyroid gland during a physical examination. Laboratory tests allow doctors to evaluate the patient for elevated erythrocyte sedimentation rates, elevated thyroglobulin levels, and depressed radioactive iodine intake (Mather, 2007). Blood tests also help to determine the kind of thyroiditis and to see how much thyroid stimulating hormone the pituitary gland is producing and what antibodies are present in the body. In some cases a biopsy may be needed to find out what is attacking the thyroid.
Conditions
Most types of thyroiditis are three to five times more likely to be found in women than in men. The average age of onset is between thirty and fifty years of age. This disease tends to be geographical and seasonal, and is most common in summer and fall.[3]
Treatment
Treatments for this disease depends on the type of thyroiditis that is diagnosed. For the most common type, which is known as Hashimoto’s thyroiditis, the treatment is to immediately start hormone replacement. This prevents or corrects the hypothyroidism, and it also generally keeps the gland from getting bigger.[6] Often, victims of this disease only need bed rest and non-steroidal anti-inflammatory medications; however, some need steroids to reduce inflammation and to control palpitations. Depending on the type of thyroiditis, doctors may prescribe drugs called beta blockers to lower the heart rate and reduce tremors.[7]
Hashimoto’s Thyroiditis
Hashimoto's thyroiditis was first described by Japanese physician Hashimoto Hakaru working in Germany in 1912. Hashimoto’s thyroiditis is also known as lymphocytic thyroiditis, and patients with this disease often complain about difficulty swallowing. This condition may be so mild at first that the disease goes unnoticed for years. The first symptom that shows signs of Hashimoto’s thyroiditis is a goitre on the front of the neck.[6] Depending on the severity of the disease and how much it has progressed, doctors then decide what steps are taken for treatment.
See also
- Hypothyroidism
- Hashitoxicosis
- Hyperthyroidism
- Hashimoto's Disease
- Thyroid Cancer
References
- ^ "Thyroiditis." www.thyroid.org. 2005. American Thyroid Association. 13 Mar. 2008. 15 Oct. 2010 <http://www.thyroid.org/patients/brochures/Thyroiditis.pdf>.
- ^ "Thyroiditis." www.thyroid.org. 2005. American Thyroid Association. 15 Oct. 2010 <http://www.thyroid.org/patients/brochures/Thyroiditis.pdf>.
- ^ a b Thyroiditis." Familydoctor.Org. 2007. American Academy of Family Physicians. 9 Mar. 2008 <http://familydoctor.org/online/famdocen/home/common /hormone /913.html>.
- ^ De Groot, Leslie J., Nobuyuki Amino, and Akamizu Takashi. "Hashimoto's Thryoiditis." 30 Jan. 2007. Takashi Akamizu. 3 Mar. 2008 <www.thyroidmanager.org/Chapter8/chapter8.html>.
- ^ Mather, M.d., Ruchi. "Hashimoto's Thryoiditis." Medicine.Net. 8 Sept. 2007. 9 Mar. 2008 <http://www.medicinenet.com/hashimotos_thyroiditis/article.htm>.
- ^ a b "Hashimoto's Thryoiditis." ECureMe.Com. 2003. 15 Mar. 2008 <http://www.google.com/imgres?imgurl=http://www.ecureme.com>.
- ^ "Hashimotos Disease." Health Encyclopedia Diseases and ConditioNS. 2008. USA Today. 9 Mar. 2008 <http://www.healthscout.com/ency/68/277/main.html>.
Endocrine pathology: endocrine diseases (E00–E35, 240–259) Pancreas/
glucose
metabolismHypofunctiontypes: (type 1, type 2, MODY 1 2 3 4 5 6) · complications (coma, angiopathy, ketoacidosis, nephropathy, neuropathy, retinopathy, cardiomyopathy)
insulin receptor (Rabson–Mendenhall syndrome) · Insulin resistanceHyperfunctionHypothalamic/
pituitary axesHypothalamusPituitaryanterior (Acromegaly, Hyperprolactinaemia, Pituitary ACTH hypersecretion) · posterior (SIADH) · general (Nelson's syndrome)anterior (Kallmann syndrome, Growth hormone deficiency, ACTH deficiency/Secondary adrenal insufficiency) · posterior (Neurogenic diabetes insipidus) · general (Empty sella syndrome, Pituitary apoplexy, Sheehan's syndrome, Lymphocytic hypophysitis)ThyroidHyperthyroxinemia (Thyroid hormone resistance, Familial dysalbuminemic hyperthyroxinemia) · Hashitoxicosis · Thyrotoxicosis factitia · Graves' diseaseThyroiditisAcute infectious · Subacute (De Quervain's, Subacute lymphocytic) · Autoimmune/chronic (Hashimoto's, Postpartum, Riedel's)ParathyroidAdrenalaldosterone: Hyperaldosteronism/Primary aldosteronism (Conn syndrome, Bartter syndrome, Glucocorticoid remediable aldosteronism) · AME · Liddle's syndrome · 17α CAHGonadsHeight Multiple Autoimmune polyendocrine syndrome (APS1, APS2) · Carcinoid syndrome · Multiple endocrine neoplasia (1, 2A, 2B) · Progeria (Werner syndrome, Acrogeria, Metageria) · Woodhouse-Sakati syndromeCategories:- Thyroid disease
- Inflammations
Wikimedia Foundation. 2010.
