- Primary aldosteronism
-
Primary hyperaldosteronism Classification and external resources 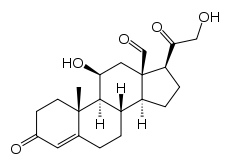
AldosteroneICD-10 E26.0 ICD-9 255.1 DiseasesDB 3073 MedlinePlus 000330 eMedicine med/432 MeSH D006929 Primary aldosteronism, also known as primary hyperaldosteronism, is characterized by the overproduction of the mineralocorticoid hormone aldosterone by the adrenal glands.,[1] when not a result of excessive renin secretion. Aldosterone causes increase in sodium and water retention and potassium excretion in the kidneys, leading to arterial hypertension (high blood pressure). An increase in the production of mineralocorticoid from the adrenal gland is evident. It is amongst the most common causes of secondary hypertension,[2] renal disease being the most common.
Primary hyperaldosteronism has many causes, including adrenal hyperplasia and adrenal carcinoma.[3] When it occurs due to a solitary aldosterone-secreting adrenal adenoma (a type of benign tumor), it is known as Conn's syndrome,.[4] In practice, however, the terms are often used interchangeably, regardless of the underlying physiology.
Conn's syndrome is an Aldosterone-Producing Adenoma (APA).
Contents
Causes
The syndrome is due to:
- bilateral idiopathic adrenal hyperplasia 70 %
- unilateral idiopathic adrenal hyperplasia 20 %
- aldosterone-secreting adrenal adenoma (benign tumor, < 5%)
- rare forms, including disorders of the renin-angiotensin system
Signs, symptoms and findings
Aldosterone enhances exchange of sodium for potassium in the kidney so increased aldosteronism will lead to hypernatremia and hypokalemia. Once the potassium has been significantly reduced by aldosterone, a sodium/hydrogen pump in the nephron becomes more active leading to increased excretion of hydrogen ions and further exacerbating the hypernatremia. The hydrogen ions that are exchanged for sodium are generated by carbonic anhydrase in the renal tubule epithelium causing increased production of bicarbonate. The increased bicarbonate and the excreted hydrogen combine to generate a metabolic alkalosis. The high pH of the blood makes calcium less available to the tissues and causes symptoms of hypocalcemia (low calcium levels).
The sodium retention leads to plasma volume expansion and elevated blood pressure. The increased blood pressure will lead to increased glomerular filtration rate and cause a decrease in renin release from the granular cells of the juxtaglomerular apparatus in the kidney. If there is a primary hyperaldosteronism the decreased renin (and subsequent decreased angiotensin II) will not lead to a decrease in aldosterone levels (a very helpful clinical tool in diagnosis of primary hyperaldosteronism).
Aside from high blood pressure manifestations of muscle cramps (due to hyperexcitability of neurons secondary to hypocalcemia), muscle weakness (due to hypoexcitability of skeletal muscles secondary to hypokalemia), and headaches (due to hypokalemia or high blood pressure) may be seen.
Secondary hyperaldosteronism is often related to decreased cardiac output which is associated with elevated renin levels.
Diagnosis
Measuring aldosterone alone is not considered adequate to diagnose primary hyperaldosteronism. Rather, both renin and aldosterone are measured, and a resultant aldosterone-to-renin ratio is used for diagnosis.[5][6] A high aldosterone-to-renin ratio indicates presence of primary hyperaldosteronism.
If plasma levels of renin and aldosterone suggest hyperaldosteronism, CT scanning can confirm the presence of an adrenal adenoma. If the clinical presentation primarily involves hypertension and elevated levels of catecholamines, CT or MRI scanning can confirm a tumor on the adrenal medulla, typically an aldosteronoma.
Hyperaldosteronism can be mimicked by Liddle syndrome, and by ingestion of licorice and other foods containing glycyrrhizin. In one case report, hypertension and quadriparesis resulted from intoxication with a non-alcoholic pastis (an anise-flavored aperitif containing glycyrrhizinic acid).[7]
Therapy
The treatment for hyperaldosteronism depends on the underlying cause. In patients with a single benign tumor (adenoma), surgical removal (adrenalectomy) is curative. This is usually performed laparoscopically, through several very small incisions. For patients with hyperplasia of both glands, successful treatment is often achieved with spironolactone or eplerenone, drugs that block the effect of aldosterone. With its antiandrogen effect, spironolactone drug therapy may have a range of effects in males, including sometimes gynecomastia. These symptoms usually do not occur with eplerenone drug therapy.[8]
In the absence of proper treatment, individuals with hyperaldosteronism often suffer from poorly controlled high blood pressure, which may be associated with increased rates of stroke, heart disease, and kidney failure. With appropriate treatment, the prognosis is excellent.[9]
Eponym
Conn's syndrome is named after Jerome W. Conn (1907–1994), the American endocrinologist who first described the condition at the University of Michigan in 1955.[1]
References
- ^ a b Conn JW, Louis LH (1955). "Primary aldosteronism: a new clinical entity". Trans. Assoc. Am. Physicians 68: 215–31; discussion, 231–3. PMID 13299331.
- ^ http://emedicine.medscape.com/article/117280-overview
- ^ http://www.merck.com/mmhe/sec13/ch164/ch164e.html
- ^ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease. St. Louis, Mo: Elsevier Saunders. pp. 1210. ISBN 0-7216-0187-1.
- ^ Tiu S, Choi C, Shek C, Ng Y, Chan F, Ng C, Kong A (2005). "The use of aldosterone-renin ratio as a diagnostic test for primary hyperaldosteronism and its test characteristics under different conditions of blood sampling". J Clin Endocrinol Metab 90 (1): 72–8. doi:10.1210/jc.2004-1149. PMID 15483077.
- ^ United Bristol Healthcare NHS Trust, the major teaching trust in South West England
- ^ Trono D, Cereda JM, Favre L (August 1983). "[Pseudo-Conn's syndrome due to intoxication with nonalcoholic pastis]" (in French). Schweiz Med Wochenschr 113 (31–32): 1092–5. PMID 6623028.
- ^ http://labeling.pfizer.com/ShowLabeling.aspx?id=599
- ^ Columbia Adrenal Center, Hyperaldosteronism (Conn's Syndrome)
Endocrine pathology: endocrine diseases (E00–E35, 240–259) Pancreas/
glucose
metabolismHypofunctiontypes: (type 1, type 2, MODY 1 2 3 4 5 6) · complications (coma, angiopathy, ketoacidosis, nephropathy, neuropathy, retinopathy, cardiomyopathy)
insulin receptor (Rabson–Mendenhall syndrome) · Insulin resistanceHyperfunctionHypothalamic/
pituitary axesHypothalamusPituitaryanterior (Acromegaly, Hyperprolactinaemia, Pituitary ACTH hypersecretion) · posterior (SIADH) · general (Nelson's syndrome)anterior (Kallmann syndrome, Growth hormone deficiency, ACTH deficiency/Secondary adrenal insufficiency) · posterior (Neurogenic diabetes insipidus) · general (Empty sella syndrome, Pituitary apoplexy, Sheehan's syndrome, Lymphocytic hypophysitis)ThyroidHyperthyroxinemia (Thyroid hormone resistance, Familial dysalbuminemic hyperthyroxinemia) · Hashitoxicosis · Thyrotoxicosis factitia · Graves' diseaseAcute infectious · Subacute (De Quervain's, Subacute lymphocytic) · Autoimmune/chronic (Hashimoto's, Postpartum, Riedel's)ParathyroidAdrenalaldosterone: Hyperaldosteronism/Primary aldosteronism (Conn syndrome, Bartter syndrome, Glucocorticoid remediable aldosteronism) · AME · Liddle's syndrome · 17α CAHGonadsHeight Multiple Autoimmune polyendocrine syndrome (APS1, APS2) · Carcinoid syndrome · Multiple endocrine neoplasia (1, 2A, 2B) · Progeria (Werner syndrome, Acrogeria, Metageria) · Woodhouse-Sakati syndromeCategories:- Adrenal gland disorders
Wikimedia Foundation. 2010.
