- Conn's syndrome
-
Main article: Primary aldosteronism
Conn's syndrome Classification and external resources 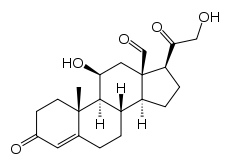
AldosteroneICD-10 E26.0 ICD-9 255.12 DiseasesDB 3073 MeSH D006929 Conn's syndrome is an Aldosterone-Producing Adenoma (APA). Conn's syndrome is named after Jerome W. Conn (1907–1994), the American endocrinologist who first described the condition at the University of Michigan in 1955.[1]
Contents
Causes
Primary hyperaldosteronism has many causes, including adrenal hyperplasia and adrenal carcinoma.[2]
The syndrome is due to:
- bilateral idiopathic adrenal hyperplasia 70 %
- unilateral idiopathic adrenal hyperplasia 20 %
- aldosterone-secreting adrenal adenoma (benign tumor, < 5%)
- rare forms, including disorders of the renin-angiotensin system
Pathogenesis
Aldosterone enhances exchange of sodium for potassium in the kidney so increased aldosteronism will lead to hypernatremia and hypokalemia. Once the potassium has been significantly reduced by aldosterone, a sodium/hydrogen pump in the nephron becomes more active leading to increased excretion of hydrogen ions and further exacerbating the hypernatremia. The hydrogen ions that are exchanged for sodium are generated by carbonic anhydrase in the renal tubule epithelium causing increased production of bicarbonate. The increased bicarbonate and the excreted hydrogen combine to generate a metabolic alkalosis.
The high pH of the blood makes calcium less available to the tissues and causes symptoms of hypocalcemia (low calcium levels).
The sodium retention leads to plasma volume expansion and elevated blood pressure. The increased blood pressure will lead to increased glomerular filtration rate and cause a decrease in renin release from the granular cells of the juxtaglomerular apparatus in the kidney. If a patient is thought to suffer from primary hyperaldosteronism, the Aldo:renin activity ratio is used to assess this. The thought behind this is that decreased renin levels and in turn the reactive down-regulation of angiotensin II are unable to down-regulate the constitutively formed aldosterone, thus leading to an elevated [plasma Aldo:plasma Renin activity] ratio (lending the assay to be a clinical tool for diagnostic purposes).
Aside from Hypertension, other manifesting problems include myalgias, weakness, and chronic headaches. The muscle cramps being due to neuron hyperexcitability seen in the setting of hypocalcemia, muscle weakness secondary to hypoexcitability of skeletal muscles in the setting of hypokalemia, and headaches which are thought to be due to both electrolyte imbalance (hypokalemia) and HTN.
Secondary hyperaldosteronism is often related to decreased cardiac output which is associated with elevated renin levels.
Diagnosis
Measuring aldosterone alone is not considered adequate to diagnose primary hyperaldosteronism. The screening test of choice for diagnosis is Plasma Aldosterone: Plasma renin activity ratio. Note that renin activity and NOT simply plasma renin is being assayed. Both renin and aldosterone are measured and a ratio of >30 is indicative of primary hyperaldosteronism.[3][4]
Dif. Diagnosis
Hyperaldosteronism can be mimicked by Liddle syndrome, and by ingestion of licorice and other foods containing glycyrrhizin. In one case report, hypertension and quadriparesis resulted from intoxication with a non-alcoholic pastis (an anise-flavored aperitif containing glycyrrhizinic acid).[5]
Therapy
In patients with a single benign tumor (adenoma), surgical removal (adrenalectomy) is curative. This is usually performed laparoscopically, through several very small incisions. For patients with hyperplasia of both glands, successful treatment is often achieved with spironolactone or eplerenone, drugs that block the effect of aldosterone. In males, one common side effect of spironolactone drug therapy sometimes seen is gynecomastia. Gynecomastia usually does not occur with eplerenone drug therapy.[citation needed]
Prognosis
In the absence of proper treatment, individuals with hyperaldosteronism often suffer from poorly controlled high blood pressure, which may be associated with increased rates of stroke, heart disease, and kidney failure. With appropriate treatment, the prognosis is excellent.[6]
References
- ^ Conn JW, Louis LH (1955). "Primary aldosteronism: a new clinical entity". Trans. Assoc. Am. Physicians 68: 215–31; discussion, 231–3. PMID 13299331.
- ^ http://www.merck.com/mmhe/sec13/ch164/ch164e.html
- ^ Tiu S, Choi C, Shek C, Ng Y, Chan F, Ng C, Kong A (2005). "The use of aldosterone-renin ratio as a diagnostic test for primary hyperaldosteronism and its test characteristics under different conditions of blood sampling". J Clin Endocrinol Metab 90 (1): 72–8. doi:10.1210/jc.2004-1149. PMID 15483077.
- ^ United Bristol Healthcare NHS Trust, the major teaching trust in South West England
- ^ Trono D, Cereda JM, Favre L (August 1983). "[Pseudo-Conn's syndrome due to intoxication with nonalcoholic pastis]" (in French). Schweiz Med Wochenschr 113 (31-32): 1092–5. PMID 6623028.
- ^ Columbia Adrenal Center, Hyperaldosteronism (Conn's Syndrome)
See also
- Primary aldosteronism
- Adrenal adenoma
Categories:- Adrenal gland disorders
Wikimedia Foundation. 2010.
