- Myxedema
-
Myxoedema Classification and external resources 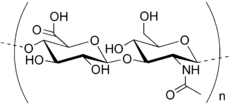
Hyaluronan, an example of a mucopolysaccharide.ICD-10 E03.9 ICD-9 244.9 DiseasesDB 6558 MedlinePlus 000353 eMedicine med/1581 derm/347 MeSH D009230 Myxedema (British English: myxoedema) describes a specific form of cutaneous and dermal edema secondary to increased deposition of connective tissue components (like glycosaminoglycans, hyaluronic acid, and other mucopolysaccharides) in subcutaneous tissue as seen in various forms of hypothyroidism and Graves' disease.[1]:535 It is more common in women than in men. [2]
Contents
Terminology
The word originates from μύξα, taken from ancient Greek to convey 'mucus' or 'slimy substance' and ὁίδημα for swelling.
- Hyperthyroid: Myxedema typically presents in specific areas (pretibial myxedema and exophthalmos) and is related to high levels of TSH receptor stimulation and/or inflammation mounted against the TSH receptor itself. Myxedema of the lower legs (called pretibial myxedema), can occur in one to four percent of patients with Graves' disease -- a condition that causes hyperthyroidism.[3]
- Hypothyroid: Myxedema is also used to describe the clinical syndrome secondary to hypothyroidism. Symptoms can include depression, mental slowness, weakness, bradycardia, fatigue, hypothermia, alopecia, and many others (see symptoms of severe hypothyroidism). Used in this way, myxedema can be considered the adult counterpart of cretinism.[4]
Myxedema coma is rare and establishing the diagnosis requires a high index of suspicion. Myxedema coma represents the severest form of hypothyroidism and has an associated mortality rate of 30 percent to 40 percent. It can occur due to long-standing, untreated hypothyroidism, but is often linked to a precipitant, such as acute infection, myocardial infarction, congestive heart failure, cerebral vascular accident, trauma, or drug toxicity. Several medications can cause hypothyroidism, and patients taking them must be carefully monitored. These medications include amiodarone, lithium, and sedatives. No consensus exists on specific thyroid hormone replacement regimens for myxedema coma. Most experts agree that a large intravenous bolus of levothyroxine should be administered (200 to 400 mcg), followed by daily doses of 50 to 100 mcg, based on the patient's weight and comorbidities. Other experts advocate the use of triiodothyronine (T3) or a combination of both T3 and T4. In addition to thyroid replacement therapy, it is important to detect coexisting adrenal insufficiency and treat patients with stress-dose steroids to avoid precipitating adrenal crisis.[5]
Cause
The increased deposition of glycosaminoglycan is not fully understood, however two mechanisms predominate.
- Exophthalmos in particular results from TSH receptor stimulation on fibroblasts behind the eyes which leads to increased glycosaminoglycan deposition. It is thought that many cells responsible for forming connective tissue react to increases in TSH levels.[citation needed]
- Secondarily, in autoimmune thyroid diseases lymphocytes react to the TSH receptor. Thus, in addition to the inflammation within the thyroid, any cell that expresses the TSH receptor will likely experience lymphocytic infiltrates as well. The inflammation can cause tissue damage and scar tissue formation, explaining the deposition of glycosaminoglycans.[citation needed]
The increased deposition of glycosaminoglycans causes an osmotic edema and fluid collection.
Hashimoto's thyroiditis is the most common cause of myxedema in the United States.[6]
See also
References
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ^ BRS Pathology - A.S. Schneider, P.A. Szanto - 3rd edition - page 314
- ^ "Pretibial Myxedema", Retrieved on 2009-3-27
- ^ "myxedema" at Dorland's Medical Dictionary
- ^ 1.Ross D. Myxedema Coma. UpToDate.com. Last update: September 9, 2009. Available at: http://www.uptodate.com/patients/content/topic.do?topicKey=~aqassDt4J0HGlq. Date accessed: Jan 20, 2010.
- ^ "Hasihimotos Thyroiditis", Retrieved on 2009-3-27
Categories:- Diseases and disorders
- Endocrine-related cutaneous conditions
- Skin conditions resulting from errors in metabolism
Wikimedia Foundation. 2010.
