- Medical imaging
-
This article is about imaging techniques and modalities for the human body. For imaging of animals in research, see Preclinical imaging.
Medical imaging Diagnostics 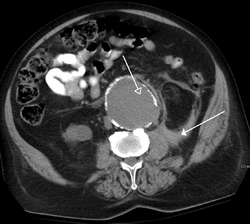
A CT scan image showing a ruptured abdominal aortic aneurysmICD-10-PCS B ICD-9 87-88 MeSH D003952 OPS-301 code 3 MedlinePlus 007451 Medical imaging is the technique and process used to create images of the human body (or parts and function thereof) for clinical purposes (medical procedures seeking to reveal, diagnose or examine disease) or medical science (including the study of normal anatomy and physiology). Although imaging of removed organs and tissues can be performed for medical reasons, such procedures are not usually referred to as medical imaging, but rather are a part of pathology.
As a discipline and in its widest sense, it is part of biological imaging and incorporates radiology (in the wider sense), nuclear medicine, investigative radiological sciences, endoscopy, (medical) thermography, medical photography and microscopy (e.g. for human pathological investigations).
Measurement and recording techniques which are not primarily designed to produce images, such as electroencephalography (EEG), magnetoencephalography (MEG), electrocardiography (EKG) and others, but which produce data susceptible to be represented as maps (i.e. containing positional information), can be seen as forms of medical imaging.
Up until 2010, 5 billion medical imaging studies had been conducted worldwide.[1] Radiation exposure from medical imaging in 2006 made up about 50% of total ionizing radiation exposure in the United States.[2]
Contents
Overview
In the clinical context, "invisible light" medical imaging is generally equated to radiology or "clinical imaging" and the medical practitioner responsible for interpreting (and sometimes acquiring) the images is a radiologist. "Visible light" medical imaging involves digital video or still pictures that can be seen without special equipment. Dermatology and wound care are two modalities that utilize visible light imagery. Diagnostic radiography designates the technical aspects of medical imaging and in particular the acquisition of medical images. The radiographer or radiologic technologist is usually responsible for acquiring medical images of diagnostic quality, although some radiological interventions are performed by radiologists. While radiology is an evaluation of anatomy, nuclear medicine provides functional assessment.
As a field of scientific investigation, medical imaging constitutes a sub-discipline of biomedical engineering, medical physics or medicine depending on the context: Research and development in the area of instrumentation, image acquisition (e.g. radiography), modelling and quantification are usually the preserve of biomedical engineering, medical physics and computer science; Research into the application and interpretation of medical images is usually the preserve of radiology and the medical sub-discipline relevant to medical condition or area of medical science (neuroscience, cardiology, psychiatry, psychology, etc.) under investigation. Many of the techniques developed for medical imaging also have scientific and industrial applications.
Medical imaging is often perceived to designate the set of techniques that noninvasively produce images of the internal aspect of the body. In this restricted sense, medical imaging can be seen as the solution of mathematical inverse problems. This means that cause (the properties of living tissue) is inferred from effect (the observed signal). In the case of ultrasonography the probe consists of ultrasonic pressure waves and echoes inside the tissue show the internal structure. In the case of projection radiography, the probe is X-ray radiation which is absorbed at different rates in different tissue types such as bone, muscle and fat.
The term noninvasive is a term based on the fact that following medical imaging modalities do not penetrate the skin physically. But on the electromagnetic and radiation level, they are quite invasive. From the high energy photons in X-Ray Computed Tomography, to the 2+ Tesla coils of an MRI device, these modalities alter the physical and chemical environment of the body in order to obtain data.
Imaging technology
Radiography
Two forms of radiographic images are in use in medical imaging; projection radiography and fluoroscopy, with the latter being useful for catheter guidance. These 2D techniques are still in wide use despite the advance of 3D tomography due to the low cost, high resolution, and depending on application, lower radiation dosages. This imaging modality utilizes a wide beam of x rays for image acquisition and is the first imaging technique available in modern medicine.
- Fluoroscopy produces real-time images of internal structures of the body in a similar fashion to radiography, but employs a constant input of x-rays, at a lower dose rate. Contrast media, such as barium, iodine, and air are used to visualize internal organs as they work. Fluoroscopy is also used in image-guided procedures when constant feedback during a procedure is required. An image receptor is required to convert the radiation into an image after it has passed through the area of interest. Early on this was a fluorescing screen, which gave way to an Image Amplifier (IA) which was a large vacuum tube that had the receiving end coated with cesium iodide, and a mirror at the opposite end. Eventually the mirror was replaced with a TV camera.
- Projectional radiographs, more commonly known as x-rays, are often used to determine the type and extent of a fracture as well as for detecting pathological changes in the lungs. With the use of radio-opaque contrast media, such as barium, they can also be used to visualize the structure of the stomach and intestines - this can help diagnose ulcers or certain types of colon cancer.
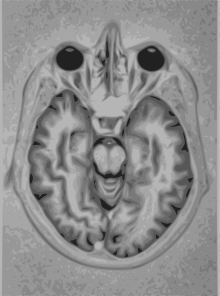
Magnetic resonance imaging (MRI)
A magnetic resonance imaging instrument (MRI scanner), or "nuclear magnetic resonance (NMR) imaging" scanner as it was originally known, uses powerful magnets to polarise and excite hydrogen nuclei (single proton) in water molecules in human tissue, producing a detectable signal which is spatially encoded, resulting in images of the body. The MRI machine emits an RF (radio frequency) pulse that specifically binds only to hydrogen. The system sends the pulse to the area of the body to be examined. The pulse makes the protons in that area absorb the energy needed to make them spin in a different direction. This is the “resonance” part of MRI. The RF pulse makes them (only the one or two extra unmatched protons per million) spin at a specific frequency, in a specific direction. The particular frequency of resonance is called the Larmour frequency and is calculated based on the particular tissue being imaged and the strength of the main magnetic field. MRI uses three electromagnetic fields: a very strong (on the order of units of teslas) static magnetic field to polarize the hydrogen nuclei, called the static field; a weaker time-varying (on the order of 1 kHz) field(s) for spatial encoding, called the gradient field(s); and a weak radio-frequency (RF) field for manipulation of the hydrogen nuclei to produce measurable signals, collected through an RF antenna.
Like CT, MRI traditionally creates a two dimensional image of a thin "slice" of the body and is therefore considered a tomographic imaging technique. Modern MRI instruments are capable of producing images in the form of 3D blocks, which may be considered a generalisation of the single-slice, tomographic, concept. Unlike CT, MRI does not involve the use of ionizing radiation and is therefore not associated with the same health hazards. For example, because MRI has only been in use since the early 1980s, there are no known long-term effects of exposure to strong static fields (this is the subject of some debate; see 'Safety' in MRI) and therefore there is no limit to the number of scans to which an individual can be subjected, in contrast with X-ray and CT. However, there are well-identified health risks associated with tissue heating from exposure to the RF field and the presence of implanted devices in the body, such as pace makers. These risks are strictly controlled as part of the design of the instrument and the scanning protocols used.
Because CT and MRI are sensitive to different tissue properties, the appearance of the images obtained with the two techniques differ markedly. In CT, X-rays must be blocked by some form of dense tissue to create an image, so the image quality when looking at soft tissues will be poor. In MRI, while any nucleus with a net nuclear spin can be used, the proton of the hydrogen atom remains the most widely used, especially in the clinical setting, because it is so ubiquitous and returns a large signal. This nucleus, present in water molecules, allows the excellent soft-tissue contrast achievable with MRI.
Fiduciary Markers
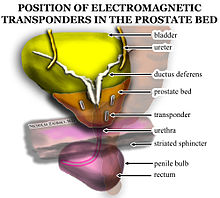 Electromagnetic fiducial transponder beacons are placed in the prostate bed after prostatectomy to improve radiation oncology accuracy. Transponders are placed in a triangular separation pattern, at least one centimeter apart from one another. There is one beacon on either lateral aspect of the vesicoureteral anastomosis and one in the retrovesical tissue approximately at the level where the seminal vesicles had been.
Electromagnetic fiducial transponder beacons are placed in the prostate bed after prostatectomy to improve radiation oncology accuracy. Transponders are placed in a triangular separation pattern, at least one centimeter apart from one another. There is one beacon on either lateral aspect of the vesicoureteral anastomosis and one in the retrovesical tissue approximately at the level where the seminal vesicles had been.
Fiduciary markers are used in a wide range of medical imaging applications. Images of the same subject produced with two different imaging systems may be correlated by placing a fiduciary marker in the area imaged by both systems. In this case, a marker which is visible in the images produced by both imaging modalities must be used. By this method, functional information from SPECT or positron emission tomography can be related to anatomical information provided by magnetic resonance imaging (MRI).[3] Similarly, fiducial points established during MRI can be correlated with brain images generated by magnetoencephalography to localize the source of brain activity.
Nuclear medicine
Nuclear medicine encompasses both diagnostic imaging and treatment of disease, and may also be referred to as molecular medicine or molecular imaging & therapeutics.[4] Nuclear medicine uses certain properties of isotopes and the energetic particles emitted from radioactive material to diagnose or treat various pathology. Different from the typical concept of anatomic radiology, nuclear medicine enables assessment of physiology. This function-based approach to medical evaluation has useful applications in most subspecialties, notably oncology, neurology, and cardiology. Gamma cameras are used in e.g. scintigraphy, SPECT and PET to detect regions of biologic activity that may be associated with disease. Relatively short lived isotope, such as 123I is administered to the patient. Isotopes are often preferentially absorbed by biologically active tissue in the body, and can be used to identify tumors or fracture points in bone. Images are acquired after collimated photons are detected by a crystal that gives off a light signal, which is in turn amplified and converted into count data.
- Scintigraphy ("scint") is a form of diagnostic test wherein radioisotopes are taken internally, for example intravenously or orally. Then, gamma cameras capture and form two-dimensional[5] images from the radiation emitted by the radiopharmaceuticals.
- SPECT is a 3D tomographic technique that uses gamma camera data from many projections and can be reconstructed in different planes. A dual detector head gamma camera combined with a CT scanner, which provides localization of functional SPECT data, is termed a SPECT/CT camera, and has shown utility in advancing the field of molecular imaging. In most other medical imaging modalities, energy is passed through the body and the reaction or result is read by detectors. In SPECT imaging, the patient is injected with a radioisotope, most commonly Thallium 201TI, Technetium 99mTC, Iodine 123I, and Gallium 67Ga[6]
. The radioactive gamma rays are emitted through the body as the natural decaying process of these isotopes takes place. The emissions of the gamma rays are captured by detectors that surround the body. This essentially means that the human is now the source of the radioactivity, rather than the medical imaging devices such as X-Ray, CT, or Ultrasound.
- Positron emission tomography (PET) uses coincidence detection to image functional processes. Short-lived positron emitting isotope, such as 18F, is incorporated with an organic substance such as glucose, creating F18-fluorodeoxyglucose, which can be used as a marker of metabolic utilization. Images of activity distribution throughout the body can show rapidly growing tissue, like tumor, metastasis, or infection. PET images can be viewed in comparison to computed tomography scans to determine an anatomic correlate. Modern scanners combine PET with a CT, or even MRI, to optimize the image reconstruction involved with positron imaging. This is performed on the same equipment without physically moving the patient off of the gantry. The resultant hybrid of functional and anatomic imaging information is a useful tool in non-invasive diagnosis and patient management.
Photo acoustic imaging
Photoacoustic imaging is a recently developed hybrid biomedical imaging modality based on the photoacoustic effect. It combines the advantages of optical absorption contrast with ultrasonic spatial resolution for deep imaging in (optical) diffusive or quasi-diffusive regime. Recent studies have shown that photoacoustic imaging can be used in vivo for tumor angiogenesis monitoring, blood oxygenation mapping, functional brain imaging, and skin melanoma detection, etc.
Breast Thermography
Digital infrared imaging thermography is based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue. Cancerous tumors require an ever-increasing supply of nutrients and therefore increase circulation to their cells by holding open existing blood vessels, opening dormant vessels, and creating new ones (neoangiogenesis). This process frequently results in an increase in regional surface temperatures of the breast. Digital infrared imaging uses extremely sensitive medical infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution diagnostic images of these temperature variations. Because of DII's sensitivity, these temperature variations may be among the earliest signs of breast cancer and/or a pre-cancerous state of the breast.[7]
Tomography
Tomography is the method of imaging a single plane, or slice, of an object resulting in a tomogram. There are several forms of tomography:
- Linear tomography: This is the most basic form of tomography. The X-ray tube moved from point "A" to point "B" above the patient, while the cassette holder (or "bucky") moves simultaneously under the patient from point "B" to point "A." The fulcrum, or pivot point, is set to the area of interest. In this manner, the points above and below the focal plane are blurred out, just as the background is blurred when panning a camera during exposure. No longer carried out and replaced by computed tomography.
- Poly tomography: This was a complex form of tomography. With this technique, a number of geometrical movements were programmed, such as hypocycloidic, circular, figure 8, and elliptical. Philips Medical Systems [1] produced one such device called the 'Polytome.' This unit was still in use into the 1990s, as its resulting images for small or difficult physiology, such as the inner ear, was still difficult to image with CTs at that time. As the resolution of CTs got better, this procedure was taken over by the CT.
- Zonography: This is a variant of linear tomography, where a limited arc of movement is used. It is still used in some centres for visualising the kidney during an intravenous urogram (IVU).
- Orthopantomography (OPT or OPG): The only common tomographic examination in use. This makes use of a complex movement to allow the radiographic examination of the mandible, as if it were a flat bone. It is often referred to as a "Panorex", but this is incorrect, as it is a trademark of a specific company.
- Computed Tomography (CT), or Computed Axial Tomography (CAT: A CT scan, also known as a CAT scan), is a helical tomography (latest generation), which traditionally produces a 2D image of the structures in a thin section of the body. It uses X-rays. It has a greater ionizing radiation dose burden than projection radiography; repeated scans must be limited to avoid health effects. CT is based on the same principles as X-Ray projections but in this case, the patient is enclosed in a surrounding ring of detectors assigned with 500-1000 scintillation detectors[6]
. This being the fourth-generation X-Ray CT scanner geometry. Previously in older generation scanners, the X-Ray beam was paired by a translating source and detector.
Ultrasound
Medical ultrasonography uses high frequency broadband sound waves in the megahertz range that are reflected by tissue to varying degrees to produce (up to 3D) images. This is commonly associated with imaging the fetus in pregnant women. Uses of ultrasound are much broader, however. Other important uses include imaging the abdominal organs, heart, breast, muscles, tendons, arteries and veins. While it may provide less anatomical detail than techniques such as CT or MRI, it has several advantages which make it ideal in numerous situations, in particular that it studies the function of moving structures in real-time, emits no ionizing radiation, and contains speckle that can be used in elastography. Ultrasound is also used as a popular research tool for capturing raw data, that can be made available through an Ultrasound research interface, for the purpose of tissue characterization and implementation of new image processing techniques. The concepts of ultrasound differ from other medical imaging modalities in the fact that it is operated by the transmission and receipt of sound waves. The high frequency sound waves are sent into the tissue and depending on the composition of the different tissues; the signal will be attenuated and returned at separate intervals. A path of reflected sound waves in a multilayered structure can be defined by an input acoustic impedance( Ultrasound sound wave) and the Reflection and transmission coefficients of the relative structures[6] . It is very safe to use and does not appear to cause any adverse effects, although information on this is not well documented. It is also relatively inexpensive and quick to perform. Ultrasound scanners can be taken to critically ill patients in intensive care units, avoiding the danger caused while moving the patient to the radiology department. The real time moving image obtained can be used to guide drainage and biopsy procedures. Doppler capabilities on modern scanners allow the blood flow in arteries and veins to be assessed.
Medical imaging topics
Maximizing imaging procedure use
The amount of data obtained in a single MR or CT scan is very extensive. Some of the data that radiologists discard could save patients time and money, while reducing their exposure to radiation and risk of complications from invasive procedures.[8]
Creation of three-dimensional images
Recently, techniques have been developed to enable CT, MRI and ultrasound scanning software to produce 3D images for the physician.[9] Traditionally CT and MRI scans produced 2D static output on film. To produce 3D images, many scans are made, then combined by computers to produce a 3D model, which can then be manipulated by the physician. 3D ultrasounds are produced using a somewhat similar technique. In diagnosing disease of the viscera of abdomen,ultrasound is particularly sensitive on imaging of biliary tract,urinary tract and female reproductive organs (ovary,fallopian tubes). As for example,diagnosis of gall stone by dilatation of common bile duct and stone in common bile duct . With the ability to visualize important structures in great detail, 3D visualization methods are a valuable resource for the diagnosis and surgical treatment of many pathologies. It was a key resource for the famous, but ultimately unsuccessful attempt by Singaporean surgeons to separate Iranian twins Ladan and Laleh Bijani in 2003. The 3D equipment was used previously for similar operations with great success.
Other proposed or developed techniques include:
- Diffuse optical tomography
- Elastography
- Electrical impedance tomography
- Optoacoustic imaging
- Ophthalmology
Some of these techniques are still at a research stage and not yet used in clinical routines.
Compression of medical images
Medical imaging techniques produce very large amounts of data, especially from CT, MRI and PET modalities. As a result, storage and communications of electronic image data are prohibitive without the use of compression. JPEG 2000 is the state-of-the-art image compression DICOM standard for storage and transmission of medical images. The cost and feasibility of accessing large image data sets over low or various bandwidths are further addressed by use of another DICOM standard, called JPIP, to enable efficient streaming of the JPEG 2000 compressed image data.
Non-diagnostic imaging
Neuroimaging has also been used in experimental circumstances to allow people (especially disabled persons) to control outside devices, acting as a brain computer interface.
Archiving and recording
Used primarily in ultrasound imaging, capturing the image produced by a medical imaging device is required for archiving and telemedicine applications. In most scenarios, a frame grabber is used in order to capture the video signal from the medical device and relay it to a computer for further processing and operations.[10]
Medical Imaging in the Cloud
There has been growing trend to migrate from PACS to a Cloud Based RIS. A recent article by Applied Radiology said, "As the digital-imaging realm is embraced across the healthcare enterprise, the swift transition from terabytes to petabytes of data has put radiology on the brink of information overload. Cloud computing offers the imaging department of the future the tools to manage data much more intelligently."[11]
Use in pharmaceutical clinical trials
Medical imaging has become a major tool in clinical trials since it enables rapid diagnosis with visualization and quantitative assessment.
A typical clinical trial goes through multiple phases and can take up to eight years. Clinical endpoints or outcomes are used to determine whether the therapy is safe and effective. Once a patient reaches the endpoint, he/she is generally excluded from further experimental interaction. Trials that rely solely on clinical endpoints are very costly as they have long durations and tend to need large number of patients.
In contrast to clinical endpoints, surrogate endpoints have been shown to cut down the time required to confirm whether a drug has clinical benefits. Imaging biomarkers (a characteristic that is objectively measured by an imaging technique, which is used as an indicator of pharmacological response to a therapy) and surrogate endpoints have shown to facilitate the use of small group sizes, obtaining quick results with good statistical power.[12]
Imaging is able to reveal subtle change that is indicative of the progression of therapy that may be missed out by more subjective, traditional approaches. Statistical bias is reduced as the findings are evaluated without any direct patient contact.
For example, measurement of tumour shrinkage is a commonly used surrogate endpoint in solid tumour response evaluation. This allows for faster and more objective assessment of the effects of anticancer drugs. In evaluating the extent of Alzheimer’s disease, it is still prevalent to use behavioural and cognitive tests. MRI scans on the entire brain can accurately pinpoint hippocampal atrophy rate while PET scans is able to measure the brain’s metabolic activity by measuring regional glucose metabolism.[12]
An imaging-based trial will usually be made up of three components:
- A realistic imaging protocol. The protocol is an outline that standardizes (as far as practically possible) the way in which the images are acquired using the various modalities (PET, SPECT, CT, MRI). It covers the specifics in which images are to be stored, processed and evaluated.
- An imaging centre that is responsible for collecting the images, perform quality control and provide tools for data storage, distribution and analysis. It is important for images acquired at different time points are displayed in a standardised format to maintain the reliability of the evaluation. Certain specialised imaging contract research organizations provide to end medical imaging services, from protocol design and site management through to data quality assurance and image analysis.
- Clinical sites that recruit patients to generate the images to send back to the imaging centre.
See also
- Preclinical imaging
- Cardiac PET
- Biomedical informatics
- Digital Imaging and Communications in Medicine
- Digital mammography
- eMix
- Fotofinder
- Full-body scan
- VoluMedic
- Magnetic field imaging
- Medical examination
- Medical radiography
- Medical test
- Neuroimaging
- Non-invasive (medical)
- Olea Medical
- PACS
- JPEG 2000 compression
- JPIP streaming
- Pneumoencephalogram
- Radiology information system
- Segmentation (image processing)
- Signal-to-noise ratio
- Society for Imaging Science and Technology
- Tomogram
- Virtopsy
- CellProfiler
- imageJ
- FIJI
- Endrov
- OpenCV
- GemIdent
- 3D Slicer
- ITK
- OsiriX
- MicroDicom
- FreeSurfer
- ClearCanvas
- Seg3D
- InVesalius
- FMRIB Software Library
- AFNI
- ITK
- ITK-SNAP
- VXL
Proprietary - Matlab
- Mathematica
- Bitplane
References
- ^ Roobottom CA, Mitchell G, Morgan-Hughes G (November 2010). "Radiation-reduction strategies in cardiac computed tomographic angiography". Clin Radiol 65 (11): 859–67. doi:10.1016/j.crad.2010.04.021. PMID 20933639.
- ^ "Medical Radiation Exposure Of The U.S. Population Greatly Increased Since The Early 1980s". http://www.sciencedaily.com/releases/2009/03/090303125809.htm.
- ^ Correlation of single photon emission CT with MR image data using fiduciary markers. BJ Erickson and CR Jack Jr., American Journal of Neuroradiology, Vol 14, Issue 3 713-720.
- ^ Society of Nuclear Medicine
- ^ thefreedictionary.com - scintigraphy Citing: Dorland's Medical Dictionary for Health Consumers, 2007 by Saunders; Saunders Comprehensive Veterinary Dictionary, 3 ed. 2007; McGraw-Hill Concise Dictionary of Modern Medicine, 2002 by The McGraw-Hill Companies
- ^ a b c Dhawan P, A. (2003). Medical Imaging Analysis. Hoboken, NJ: Wiley-Interscience Publication
- ^ http://www.breastthermography.com/breast_thermography_mf.htm
- ^ Freiherr G. Waste not, want not: Getting the most from imaging procedures. Diagnostic Imaging. March 19, 2010.
- ^ Udupa, J.K. and Herman, G. T., 3D Imaging in Medicine, 2nd Edition, CRC Press, 2000
- ^ Treating Medical Ailments in Real Time
- ^ Template:Applied Radiology
- ^ a b Hajnal, J. V., Hawkes, D. J., & Hill, D. L. (2001). Medical Image Registration. CRC Press.
External links
Medical testing : Medical imaging · Radiology · (ICD-9-CM V3 87-88, ICD-10-PCS B, CPT 70010-79999) X-ray/
medical radiography/
Industrial radiographyMedical: Pneumoencephalography · Dental radiography · Sialography · Myelography · CXR (Bronchography) · AXR / KUB · DXA/DXR · Upper gastrointestinal series/Small bowel follow-through/Lower gastrointestinal series · Cholangiography/Cholecystography · Mammography · Pyelogram · Cystography · Arthrogram · Hysterosalpingography · Skeletal survey · Angiography (Angiocardiography, Aortography) · Venography · Lymphogram
Industrial: Radiographic testingMedical: CT pulmonary angiogram · Cardiac CT · Abdominal and pelvic CT (Virtual colonoscopy) · CT angiography · CT head · pQCT · Spiral computed tomography · High resolution CT · Whole body imaging (Full-body CT scan) · Electron beam tomography
Industrial: Industrial CT ScanningOtherMRI MRI of brain and brain stem · MR neurography · Cardiac MRI/Cardiac MRI perfusion · MR angiography · MR cholangiopancreatography · Breast MRI
Functional MRI · Diffusion MRIUltrasound Echocardiography / Doppler echocardiography (TTE · TEE) · Intravascular · Gynecologic · Obstetric · Echoencephalography · Transcranial doppler · Abdominal ultrasonography · Transrectal · Breast ultrasound · Transscrotal ultrasound · Carotid ultrasonography
Contrast-enhanced · 3D ultrasound · Endoscopic ultrasound · Emergency ultrasound (FAST) · DuplexRadionuclide 2D / scintigraphyCholescintigraphy · Scintimammography · Ventilation/perfusion scan · Radionuclide ventriculography · Radionuclide angiography · Radioisotope renography · Sestamibi parathyroid scintigraphy · Radioactive iodine uptake test · Bone scintigraphy · Immunoscintigraphy
full body: Octreotide scan · Gallium 67 scan · Indium 111 WBC scan3D / ECTSPECT (gamma ray): SPECT of brain, Myocardial perfusion imaging
PET (positron): Brain PET, Cardiac PET, PET mammography, PET-CTOptical laser Thermography Breast thermography
Wikimedia Foundation. 2010.