- Obstetric ultrasonography
-
Obstetric ultrasonography Intervention 
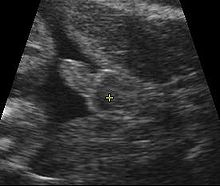
Obstetric sonogram of a fetus at 16 weeks. The bright white circle center-right is the head, which faces to the left. Features include the forehead at 10 o'clock, the left ear toward the center at 7 o'clock and the right hand covering the eyes at 9:00.ICD-9-CM 88.78 MeSH D016216 OPS-301 code: 3-032, 3-05d Obstetric sonography (ultrasonography) is the application of medical ultrasonography to obstetrics, in which sonography is used to visualize the embryo or foetus in its mother's uterus (womb). The procedure is often a standard part of prenatal care, as it yields a variety of information regarding the health of the mother and of the fetus, as well as regarding the progress of the pregnancy.
Contents
Types
Traditional obstetric sonograms are done by placing a transducer (a device that converts one type of energy into another) on the abdomen of the pregnant woman. One variant, a transvaginal sonography, is done with a probe placed in the woman's vagina. Transvaginal scans usually provide clearer pictures during early pregnancy and in obese women. Also used is Doppler sonography which detects the heartbeat of the fetus. Doppler sonography can be used to evaluate the pulsations in the fetal heart and bloods vessels for signs of abnormalities.[1]
Early pregnancy
The gestational sac can sometimes be visualized as early as four and a half weeks of gestation (approximately two and a half weeks after ovulation) and the yolk sac at about five weeks gestation. The embryo can be observed and measured by about five and a half weeks. The heartbeat may be seen as early as 6 weeks, and is usually visible by 7 weeks gestation.[1][2]
Dating and growth monitoring
Gestational age is usually determined by the date of the woman's last menstrual period, and assuming ovulation occurred on day fourteen of the menstrual cycle. Sometimes a woman may be uncertain of the date of her last menstrual period, or there may be reason to suspect ovulation occurred significantly earlier or later than the fourteenth day of her cycle. Ultrasound scans offer an alternative method of estimating gestational age. The most accurate measurement for dating is the crown-rump length of the fetus, which can be done between 7 and 13 weeks of gestation. After 13 weeks gestation, the fetal age may be estimated by the biparietal diameter (the transverse diameter of the head), the head circumference, the length of the femur (the longest bone in the body), and the many more fetal parameters that have been measured and correlated with age over the last 30 years. Dating is more accurate when done earlier in the pregnancy; if a later scan gives a different estimate of gestational age, the estimated age is not normally changed but rather it is assumed the fetus is not growing at the expected rate.[1]
Not useful for dating, the abdominal circumference of the fetus may also be measured. This gives an estimate of the weight and size of the fetus and is important when doing serial ultrasounds to monitor fetal growth.[1]
Fetal sex determination
The sex of the fetus can usually be determined by ultrasound at any time after 16 weeks, often at the dating scan around 20 weeks into the pregnancy depending upon the quality of the sonographic machine and skill of the operator. This is also the best time to have an ultrasound done as most infants are the same size at this stage of development[citation needed]. Depending on the skill of the sonographer, ultrasound may suffer from a high rate of false negatives and false positives. This means care has to be taken in interpreting the accuracy of the scan.
Ultrasonography of the cervix
Obstetric sonography has become useful in the assessment of the cervix in women at risk for premature birth. A short cervix preterm is undesirable: At 24 weeks gestation a cervix length of less than 25 mm defines a risk group for preterm birth, further, the shorter the cervix the greater the risk.[3] It also has been helpful to use ultrasonography in women with preterm contractions, as those whose cervix length exceed 30 mm are unlikely to deliver within the next week.[4]
Abnormality screening
In some countries, routine pregnancy sonographic scans are performed to detect developmental defects before birth. This includes checking the status of the limbs and vital organs, as well as (sometimes) specific tests for abnormalities. Some abnormalities detected by ultrasound can be addressed by medical treatment in utero or by perinatal care, though indications of other abnormalities can lead to a decision regarding abortion.
Perhaps the most common such test uses a measurement of the nuchal translucency thickness ("NT-test", or "Nuchal Scan"). Although 91% of fetuses affected by Down syndrome exhibit this defect, 5% of fetuses flagged by the test do not have Down syndrome.
Ultrasound may also detect fetal organ anomaly. Usually scans for this type of detection are done around 18 to 20 weeks of gestational age.
History
Scottish physician Ian Donald was one of the pioneers of medical use of ultrasound. His article "Investigation of Abdominal Masses by Pulsed Ultrasound" was published in The Lancet in 1958. Donald was Regius Professor of Midwifery at the University of Glasgow.[5]
In 1962, after about two years of work, Joseph Holmes, William Wright, and Ralph Meyerdirk developed the first compound contact B-mode scanner. Their work had been supported by U.S. Public Health Services and the University of Colorado. Wright and Meyerdirk left the university to form Physionic Engineering Inc., which launched the first commercial hand-held articulated arm compound contact B-mode scanner in 1963.[6] This was the start of the most popular design in the history of ultrasound scanners.
Obstetric ultrasound has played a significant role in the development of diagnostic ultrasound technology in general. Much of the technological advances in diagnostic ultrasound technology are due to the drive to create better obstetric ultrasound equipment. Acuson Corporation's pioneering work on the development of Coherent Image Formation helped shape the development of diagnostic ultrasound equipment as a whole.
Safety issues
Current evidence indicates that diagnostic ultrasound is safe for the unborn child, unlike radiographs, which employ ionizing radiation. However, no randomized controlled trials have been undertaken to test the safety of the technology, and thus ultrasound procedures are generally not done repeatedly unless medically indicated.
A 2006 study on genetically modified mice exposed to ultrasound (5-240 minutes a day) showed neurological changes in the exposed fetuses. Some of the rodent brain cells failed to migrate to their proper position and remained scattered in incorrect parts of the brain.[7]
It has been shown that Low Intensity Pulsed Ultrasound does have a localized effect on growth in human beings. The 1985 maximum power allowed by the U.S. Food and Drug Administration (FDA) of 180 milliwatts per square cm [8] is well under the levels used in therapeutic ultrasound, but still higher than the 30-80 milliwatts per square cm range of the Statison V veterinary LIPUS device.[9] LIPUS has been shown to affect tissue growth in as little as 20 minutes of time with repeated daily applications. Adding to the similarity, LIPUS and medical ultrasound both operate in the 1 to 10 MHz range.
While the benefits of medical ultrasound outweigh any risks, vanity uses such as making 3D ultrasound movies without a doctor's order present a possibly unnecessary, but unknown risk to a developing fetus. The FDA discourages its use for non-medical purposes such as fetal keepsake videos and photos, even though it is the same technology used in hospitals. The demand for keepsake ultrasound products in medical environments has prompted commercial solutions such as self-serve software that allows the patient to create a "keepsake" from the ultrasound imagery recorded during a medical ultrasound procedure.[10]
See also
- Doppler fetal monitor
- Gynecologic ultrasonography
- 3D Ultrasound
- Global Library of Women's Medicine
References
- ^ a b c d Woo, Joseph (2006). "Why and when is Ultrasound used in Pregnancy?". Obstetric Ultrasound: A Comprehensive Guide. http://www.ob-ultrasound.net/. Retrieved 2007-05-27.
- ^ Boschert, Sherry (2001-06-15). "Anxious Patients Often Want Very Early Ultrasound Exam". OB/GYN News (FindArticles.com). http://findarticles.com/p/articles/mi_m0CYD/is_12_36/ai_76636730. Retrieved 2007-05-27.
- ^ Iams JD, Goldenberg RL, Meis PJ, et al. (February 1996). "The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network". N. Engl. J. Med. 334 (9): 567–72. doi:10.1056/NEJM199602293340904. PMID 8569824. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=8569824&promo=ONFLNS19.
- ^ Leitich H, Brunbauer M, Kaider A, Egarter C, Husslein P (December 1999). "Cervical length and dilatation of the internal cervical os detected by vaginal ultrasonography as markers for preterm delivery: A systematic review". Am. J. Obstet. Gynecol. 181 (6): 1465–72. doi:10.1016/S0002-9378(99)70407-2. PMID 10601930.
- ^ Ian Donald's paper in the Lancet in 1958 by Joseph Woo
- ^ Woo, Joseph (2002). "A short History of the development of Ultrasound in Obstetrics and Gynecology". ob-ultrasound.net. http://www.ob-ultrasound.net/history1.html. Retrieved 2007-08-26.
- ^ Ang ES, Gluncic V, Duque A, Schafer ME, Rakic P (2006). "Prenatal exposure to ultrasound waves impacts neuronal migration in mice". Proc. Natl. Acad. Sci. U.S.A. 103 (34): 12903–10. Bibcode 2006PNAS..10312903A. doi:10.1073/pnas.0605294103. PMC 1538990. PMID 16901978. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1538990. Retrieved 2007-05-28.
- ^ expressed as 1800 watts per m^2
- ^ http://www.statison.com/html/Statison_V_User_Guide.pdf[dead link]
- ^ "Fetal Keepsake Videos". Food and Drug Administration. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PatientAlerts/ucm064756.htm. Retrieved 2011-05-21.
External links
- RadiologyInfo: Obstetric Ultrasound Imaging
- AIUM statement on prudent use of Ultrasound
- The Global Library of Women's Medicine Imaging in Obstetrics and Gynecology link
Pregnancy and childbirth Planning Conception Testing Prenatal AnatomyProceduresChildbirth PreparationRolesDeliveryPostpartum Obstetric history Obstetrical surgery and other procedures (ICD-9-CM V3 72-75, ICD-10-PCS 1) Diagnostic sampling: fetal tissue (Chorionic villus sampling · Amniocentesis) · blood (Triple test · Percutaneous umbilical cord blood sampling · Apt test · Kleihauer-Betke test) · Lecithin-sphingomyelin ratio · Fetal fibronectin test
obstetric ultrasonography: Nuchal scan · Biophysical profile (Amniotic fluid index)
other medical imaging: Fetoscopy
Cardiotocography · (Nonstress test) · Vibroacoustic stimulation
challenge: Contraction stress test
Leopold's maneuversIntervention Delivery Vaginal deliveryInduction (Artificial rupture of membranes/Amniotomy) · Episiotomy · Symphysiotomy · Forceps in childbirth · Ventouse in childbirth
shoulder dystocia (McRoberts maneuver, Woods' screw maneuver, Zavanelli maneuver) · Manual placenta removalPostpartum hemorrhageCategories:- Obstetrical procedures
- Pregnancy tests
- Medical ultrasound
Wikimedia Foundation. 2010.