- Fallopian tube obstruction
-
Fallopian tube obstruction Classification and external resources 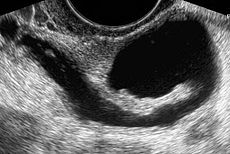
The presence of a hydrosalpinx by sonography indicates distal tubal obstructionICD-10 N97.1 ICD-9 628.2 Fallopian tube obstruction is a major cause of female infertility. Blocked fallopian tubes are unable to let the ovum and the sperm converge, thus making fertilization impossible. Fallopian Tubes are also known as oviducts, uterine tubes, and salpinges (singular salpinx).
Contents
Types
About 20% of female infertility can be attributed to tubal causes.[1] Distal tubal occlusion (affecting the end towards the ovary) is typically associated with hydrosalpinx formation and often caused by Chlamydia trachomatis.[1] Pelvic adhesions may be associated with such an infection. In less severe forms, the fimbriae may be aggluntinated and damaged, but some patency may still be preserved. Midsegment tubal obstruction can be due to tubal ligation procedures as that part of the tube is a common target of sterilization interventions. Proximal tubal occlusion can occur after infection such as a septic abortion. Also, some tubal sterilization procedures such as the Essure procedure target the part of the tube that is close to the uterus..
Causes
Most commonly a tube may be obstructed due to infection such as pelvic inflammatory disease (PID). The rate of tubal infertility has been reported to be 12% after one, 23% after two, and 53% after three episodes of PID.[1] The Fallopian tubes may also be occluded or disabled by endometritis, infections after childbirth and intraabdominal infections including appendicitis and peritonitis. The formation of adhesions may not necessarily block a fallopian tube, but render it dysfunctional by distorting or separating it from the ovary. It has been reported that women with distal tubal occlusion have a higher rate of HIV infection.[2]
Fallopian tubes may be blocked as a method of contraception. In these situations tubes tend to be healthy and typically patients requesting the procedure had children. While tubal ligation is considered a permanent procedure, some patients later regret their decision and want the procedure "undone".
Evaluation
While a full testing of tubal functions in patients with infertility is not possible, testing of tubal patency is feasible. A hysterosalpingogram will demonstrate that tubes are open when the radioopaque dye spills into the abdominal cavity. Sonography can demonstrate tubal abnormalities such as a hydrosalpinx indicative of tubal occlusion. During surgery, typically laparoscopy, the status of the tubes can be inspected and a dye such as methylene blue can be injected in a process termed chromotubation into the uterus and shown to pass through the tubes when the cervix is occluded. Laparoscopic chromotubation has ben described as the gold standard of tubal evaluation.[3] As tubal disease is often related to Chlamydia infection, testing for Chlamydia antibodies has become a cost-effective screening device for tubal pathology.[3]
Tubal insufflation is only of historical interest as an older office method to indicate patency;[4] it was used prior to laparoscopic evaluation of pelvic organs.
Treatment
Traditionally Fallopian tubal surgery (tuboplasty) was used to restore patency to the tubes and thus possibly normal function. However, in most situations today, in vitro fertilization is used to overcome tubal infertility as it is more cost-effective, less invasive, and results are immediate. With IVF, after stimulation of ovarian follicles, egg cells are removed via a sonographic directed vaginal puncture into the ovary, these eggs are fertiized outside the body, and the resultant embryo placed transcervically into the uterus; - the tubes are bypassed in this process.
Different types of tuboplasty have been developed and can be applied by laparoscopy or laparotomy. They include lysis of adhesions, fimbrioplasty (repairing the fimbriated end of the tubes), salpinostomy (creating an opening for the tube), resection and reananstomosis (removing a piece of blocked tube and reuniting the remaining patent parts of the tube), and tubal reimplantation (reconnecting the tube to the uterus). Further, using fluoroscopy or hysteroscopy proximal tubal occlusion can be overcome by transcervical catheter recanalization[5] or falloposcopy.
Results of tubal surgery are inversely related to damage that exists prior to surgery.[6] Development of adhesions remains a problem.[1] Patients with operated tubes are at increased risk for ectopic pregnancy.[6]
Surgical repair of fallopian tubes that have been occluded by a sterilization procedure generally have good success rates provided enough healthy tubal tissue is present for the surgeon to perform a tubal reversal.
While IVF therapy has largely replaced tubal surgery in the treatment of infertility, the presence of hydrosalpinx is an detriment to IVF success. It has been recommended that prior to IVF, laparoscopic surgery should be done to either block or remove hydrosalpinges.[7]
References
- ^ a b c d Yen SSC, Jaffe RB, Barbieri RL. Reproductive Endocrinology, 4th Ed.. W. B. Saunders Co, 1999. ISBN 0-7216-6897-6.
- ^ Adesiyun AG, Ameh CA, Eka A. (2008). "Hysterosalpingographic tubal abnormalities and HIV infection among black women with tubal infertility in sub-Saharan Africa.". Gynecol Obstet Invest. 2008;66(2):119-22. 66 (2): 119–22. doi:10.1159/000128600. PMID 18446041.
- ^ a b Kodaman PH, Arici A, Seli E. (2004). "Evidence-based diagnosis and management of tubal factor infertility". Curr Opin Obstet Gynecol. 2004 Jun;16(3):221-9. 16 (3): 221–9. PMID 15129051.
- ^ Speert H (February 2007,). "Memorable Medical Mentors: XVII: Isidor C. Rubin (1883–1958)". Obstetrical & Gynecological Survey 62 (2): 77–81. doi:10.1097/01.ogx.0000248809.19623.96.
- ^ Sulak PJ, Letterie GS, Hayslip CC, Coddington CC, Klein TA. (1987). "Hysteroscopic cannulation and lavage in the treatment of proximal tubal occlusion". Steril Fertil 48:493-4, 1987 48 (3): 493–4. PMID 2957240.
- ^ a b Mossa B, Patella A, Ebano V, Pacifici E, Mossa S, Marziani R. (2005). "Microsurgery versus laparoscopy in distal tubal obstruction hysterosalpingographically or laparoscopically investigated". Clin Exp Obstet Gynecol. 2005;32(3):169-71. 32 (3): 169–71. PMID 16433156.
- ^ Johnson N, van Voorst S, Sowter MC, Strandell A, Mol BW. (2010). Johnson, Neil. ed. "Surgical treatment for tubal disease in women due to undergo in vitro fertilisation". Cochrane Database Syst Rev. 2010 Jan 20;(1):CD002125. (1): CD002125. doi:10.1002/14651858.CD002125.pub3. PMID 20091531.
Female diseases of the pelvis and genitals (N70–N99, 614–629) Internal AdnexaOophoritis · Ovarian cyst (Follicular cyst of ovary, Corpus luteum cyst, Theca lutein cyst) · Endometriosis of ovary · Ovarian hyperstimulation syndrome · Ovarian torsion · Ovarian apoplexy · Mittelschmerz · Female infertility (Anovulation, Poor ovarian reserve)Cervicitis · Cervical polyp · Nabothian cyst · Cervical incompetence · Female infertility (Cervical stenosis) · Cervical dysplasiaGeneralVaginitis (Bacterial vaginosis, Atrophic vaginitis, Candidal vulvovaginitis) · Leukorrhea/Vaginal discharge · Hematocolpos/HydrocolposOther/generalPelvic inflammatory disease · Pelvic congestion syndromeExternal Categories:- Noninflammatory disorders of female genital tract
Wikimedia Foundation. 2010.
