- Cladribine
-
Cladribine 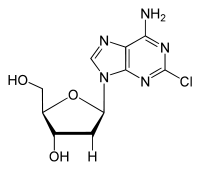
Systematic (IUPAC) name 5-(6-amino-2-chloro-purin-9-yl)-2-(hydroxymethyl)oxolan-3-ol Clinical data AHFS/Drugs.com monograph MedlinePlus a693015 Pregnancy cat. D(US) Legal status ℞-only (US) Routes Intravenous, subcutaneous, oral Pharmacokinetic data Bioavailability 100% (i.v.) Protein binding 20% Half-life 5.4 hours Identifiers CAS number 4291-63-8 ATC code L01BB04 PubChem CID 20279 DrugBank APRD00260 ChemSpider 19105 
UNII 47M74X9YT5 
KEGG D01370 
ChEBI CHEBI:567361 
ChEMBL CHEMBL1619 
Chemical data Formula C10H12ClN5O3 Mol. mass 285.687 g/mol SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Cladribine (trade names Litak and Movectro) is a drug used to treat hairy cell leukemia (HCL, leukemic reticuloendotheliosis) and multiple sclerosis. Its chemical name is 2-chlorodeoxyadenosine (2CDA).
As a purine analog, it is a synthetic anti-cancer agent that also suppresses the immune system. Chemically, it mimics the nucleoside adenosine and thus inhibits the enzyme adenosine deaminase, which interferes with the cell's ability to process DNA. It is easily destroyed by normal cells except for blood cells, with the result that it produces relatively few side effects and results in very little non-target cell loss.
Contents
Indications
Cladribine (as injections) is indicated [approved] for the treatment of symptomatic hairy cell leukemia.[1]
It is under investigation for other B cell leukemias and lymphomas, such as mantle cell lymphoma,[2] and for use in the treatment of multiple sclerosis.
According to the Histiocytosis Association of America, cladribine is used to treat histiocytosis.[3]
Multiple sclerosis
In January 2010, a large clinical trial involving more than 1000 patients documented significant reduction in relapse rates in multiple sclerosis patients with use of oral cladribine and thus making its use as the first oral medication in multiple sclerosis patients, most likely in year [2011].[4]
Russia was the first country to approve it for use treating multiple sclerosis on July 12, 2010.[5] In the European Union, the European Medicines Agency's CHMP did not approve cladribine in the first application, as did the U.S. Food and Drug Administration (FDA).[6] As of March 2, 2011, the FDA has rejected oral cladribine for multiple sclerosis,[7] "acknowledging sufficient data on the drug’s efficacy in multiple sclerosis but requiring more data on safety and risk-benefit " [8]
June 2011 : Merck has decided to withdraw all marketing applications for cladribine tablets, and to stop selling it in Russia and Australia which had approved it.[9]
Routes of administration
For hairy cell leukemia, cladribine can be given by i.v. infusion or subcutaneous (s.c.) injection.
For outpatient i.v. infusions, the delivery time (not including time to place the i.v. line) may range from one to four hours; two hours is most common. Continuous i.v. infusion may be chosen; this approach drips in the cladribine slowly, 24 hours a day using a portable pump and a central venous catheter or a PICC line. By contrast, s.c. injections take less than ten seconds per day.
The same total doses are given by both routes. Intravenous and s.c. routes have the same overall outcomes, and the s.c. route may be reduce the infections and other risks associated with venipuncture.[10]
An oral tablet form of cladribine has been successfully tested in patients with relapsing multiple sclerosis.[11]
Treatment schedule
Using either i.v. or s.c. routes of administration, cladribine can be administered on a daily or a weekly schedule. Daily schedules involve one s.c. injection or one i.v. infusion per day for five to seven consecutive days. Weekly schedules involve one injection or infusion each week, for five or six weeks. One cycle is normally sufficient to produce a complete response, but in the event of a partial response, cycles may safely be repeated one to three months after the end of the first cycle.
Actual doses are calculated according to the surface area of the patient's skin instead of by weight, and divided by the number of planned treatments.
All schedules produce the same benefits and disadvantages. Five-day and seven-day daily schedules give the same total amount of drug and have the same outcomes, including remissions and adverse effects.[12] Daily and weekly schedules give the same total amount of drug and have the same outcomes, including similar proportions of complete responses and similar proportions of patients hospitalized for fevers and opportunistic infections.[13]
Adverse effects
Existing studies estimate that from 18%[14] to 42%[15] of patients will experience a fever after cladribine infusion. This is usually a transient fever which can be treated with acetaminophen (paracetamol).[16] These fevers, which resolve in less than 48 hours,[17] have no evidence of being related to infection.
However, some patients have fevers that last longer and may be caused by an infection.[17][18] Very few infections have actually been documented,[15] but they do happen, and these infections are largely responsible for the 3% mortality rate associated with cladribine therapy in HCL.[19] Factors that increased the likelihood of a neutropenic fever (with or without concomitant infection) include: anemia, hypocholesterolemia, a high proportion of hairy cells in the bone marrow with a low proportion of myelopoietic cells, low albumin, and high C-reactive protein. These are all signs of an advanced case of HCL.
In patients with hairy cell leukemia, there is no benefit to using hormones such as filgrastim or Granulocyte macrophage colony-stimulating factor to raise white blood cell counts prophylactically.[15][19] The use of these expensive drugs does not reduce the number of patients who experience fevers, the number of days that the fevers last, or the number of patients admitted to the hospital for antibiotic treatments.[15] Therefore routine adjunctive use (that is, use when there are no signs of infection) is not recommended.[15]
In addition to fevers, cladribine increases the risk of herpes virus infections, particularly shingles.[14]
Some patients develop a rash after treatment. Nearly all patients who develop a rash are taking other drugs, notably allopurinol or a sulfa drug, which are known to cause rashes, and the rash is likely due to these drugs rather than to cladribine itself.[20]
Some HCL patients will require blood transfusions of platelets or packed red blood cells.[12]
Patients are expected to experience a decline in blood cell counts during treatment. Several weeks after successful treatment, cell counts will begin to rebound, with platelet and neutrophil counts recovering before red blood cells and T cells. T4 cell counts may never reach pre-disease levels. Patients are usually advised to avoid sick people and large crowds of people as well as to wash their hands and keep their hands away from their eyes, nose, and mouth until their neutrophil counts have recovered.
Many patients experience fatigue, even in the absence of anemia, but since fatigue is a common feature of the disease, this may be caused by the disease instead of by the drug.
This drug does not cause hair loss, vomiting, or other side effects that are commonly associated with "old style" alkylating chemotherapy drugs. However, peripheral neuropathy has been reported occasionally after repeated doses of cladribine in the treatment of hairy cell leukemia. Overdose may cause kidney damage.
Response
According to the drug's FDA-approved prescribing information,[20] the median time to normalization of blood counts in patients with hairy cell leukemia is: two weeks for platelets, five weeks for absolute neutrophil counts, eight weeks for hemoglobin, and nine weeks for a patient to have all three parameters normalized. Weeks are counted from the first day of treatment, and all patients were on a seven-day daily treatment schedule for these studies.
History
Cladribine was designed by Dennis A. Carson as an anti-lymphocyte compound.[21] It was first synthesized at Brigham Young University.[22]
In 2008, Ernest Beutler won the Wallace H. Coulter Award for Lifetime Achievement in Hematology from the Coulter Foundation and the American Society of Hematology in part because of the clinical trials he ran, which established cladribine as the most effective treatment for hairy cell leukemia (HCL).[21]
References
- ^ Else M, Dearden CE, Matutes E, et al. (March 2009). "Long-term follow-up of 233 patients with hairy cell leukaemia, treated initially with pentostatin or cladribine, at a median of 16 years from diagnosis". Br. J. Haematol. 145 (6): 733–40. doi:10.1111/j.1365-2141.2009.07668.x. PMID 19344416.
- ^ Mantle Cell Lymphoma initiative
- ^ Histiocytosis Association of America
- ^ Giovannoni G, et al., NEJM 2010
- ^ Hirschler, Ben (July 12, 2010). "UPDATE 1-Russia okays Merck KGaA's multiple sclerosis pill". Reuters. http://www.reuters.com/article/idCNLDE66B0GB20100712?rpc=44.
- ^ http://www.n-tv.de/wirtschaft/Merck-erleidet-herben-Schlag-article1561811.html
- ^ http://www.medscape.com/viewarticle/738239
- ^ "Oral Multiple Sclerosis Therapies Spark Excitement, Concern" Internal Medicine News, April, 2011. [1]
- ^ http://www.genengnews.com/gen-news-highlights/merck-serono-gives-up-on-getting-drug-candidate-for-multiple-sclerosis-approved/81245334/
- ^ von Rohr A, Schmitz SF, Tichelli A, et al. (2002). "Treatment of hairy cell leukemia with cladribine (2-chlorodeoxyadenosine) by subcutaneous bolus injection: a phase II study". Ann. Oncol. 13 (10): 1641–9. doi:10.1093/annonc/mdf272. PMID 12377655. http://annonc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12377655.
- ^ Cladribine Tablets for Multiple Sclerosis Significantly Reduced Relapse Rate in Two-Year Phase III Pivotal Trial
- ^ a b Aurer I, Mitrović Z, Kovacević-Metelko J, et al. (2007). "[Treatment of hairy cell leukemia with cladribine]" (in Croatian). Lijec Vjesn 129 (3–4): 80–3. PMID 17557550.
- ^ Robak T, Jamroziak K, Gora-Tybor J, et al. (2007). "Cladribine in a weekly versus daily schedule for untreated active hairy cell leukemia: final report from the Polish Adult Leukemia Group (PALG) of a prospective, randomized, multicenter trial". Blood 109 (9): 3672–5. doi:10.1182/blood-2006-08-042929. PMID 17209059. http://www.bloodjournal.org/cgi/pmidlookup?view=long&pmid=17209059.
- ^ a b Van Den Neste E, Delannoy A, Vandercam B, et al. (1996). "Infectious complications after 2-chlorodeoxyadenosine therapy". Eur. J. Haematol. 56 (4): 235–40. doi:10.1111/j.1600-0609.1996.tb01935.x. PMID 8641392.
- ^ a b c d e Saven A, Burian C, Adusumalli J, Koziol JA (1999). "Filgrastim for cladribine-induced neutropenic fever in patients with hairy cell leukemia". Blood 93 (8): 2471–7. PMID 10194424. http://www.bloodjournal.org/cgi/pmidlookup?view=long&pmid=10194424.
- ^ Nelson MC, Hogan DK (1995). "The role of cladribine in the treatment of lymphoid malignancies". Oncol Nurs Forum 22 (9): 1395–400. PMID 8539180.
- ^ a b Lauria F, Benfenati D, Raspadori D, et al. (1994). "Retreatment with 2-CdA of progressed HCL patients". Leuk. Lymphoma 14 Suppl 1: 143–5. PMID 7820047.
- ^ Lauria F, Benfenati D, Raspadori D, Rondelli D, Zinzani PL, Tura S (1993). "High complete remission rate in hairy cell leukemia treated with 2-chlorodeoxyadenosine". Leuk. Lymphoma 11 (5–6): 399–404. doi:10.3109/10428199309067932. PMID 7907247.
- ^ a b Juliusson G, Lenkei R, Tjønnfjord G, Heldal D, Liliemark J (April 1995). "Neutropenic fever following cladribine therapy for symptomatic hairy-cell leukemia: predictive factors and effects of granulocyte-macrophage colony-stimulating factor". Ann. Oncol. 6 (4): 371–5. PMID 7619752. http://annonc.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=7619752.
- ^ a b "Leustatin prescribing information" (PDF). Ortho Biotech Products, L.P. (a subsidiary of Johnson & Johnson. August 2007 revision. http://www.orthobiotech.com/orthobiotech/shared/OBI/PI/Leustatin_PI.pdf.
- ^ a b Lichtman, Marshall A., Josef Prchal, and Karl Blume (1 January 2008). "Wallace H. Coulter Award for Lifetime Achievement in Hematology: Inaugural Award Winner Ernest Beutler, MD". The Hematologist (American Society of Hematology). http://www.hematology.org/Publications/Hematologist/2008/1359.aspx.
- ^ Sneader, Walter (2005). Drug discovery: a history. New York: Wiley. pp. 258. ISBN 0-471-89979-8.
Categories:- Orphan drugs
- Antineoplastic antimetabolites
- Purines
- Organochlorides
Wikimedia Foundation. 2010.
