- Hydroxycarbamide
-
Hydroxycarbamide 
Systematic (IUPAC) name hydroxyurea Clinical data Trade names Apo-Hydroxyurea, Droxia, Hydrea AHFS/Drugs.com International Drug Names MedlinePlus a682004 Pregnancy cat. D (USA) Legal status ? Routes Oral Pharmacokinetic data Metabolism Liver Half-life 3-4 hours Excretion Renal and lungs Identifiers CAS number 127-07-1 
ATC code L01XX05 PubChem CID 3657 DrugBank APRD00023 ChemSpider 3530 
UNII X6Q56QN5QC 
KEGG D00341 
ChEBI CHEBI:44423 
ChEMBL CHEMBL467 
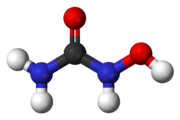
Chemical data Formula CH4N2O2 Mol. mass 76.0547 g/mol SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Hydroxycarbamide (INN) or hydroxyurea (brand names include Hydrea and Droxia) is an antineoplastic drug, first synthesized in 1869, used in myeloproliferative disorders, specifically polycythemia vera and essential thrombocythemia. It is also used to reduce the rate of painful attacks in sickle-cell disease and has antiretroviral properties in diseases such as AIDS.
Contents
Mechanism of action
One mechanism of action is thought to be based on its reduction of production of deoxyribonucleotides[1] via inhibition of the enzyme ribonucleotide reductase by scavenging tyrosyl free radicals as they are involved in the reduction NDPs.[2]
In the treatment of sickle-cell disease, hydroxycarbamide increases the concentration of fetal hemoglobin. The precise mechanism of action is not yet clear, but it appears that hydroxycarbamide increases nitric oxide levels, causing soluble guanylyl cyclase activation with a resultant rise in cyclic GMP, and the activation of gammaglobin synthesis necessary for fetal hemoglobin (by removing the rapidly dividing cells that preferentially produce sickle hemoglobin).[2][3]
Uses
Hydroxycarbamide is used for the following indications:
- Myeloproliferative disease (primarily polycythemia vera and essential thrombocytosis[4])
- Sickle-cell disease[5] (breaks down cells that are prone to sickle, as well as increasing fetal hemoglobin content)
- AIDS as an adjunct to ddI in combination antiretroviral therapies[6]
- Second line treatment for psoriasis[7] (slows down the rapid division of skin cells)
- Biochemical research as a DNA replication inhibitor[8] that causes deoxyribonucleotide depletion and results in DNA double strand breaks near replication forks (see DNA repair)
- Treatment for systemic mastocytosis[citation needed]
Dose
The dose depends on the indication, but tends to be 500 milligrams once a day when treatment is initiated. In myeloproliferative disease, further increases are determined by the response of the cell count and whether myelosuppression (decreased production of other blood cells) develops.[citation needed]
In sickle-cell disease, the initial daily dose is 15 mg per kilogram body weight (or less in reduced kidney function); after two weeks, a fall in the hemoglobin and platelet count and an increase in MCV (mean corpuscular volume) (size of the red blood cells) is to be expected. The dose is then increased every two weeks with monitoring of the full blood count until the dose is either 35 mg/kg or cytopenias develop.[2]
Side effects
Reported side-effects are: drowsiness, nausea, vomiting and diarrhea, constipation, mucositis, anorexia, stomatitis, bone marrow toxicity (which may take 7–21 days to recover after the drug has been discontinued), alopecia (hair loss), skin changes, abnormal liver enzymes, creatinine and blood urea nitrogen.[9]
Due to its effect on the bone marrow, regular monitoring of the full blood count is vital, as well as early response to possible infections. In addition, renal function, uric acid and electrolytes, as well as liver enzymes, are commonly checked.[citation needed]
Hydroxycarbamide has been used primarily for the treatment of myeloproliferative diseases, which has an inherent risk of transforming to acute myeloid leukemia. There has been a longstanding concern that hydroxycarbamide itself carries a leukemia risk, but large studies have shown that the risk is either absent or very small. Nevertheless, it has been a barrier for its wider use in patients with sickle-cell disease.[2]
Contraindications
Contraindications are: severe anemia, neutropenia.[citation needed]
Use in pregnancy
Category D - investigational or post-marketing data show risk to the fetus. However, potential benefits may outweigh the potential risk. Generally this rating is reserved for drugs with no safer alternatives.[9]
Synthesis
Hydroxyurea was first synthesized in 1869 by Dresler and Stein from hydroxylamine and hydrogen cyanate; the industrial process is analogous.[10] Hydroxyurea may also be synthesized by reaction of ethyl carbamate with hydroxylamine; hydroxylamine displaces the ester to give the amide.[11]
References
- ^ "hydroxyurea" at Dorland's Medical Dictionary
- ^ a b c d Platt OS (2008). "Hydroxyurea for the treatment of sickle cell anemia". N. Engl. J. Med. 358 (13): 1362–9. doi:10.1056/NEJMct0708272. PMID 18367739.
- ^ Cokic VP, Smith RD, Beleslin-Cokic BB, et al. (2003). "Hydroxyurea induces fetal hemoglobin by the nitric oxide-dependent activation of soluble guanylyl cyclase". J Clin Invest 111 (2): 231–9. doi:10.1172/JCI16672. PMC 151872. PMID 12531879. http://www.jci.org/articles/view/16672. Full text at PMC: 151872
- ^ Harrison CN, Campbell PJ, Buck G, et al. (July 2005). "Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia". N. Engl. J. Med. 353 (1): 33–45. doi:10.1056/NEJMoa043800. PMID 16000354. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=16000354&promo=ONFLNS19.
- ^ Lanzkron S, Strouse JJ, Wilson R, et al. (June 2008). "Systematic review: Hydroxyurea for the treatment of adults with sickle cell disease". Ann. Intern. Med. 148 (12): 939–55. PMID 18458272.
- ^ Frank I, Bosch RJ, Fiscus S, et al. (September 2004). "Activity, safety, and immunological effects of hydroxyurea added to didanosine in antiretroviral-naive and experienced HIV type 1-infected subjects: a randomized, placebo-controlled trial, ACTG 307". AIDS Res. Hum. Retroviruses 20 (9): 916–26. doi:10.1089/aid.2004.20.916. PMID 15597521.
- ^ Sharma VK, Dutta B, Ramam M (2004). "Hydroxyurea as an alternative therapy for psoriasis". Indian J Dermatol Venereol Leprol 70 (1): 13–7. PMID 17642550. http://www.ijdvl.com/article.asp?issn=0378-6323;year=2004;volume=70;issue=1;spage=13;epage=17;aulast=Sharma.
- ^ Koç A, Wheeler LJ, Mathews CK, Merrill GF (January 2004). "Hydroxyurea arrests DNA replication by a mechanism that preserves basal dNTP pools". J. Biol. Chem. 279 (1): 223–30. doi:10.1074/jbc.M303952200. PMID 14573610. http://www.jbc.org/cgi/pmidlookup?view=long&pmid=14573610.
- ^ a b Liebelt, E.; Balk, S.; Faber, W.; Fisher, J.; Hughes, C.; Lanzkron, S.; Lewis, K.; Marchetti, F. et al. (2007). "NTP-CERHR expert panel report on the reproductive and developmental toxicity of hydroxyurea". Birth defects research. Part B, Developmental and reproductive toxicology 80 (4): 259–366. doi:10.1002/bdrb.20123. PMID 17712860.
- ^ Lunghi, A; Aloni, C; Gigante, L; Mazzei, N; Cardillo, P (2002). "Hydroxyurea explosion: a thermoanalytical and calorimetric study". Journal of Loss Prevention in the Process Industries 15 (6): 489–495. doi:10.1016/S0950-4230(02)00044-X.
- ^ R. Deghenghi (1973), "Hydroxyurea", Org. Synth., http://www.orgsyn.org/orgsyn/orgsyn/prepContent.asp?prep=cv5p0645; Coll. Vol. 5: 645
Antiviral drugs: antiretroviral drugs used against HIV (primarily J05) Entry/fusion inhibitors
(Discovery & development)Reverse-transcriptase
inhibitors (RTIs)Nucleoside analogues/NARTIs: Abacavir (ABC)°# • Emtricitabine (FTC)°# • Lamivudine (3TC)°# • Didanosine (ddI)# • Zidovudine (AZT)# • Apricitabine† • Stampidine† • Elvucitabine† • Racivir† • Amdoxovir†• Stavudine (d4T)# • Zalcitabine (ddC)◊ • Festinavir†
Nucleotide analogues/NtRTIs: Tenofovir°# • GS 7340Non-Nucleoside (NNRTI)
(Discovery & development)(1st generation) Efavirenz°# • Nevirapine# • Loviride◊ • Delavirdine◊ •
(2nd generation) diarylpyrimidines (Etravirine, Rilpivirine) • Lersivirine†Integrase inhibitors Maturation inhibitors Protease Inhibitors (PI)
(Discovery and development)1st generation2nd generationCombined formulations Lamivudine/zidovudine • Emtricitabine/tenofovir/efavirenz • Abacavir/lamivudine/zidovudine • Tenofovir/emtricitabine • Lopinavir/ritonavir • Abacavir/lamivudine • Emtricitabine/rilpivirine/tenofovirExperimental agents TRIM5alpha (gene)Tat antagonistsTrichosanthinOtherAbzyme • Calanolide A • Ceragenin • Cyanovirin-N • Diarylpyrimidines • Epigallocatechin gallate (EGCG) • Foscarnet • Griffithsin • Hydroxycarbamide • Miltefosine • Portmanteau inhibitors • Seliciclib† • Synergistic enhancers • Tre recombinase • Zinc finger protein transcription factor • KP-1461† • Cobicistat†Failed agents#WHO-EM. ‡Withdrawn from market. Clinical trials: †Phase III. §Never to phase III °DHHS preferred first-line agent. ◊Formerly or rarely used agent.Categories:- Ureas
- Antineoplastic antimetabolites
Wikimedia Foundation. 2010.
