- Cancer pain
-
Pain is a symptom frequently associated with cancer. Cancer can cause pain by irritating or damaging nerves, by stimulating nociceptors (pain sensitive nerve fibers), or by releasing chemicals that make nociceptors respond to normally non-painful stimuli. Cancer pain may be caused by the tumor itself or by medical interventions in the diagnosis and treatment of cancer. Pain can be eliminated or well controlled in 80–90% of cases, but nearly one in two patients receives less-than-optimal care.
Contents
Pain
Main article: PainThe sensation of pain is distinct from the unpleasantness associated with it. For example, it is possible in some cases, through psychosurgery or drug treatment, to remove the unpleasantness from pain without affecting its intensity,[1] and cognitive processes such as placebo and hypnotic suggestion can temporarily reduce pain's unpleasantness but leave its intensity unchanged. Some drug therapies and other interventions can remove both the sensation of pain and its unpleasantness, and certain emotional states, such as the excitement of sport or war, can produce the same effect.[2]
Pain makes complex thought more difficult: it impairs attention control, working memory, mental flexibility, problem solving, and information processing speed,[3] and it is associated with increased depression, anxiety, fear, and anger.[4] Cancer pain is classed as acute (usually caused by medical investigation or treatment) or chronic.[5] About 75% of patients with chronic cancer pain have pain caused by the cancer itself. In most of the remainder, pain is the result of treatment.[6]
Infection
Infection of a tumor or its surrounding tissue can cause rapidly escalating pain, but is sometimes overlooked as a possible cause of pain. One study[7] found infection was the cause of pain in four percent of nearly 300 cancer patients referred for pain relief. Another report [8] described seven patients with large ulcerated and necrotic tumors of the head and neck, with erythema, swelling, and hardening or thickening of the surrounding tissue, whose previously well-controlled pain escalated significantly over several days. Antibiotic treatment produced pain relief in all patients within three days.[9]
Nervous system
Brain tissue itself contains no nociceptors; brain tumors cause pain by pressing on blood vessels or the membrane that encapsulates the brain, or indirectly by causing edema which may compress pain-sensitive tissue.[10]
Ten percent of patients with disseminated cancer develop meningeal carcinomatosis, where metastatic seedlings develop in the meninges of both brain and spinal cord, with possible invasion of the spinal cord or brain. Melanoma and breast and lung cancer account for 90 percent of such cases. Headache (often severe and possibly associated with nausea, vomiting, photophobia and neck rigidity) and back pain are frequently the first symptoms. Paresthesia, bowel or bladder dysfunction and lower motor neuron weakness are common features.[11]
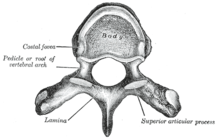
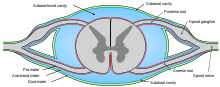
About three percent of cancer patients experience spinal cord compression, usually from expansion of the vertebral body or pedicle (fig. 1) due to metastasis, sometimes involving collapse of the vertebral body. Occasionally compression is caused by nonvertebral metastasis adjacent to the spinal cord. Compression of a spinal nerve root (fig. 3) produces radicular pain, and compression of the long tracts of the cord itself produces funicular pain. Seventy percent of cases involve the thoracic, 20 percent the lumbar, and 10 percent the cervical spine; and about 20 percent of cases involve multiple sites of compression. The nature of the pain depends on the location of the compression.[9]
Between one and five percent of cancer patients suffer peripheral neuropathy due to infiltration or compression of a peripheral nerve by a primary tumor. Small cell lung cancer and, less often, cancer of the breast, colon or ovary may produce inflammation of the dorsal root ganglia (fig. 3), precipitating burning, tingling pain in the extremities, with occasional "lightening" or lancenating pains.[5][9]
Brachial plexopathy is a common product of Pancoast tumor, lymphoma and breast cancer, and can produce severe burning dysesthesic pain on the back of the hand, and cramping, crushing forearm pain.[9]
Bone
Invasion of bone by cancer is the most common source of cancer pain. About 70 percent of breast and prostate cancer patients, and 40 percent of those with lung, kidney and thyroid cancers develop bone metastases. It is commonly felt as tenderness, with constant background pain and instances of spontaneous or movement-related exacerbation, and is frequently described as severe. Tumors in the marrow instigate a vigorous immune response which enhances pain sensitivity, and they release chemicals that stimulate nociceptors. As they grow, tumors compress, infiltrate, cut off blood supply to, or consume body tissues, which can cause nociceptive or neuropathic pain.[9][11]
Rib fractures, common in breast, prostate and other cancers with rib metastases, can cause brief severe pain on twisting the trunk, coughing, laughing, breathing deeply or moving between sitting and lying.
The base of the skull may be affected by metastases from cancer of the bronchus, breast or prostate, or cancer may spread directly to this area from the nasopharynx, and this may cause headache, facial paresthesia, dysesthesia or pain, or cranial nerve dysfunction – the exact symptoms depending on the cranial nerves impacted.[9]
Pelvis
Pain produced by cancer within the pelvis varies according to the cause, but it frequently radiates diffusely to the upper thigh, and may refer to the lumbar region. Lumbosacral plexopathy is often caused by recurrence of cancer in the presacral space, and may refer to the external genitalia or perineum rather than the legs. Local recurrence of cancer attached to the side of the pelvic wall may cause pain in one of the iliac fossae. Pain on walking that confines the patient to bed indicates possible cancer adherence to or invasion of the iliacus muscle. Pain in the hypogastrium (between the navel and pubic bone) is often found in cancers of the uterus and bladder, and sometimes in colorectal cancer especially if infiltrating or attached to either uterus or bladder.[9]
Visceral
Visceral pain is diffuse and difficult to locate, and is often referred to more distant, usually superficial, sites.[11]
A tumor can expand the size of the liver several times, and consequent stretching of its capsule can cause aching pain in the right hypochondrium. Other causes of pain in enlarged liver are traction of the supporting ligaments when standing or walking, internal bleeding of the liver, the liver pressing against the rib cage or pinching the wall of the abdomen, and straining the lumbar spine. In some postures the liver may pinch the parietal peritoneum against the lower rib cage, producing sharp, transitory pain, relieved by changing position. The tumor may also infiltrate the liver's capsule, causing dull, and sometimes stabbing pain.[9]
Cancer of the kidneys and spleen produces less pain than that caused by liver tumor – kidney tumors eliciting pain only once the organ has been almost totally destroyed and the cancer has invaded the surrounding tissue or adjacent pelvis. Pressure on the kidney or ureter from a tumor outside the kidney can cause extreme flank pain.[10] Local recurrence of cancer after the removal of a kidney can cause pain in the lumbar back, or L1 or L2 spinal nerve pain in the groin or upper thigh, accompanied by weakness and numbness of the iliopsoas muscle, exacerbated by activity.[9]
The pain of intestinal tumors may be the result of disturbed motility, dilation, altered blood flow or ulceration. Malignant lymphomas of the gastrointestinal tract can produce large tumors with significant ulceration and bleeding. Inflammation of artery walls and tissue adjacent to nerves is common in tumors of abdominal and urogenital hollow organs.[12]
Cancer in the bronchial tree is usually painless,[12] but ear and facial pain on one side of the head has been reported in some patients. This is referred via the auricular branch of the vagus nerve.[9]
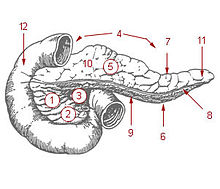 Fig. 2 The pancreas. 1. pancreatic head. 4. pancreatic body. 11. pancreatic tail.
Fig. 2 The pancreas. 1. pancreatic head. 4. pancreatic body. 11. pancreatic tail.
Ten percent of patients with cancer of the pancreatic body or tail experience pain, whereas 90 percent of those with cancer of the pancreatic head will, especially if the tumor is near the hepatopancreatic ampulla. The pain appears on the left or right upper abdomen, is constant, and increases in intensity over time. It is in some cases relieved by leaning forward and heightened by lying on the stomach. Back pain may be present and, if intense, may spread left and right. Back pain may be referred from the pancreas, or may indicate the cancer has penetrated paraspinal muscle, or entered the retroperitoneum and paraaortic lymph nodes [9]
Pain of the rectum may be experienced even after the rectum has been surgically removed. Local recurrence of rectal cancer may cause mild (described as "pressure") or strong pain on sitting; or pain on standing or walking (described as "dragging"). The latter may indicate a deeper recurrence involving attachment to muscle or fascia. A local tumor in the rectum or recurrence involving the presacral plexus may cause pain normally associated with an urgent need to defecate. This pain may, rarely, be phantom after surgical removal of the rectum. Distressing, intense, stabbing, "red hot poker" pain is sometimes reported. Pain within a few weeks of surgical removal of the rectum is usually neuropathic due to the surgery, and described in one study[13] as spontaneous, intermittent, mild to moderate shooting and bursting, or tight and aching. Pain emerging after three months usually signals recurrence, and was described as deep, sharp, aching, intense, and continuous, made worse by sitting or pressure. In over half of patients with late-onset pain in the above study, pain was ameliorated by analgesics.[9]
Infection or cancer may irritate the trigone of the urinary bladder, causing spasm of the detrusor urinae muscle (the muscle that squeezes urine from the urinary bladder), resulting in deep pain above the pubic bone, possibly referred to the tip of the penis, lasting from a few minutes to half an hour.[9]
Serous mucosa
Carcinosis of the peritoneum may cause pain through pressure of the metastases on peripheral nerves, inflammation, or disordered visceral motility. Once a tumor has penetrated or perforated hollow viscera, acute inflammation of the peritoneum appears, inducing severe abdominal pain. Pleural carcinomatosis is normally painless.[12]
Soft tissue
Invasion of soft tissue by a tumor can cause pain by inflammatory or mechanical stimulation of nociceptors, or destruction of mobile structures such as ligaments, tendons and skeletal muscles.[12]
Potentially painful interventions in cancer treatment include immunotherapy which may produce joint or muscle pain; radiotherapy, which can cause skin reactions, enteritis, radiation fibrosis, myelopathy, osteoradionecrosis, neuropathy or plexopathy; chemotherapy, often associated with mucositis, joint pain, muscle pain, peripheral neuropathy and abdominal pain due to diarrhea or constipation; hormone therapy, which sometimes causes pain flares; targeted therapies, such as trastuzumab and rituximab, which can cause muscle, joint or chest pain; angiogenesis inhibitors like bevacizumab, known to sometimes cause bone pain; surgery, which may produce postoperative pain, post-amputation pain or pelvic floor myalgia; and invasive investigations such as lumbar puncture, bone marrow biopsy, venipuncture, paracentesis, and thoracentesis.[14]
Chemotherapy
Chemotherapy may cause mucositis, muscle pain, joint pain, abdominal pain caused by diarrhea or constipation, and peripheral neuropathy (pain and numbness in the hands, wrists, feet and ankles).[14]
Chemotherapy-induced peripheral neuropathy
Some of the more common chemotherapy drugs, including vincristine/vinblastine, aclitaxel/docetaxel, cisplatin/oxaliplatin/carboplatin, thalidomide, and bortezomib, can cause chemotherapy-induced peripheral neuropathy (CIPN), experienced as tingling numbness, intense pain, and hypersensitivity to cold in a glove and sock pattern.[14][15] CIPN often follows the first chemotherapy dose and increases in severity as treatment continues, but this progressive degeneration usually halts at completion of treatment. The platinum-based drugs such as oxaliplatin and cisplatin are the exception; with these drugs, sensation may continue to deteriorate for several months after the end of treatment.[16] Some CIPN appears to be irreversible.[16]
Pain can often be helped with drug treatment but the numbness is usually resistant to treatment.[15]
CIPN disrupts leisure, work and family relations, and the pain of CIPN is often accompanied by sleep and mood disturbance, fatigue and functional difficulties. A 2007 American study found that most patients did not recall being told to expect CIPN, and doctors monitoring the condition rarely asked how it affects daily living but focused on practical effects such as dexterity and gait.[17]
It is not known what causes the condition, but microtubule and mitochondrial damage, and leaky blood vessels near nerve cells are some of the possibilities being explored. It is unknown what percentage of patients are affected.[16]
As possible preventative interventions, the American National Cancer Institute Symptom Management and Health-related Quality of Life Steering Committee recommends continued investigation of glutathione, and intravenous calcium and magnesium, which have shown early promise in limited human trials; acetyl-L-carnitine, which was effective in animal models and on diabetes and HIV patients; and the anti-oxidant alpha-lipoic acid.[18]
Mucositis
Cancer drugs can cause changes in the biochemistry of mucous membranes resulting in intense pain in the mouth, throat, nasal passages, and gastrointestinal tract, making talking, drinking, or eating difficult or impossible.[19]
Muscle and joint pain
Withdrawal of steroid medication can cause joint pain and diffuse muscle pain accompanied by fatigue; these symptoms resolve with recommencement of steroid therapy. Chronic steroid therapy can result in aseptic necrosis of the humoral or femoral head, resulting in shoulder or knee pain described as dull and aching, and reduced movement in or inability to use arm or hip. Aromatase inhibitors can cause diffuse muscle and joint pain and stiffness, and may increase the likelihood of osteoporosis and consequent fractures.[19]
Radiotherapy
Radiotherapy may affect the connective tissue surrounding peripheral nerves, and may damage or kill white or gray matter in the brain or spinal cord.
Fibrosis around the brachial or lumbosacral plexus
Radiotherapy may produce excessive growth (fibrosis) of the fibrous tissue enveloping the brachial or lumbosacral plexus, which can result in damage to the nerves over time (6 months to 20 years). This nerve damage can cause numbness, "pins and needles" or unpleasant sensation and weakness in the affected limb. If pain develops, it is described as diffuse, severe, burning pain, increasing over time, in part or all of the affected limb.[19]
Spinal cord damage
If radiotherapy includes the spinal cord, changes may occur which do not become apparent until some time after treatment. "Early delayed radiation-induced myelopathy" can manifest from six weeks to six months after treatment; the usual symptom is a Lhermitte sign ("a brief, unpleasant sensation of numbness, tingling and often electric-like discharge going from the neck to the spine and extremities, triggered by neck flexion"), and is usually followed by improvement two to nine months after onset, though in some cases symptoms persist for a long time. "Late delayed radiation-induced myelopathy" may occur six months to ten years after treatment. The typical presentation is Brown-Séquard syndrome (a motor deficit and numbness to touch and vibration on one side of the body and loss of pain and temperature sensation on the other). Onset may be sudden but is usually progressive. Some patients improve and others deteriorate.[20]
Management
Main articles: Pain management and Palliative careCancer pain treatment is directed toward relieving pain with minimal adverse treatment effects, allowing the patient a good quality of life and level of function and a relatively painless death.[21] Though 80–90% of cancer pain can be eliminated or well controlled, nearly half of all patients throughout the world with cancer pain receive less than optimal care.[22]
Barriers to pain management
Patients may not report pain due to a belief that pain is inevitable, fear of side effects of treatment, fear of developing addiction or tolerance to opioids, fear of distracting the doctor from treating the illness,[17] or fear of masking a symptom important for monitoring progress of the disease. Patients may be reluctant to take adequate pain medicine because they are unaware of the prognosis or unwilling to accept the diagnosis.[23] Patient failure to report pain or misguided reluctance to take pain medicine can be overcome by sensitive coaching.[17][21]
Despite the publication and ready availability of simple and effective evidence-based pain management guidelines by the World Health Organization (WHO)[24] and others,[25] doctors and nurses frequently lack understanding of key aspects of pain management including assessment, dosing, tolerance and addiction, and many do not know that pain elimination is possible in most cases, that this should be offered wherever possible, and where complete elimination of suffering is not achievable due to intolerable drug side effects, the maximum tolerable dose should be offered.[17][21]
Systemic problems in the delivery of pain management include failure in the clinical setting to refer patients for pain management, inadequate reimbursement for pain management, lack of stocks of pain medicines in poorer areas, out-dated government policy on cancer pain management, and legal restraints on prescription of opioid medication.[17][21]
Cancer is a dynamic process, and pain interventions need to reflect this. Several different treatment modalities may be required over time, as the disease progresses. Pain managers should clearly explain to the patient the cause of the pain and the various treatment possibilities, and should consider, as well as drug therapy, directly modifying the underlying disease, raising the pain threshold, interrupting, destroying or stimulating pain pathways, and suggesting lifestyle modification.[21] The relief of psychological, social and spiritual distress is a key element in effective pain management.[24]
Drugs
The WHO guidelines[24] recommend prompt oral administration of drugs when pain occurs, starting, if the patient is not in severe pain, with non-opioid drugs such as paracetamol, dipyrone, non-steroidal anti-inflammatory drugs or COX-2 inhibitors. Then, if complete pain relief is not achieved or disease progression necessitates more aggressive treatment, mild opioids such as codeine phosphate, dextropropoxyphene, dihydrocodeine or tramadol are added to the existing non-opioid regime. If this is or becomes insufficient, mild opioids are replaced by stronger opioids such as morphine, while continuing the non-opioid therapy, escalating opioid dose until the patient is pain-free or the maximum possible relief without intolerable side effects has been achieved. If the initial presentation is severe cancer pain, this stepping process should be skipped and a strong opioid should be started immediately in combination with a non-opioid analgesic.[21]
The usefulness of the second step is being debated in the clinical and research communities. Some are challenging the pharmacological validity of the step and, pointing to the higher toxicity and low efficacy of mild opioids, argue that they, with the possible exception of tramadol due to its unique action, could be replaced by smaller doses of strong opioids.[21]
Strong opioids should be commenced with concurrent antiemetic and laxative treatment, to counteract the usual nausea and constipation. Nausea normally resolves after two or three weeks of treatment but laxatives will need to be aggressively maintained. More than half of patients with advanced cancer and pain will need strong opioids, and these in combination with non-opioids can produce acceptable analgesia in 70–90 percent of cases. Sedation and cognitive impairment usually occur with the initial dose or a significant increase in dosage of a strong opioid, but improve after a week of consistent dosage.[21]
Analgesics should not be taken "on demand" but "by the clock" (every 3–6 hours), with each dose delivered before the preceding dose has worn off, in doses sufficiently high to ensure continuous pain relief. Patients taking slow-release morphine should also be provided with immediate-release ("rescue") morphine to use as necessary, for pain spikes that are not suppressed by their regular medication.[21]
Oral analgesia is the cheapest, simplest and most acceptable mode of delivery. Other delivery routes such as sublingual, topical, parenteral, rectal or spinal should be considered if the need is urgent, or in case of vomiting, impaired swallow, obstruction of the gastrointestinal tract, poor absorption or coma. Liver and kidney disease can affect the biological activity of analgesics. When such patients are treated with oral opioids they must be monitored for the possible need to reduce dose, extend dosing intervals, or switch to other opioids or other modes of delivery.[21]
Not all pain yields completely to classic analgesics, and drugs that are not traditionally considered analgesics but which effect pain relief in certain cases, such as steroids or bisphosphonates, may be employed concurrently with analgesics at any stage. Tricyclic antidepressants, class I antiarrhythmics, or anticonvulsants are the drugs of choice for neuropathic pain. Up to 90 percent of patients at death are using such "adjuvants". Many adjuvants carry a significant risk of serious complications.[21]
Anxiety reduction can reduce the unpleasantness of pain but is least effective for moderate or severe pain.[26] Since anxiolytics such as benzodiazepines, psychotropic drugs and major tranquilizers add to sedation, they should only be used to address anxiety, depression, disturbed sleep or muscle spasm.[21]
Interventional
If the analgesic and adjuvant regimen recommended above does not adequately relieve pain, additional modes of intervention are available.[27]
Radiation
Radiotherapy is used when drug treatment is failing to control the pain of a growing tumor, such as in bone metastisis (most commonly), penetration of soft tissue or compression of sensory nerves. Often, low doses are adequate to produce analgesia, thought to be due to reduction in pressure or, possibly, interference with the tumor's production of pain-causing chemicals.[28] Radiopharmaceuticals that target specific tumors have been used to treat the pain of metastatic illnesses. Relief may occur within a week of treatment and may last from two to four months.[27]
Nerve blocks
Neurolysis is the injury of a nerve. Chemicals, laser, freezing or heating may be used to injure a sensory nerve and so produce degeneration of the nerve's fibers and the fibers' myelin sheaths, and temporary interference with the transmission of pain signals. In this procedure, the protective casing around the myelin sheath, the basal lamina, is preserved so that, when each damaged fiber regrows, it travels within its basal lamina and connects with the correct loose end, and function may be restored. Surgical cutting of a nerve severs the basal laminae, and without these tubes to channel the regrowing fibers to their lost connections, a neuromata may develop, causing deafferentation pain. This is why neurolysis is preferred over surgically blocking peripheral nerves.[29] A brief "rehearsal" block using local anesthesia should be tried before the actual neurolytic block, to determine efficacy and detect any possible side effects."[27] The aim of this treatment is pain elimination, or the reduction of pain to the point where opioids may be effective.[27] Though neurolysis lacks long-term outcome studies and evidence-based guidelines for its use, for patients with progressive cancer and otherwise incurable pain, it can play an essential role.[29]
Targets for neurolytic block include the celiac plexus, most commonly for cancer of the gastrointestinal tract up to the transverse colon, and pancreatic cancer, but also for stomach cancer, gall bladder cancer, adrenal mass, common bile duct cancer, chronic pancreatitis and active intermittent porphyria; the splanchnic nerve, for retroperitoneal pain, and similar conditions to those addressed by the celiac plexus block but, because of its higher rate of complications, used only if the celiac plexus block is not producing adequate relief; hypogastric plexus, "for cancer affecting the descending colon, sigmoid colon and rectum," as well as cancers of the bladder, prostatic urethra, prostate, seminal vesicles, testicles, uterus, ovary and vaginal fundus; ganglion impar, for the perinium, vulva, anus, distal rectum, distal urethra, and distal third of the vagina; the stellate ganglion, usually for head and neck cancer, or sympathetically mediated arm and hand pain; the intercostal nerves, which serve the skin of the chest and abdomen; and a posterior root ganglion may be injured by targeting the root inside the subarachnoid cavity (fig.3), most effective for pain in the chest or abdominal wall, but also used for other areas including arm/hand or leg/foot pain.[27]
Intrathecal programmable pump
Delivery of an opioid such as morphine, hydromorphone, fentanyl, sufentanyl and meperidine directly into the subarachnoid cavity (fig. 3) provides enhanced analgesia with reduced systemic side effects, and has reduced the level of pain in otherwise intractable cases. The anxiolytic clonidine, or the nonopioid analgesic ziconotide, and local anesthetics such as bupivacaine, ropivacaine or tetracaine may also be infused along with the opioid.[27][30]
Long-term epidural catheter
The outer layer of the sheath surrounding the spinal cord is called the dura mater. Between this and the surrounding vertebrae is the epidural space, filled with connective tissue, fat and blood vessels, and crossed by the spinal nerve roots. A catheter may be inserted into this space for three to six months, to deliver anesthetics or analgesics. The line carrying the drug may be threaded under the skin to emerge at the front of the patient, a process called tunneling. This is recommended with long term use so as to reduce the chance of any infection at the exit site reaching the epidural space.[27]
 Fig. 4. Cross-section of the spinal cord showing the dorsal column and the anterolateral spinothalamic tracts
Fig. 4. Cross-section of the spinal cord showing the dorsal column and the anterolateral spinothalamic tracts
Spinal cord stimulation
Electrical stimulation of the dorsal columns of the spinal cord (fig. 4) can produce analgesia. First, the leads are implanted, guided by the patient's report and fluoroscopy, and the generator is worn externally for several days to assess efficacy. If pain is reduced by more than half, the therapy is deemed to be suitable. A small pocket is cut into the tissue beneath the skin of the upper buttocks, chest wall or abdomen and the leads are threaded under the skin from the stimulation site to the pocket, where they are attached to the snugly-fitting generator.[30] It seems to be more helpful with neuropathic and ischemic pain than nociceptive pain, and is not often used in the treatment of cancer pain.[31]
Deep brain stimulation
Electrical stimulation of structures deep within the brain – the periaqueductal gray and periventricular gray for nociceptive pain, and the internal capsule, ventral posterolateral nucleus and ventral posteromedial nucleus for neuropathic pain – has produced impressive results with some patients but results vary and appropriate patient selection is important. One study[32] of seventeen patients with intractable cancer pain found that thirteen were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life.[31]
Hypophysectomy
Hypophysectomy is the destruction of the pituitary gland, and has been used successfully on metastatic breast and prostate cancer pain.[30]
Cutting or destruction of nervous tissue
Surgical cutting or destruction of peripheral or central nervous tissue is now rarely used in the treatment of pain.[27] Procedures include neurectomy, cordotomy, dorsal root entry zone lesioning, and cingulotomy.
Neurectomy involves cutting a peripheral nerve, and is (rarely) used in patients with short life expectancy who are unsuitable for drug therapy due to ineffectiveness or intolerance. The dorsal (sensory) root or dorsal root ganglion may be usefully targeted (called rhizotomy); with the dorsal root ganglion possibly the more effective target because some sensory fibers enter the spinal cord from the dorsal root ganglion via the ventral (motor) root, and these would not be interrupted by dorsal root neurectomy. Because peripheral nerves often carry both sensory and motor fibers, motor impairment is a possible side effect of neurectomy. A common result of this procedure is "deafferentation pain" where, 6–9 months after surgery, the original pain returns at greater intensity. [30]
Cordotomy involves cutting into the spinothalamic tracts, which run up the front/side (anterolateral) quadrant of the spinal cord, carrying heat and pain signals to the brain (fig. 4). Pancoast tumor pain has been effectively treated with dorsal root entry zone (DREZ) lesioning – damaging a region of the spinal cord where peripheral pain signals cross to spinal cord fibers – this is major surgery, carrying the risk of significant neurological side-effects. Cingulotomy involves cutting the fibers that carry signals directly from the cingulate gyrus to the entorhinal cortex in the brain. It reduces the unpleasantness of pain without affecting its intensity, but may have cognitive side-effects.[30]
Ethical considerations
Doctors and nurses have an ethical obligation to ensure that when consent for pain treatment is withheld or given it is, wherever possible, withheld or given by a fully informed patient. Most importantly, patients must be appraised of serious risks and common side effects of pain treatment. What appears to be an obviously acceptable risk or harm to a professional may be unacceptable to the patient. For instance, patients who experience pain on movement may be willing to forgo strong opioids in order to enjoy alertness during pain-free periods, whereas others would choose round-the-clock sedation so as to remain pain-free. Well informed patients can work with their doctors and are more likely to achieve the optimum pain management regimen. The doctor should not insist on treatment if the patient rejects, and must not provide treatment the doctor believes is more harmful or riskier than the possible benefits can justify.[23]
Some, especially exhausted, terminally ill patients, may not wish to be involved in making pain management decisions, and delegate such choices to the professionals. The patient's participation is a right not an obligation, and though reduced patient involvement may result in less than optimal pain management, this choice should be respected.[23]
As professionals become better informed about the interdependent relationship between physical, emotional and social pain, and the demonstrated benefit to physical pain from alleviation of these other forms of suffering, they may be tempted to question the patient and family about personal relationships. Unless the patient has asked for such psychosocial intervention, or at least freely consented to such questioning, this would be an ethically unjustifiable intrusion into the patient's very personal affairs, analogous to providing drugs without the patient's informed consent.[23]
A professional's obligation to alleviate suffering may occasionally come into conflict with the obligation to prolong life. If a terminally ill patient prefers to be free of pain, despite sedation and the risk of shortening life, they should be provided with their desired pain relief, at the cost of sedation and a possibly slightly shorter life. Where a patient is unable to be involved in this decision, the law and the medical profession in the United Kingdom allow the doctor to assume the patient would prefer to be pain-free, and provide adequate analgesia, even if this treatment may slightly hasten death. It is taken that the underlying cause of death in this case is the illness and not the necessary pain management.[23]
A philosophical justification for this approach is the doctrine of double effect, where, to justify an act involving both a good and a bad effect, four conditions are necessary: the act must be good overall or morally neutral, the person acting must intend only the good effect with the bad effect as an unwanted side effect, the bad effect must not be the cause of the good effect, and the good effect must outweigh the bad. Just as an oncologist who intends to treat cancer may foresee but not intend nausea and other effects of chemotherapy, so a doctor treating suffering may foresee but not intend shortening life.[23]
Epidemiology
The actual global prevalence of cancer pain is difficult to assess because systems for measuring patient pain vary widely, methods of determining prevalence differ from study to study, and there is uncertainty in defining cancer pain because it can be directly or indirectly caused by the cancer.[33]
A 2003 review comparing studies of patients at all stages of cancer yielded a mean prevalence of 48%, ranging from 38% to 100%. Studies of patients at all stages with primary cancer in the head and neck, genitourinary system, prostate or esophagus reported a mean pain prevalence of 70%. Evidence for prevalence of pain in newly diagnosed cancer is scarce. One study found pain in 38% of newly diagnosed cases, and another found 35% of new patients had experienced pain in the preceding two weeks, while a third reported that pain was an early symptom in 18%-49% of cases. Comparison of twenty seven studies of the prevalence of pain in advanced cancer found a weighted mean prevalence of 74%, with reported prevalence rates ranging from 53% to 100%. Metastatic cancer is associated with a higher prevalence of pain than nonmetastatic cancer but this may be related to the disease stage.[33] About 33% of cancer survivors report chronic pain after treatment has been completed.[34]
References
- ^ "International Association for the Study of Pain: Definitions" Retrieved 19 August 2011.
- ^ Melzack R & Casey KL. Sensory, motivational and central control determinants of chronic pain: A new conceptual model. In: Kenshalo DR. The skin senses: Proceedings of the first International Symposium on the Skin Senses, held at the Florida State University in Tallahassee, Florida. p. 432.
- ^ Hart RP, Wade JB, Martelli MF. Cognitive impairment in patients with chronic pain: the significance of stress. Curr Pain Headache Rep. 2003;7(2):116–26. doi:10.1007/s11916-003-0021-5. PMID 12628053.
- ^ Bruehl S, Burns JW, Chung OY, Chont M. Pain-related effects of trait anger expression: neural substrates and the role of endogenous opioid mechanisms. Neurosci Biobehav Rev. 2009;33(3):475–91. doi:10.1016/j.neubiorev.2008.12.003. PMID 19146872.
- ^ a b Foley KM. Acute and chronic cancer pain syndromes. In: Doyle D, Hanks G, Cherny N & Calman K. Oxford textbook of palliative medicine. Oxford: OUP; 2004. ISBN 0198510985. p. 298–316.
- ^ Treatment of cancer pain. The Lancet. 2011;377(9784):2236–2247. doi:10.1016/S0140-6736(11)60236-5. PMID 21704873.
- ^ Gonzalez GR, Foley KM & Portenoy RK. American Pain Society meeting, Phoenix Arizona. 1989.
- ^ Bruera E & MacDonald RN. Intractable pain in patients with advanced head and neck tumors: a possible role of local infection. Cancer treatment reports. 1986;70:691–2. PMID 3708626.
- ^ a b c d e f g h i j k l m Twycross R & Bennett M. Cancer pain syndromes. In: Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain. 2nd ed. London: Hodder Arnold; 2008. ISBN 9780340940075. p. 27–37.
- ^ a b Fitzgibbon DR & Loeser JD. Cancer pain: Assessment, diagnosis and management. Philadelphia: 2010. ISBN 1608310892. p. 34.
- ^ a b c Urch CE & Suzuki R. Pathophysiology of somatic, visceral, and neuropathic cancer pain. In: Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain. 2nd ed. London: Hodder Arnold; 2008. ISBN 9780340940075. p. 3–12.
- ^ a b c d Fitzgibbon DR & Loeser JD. Cancer pain: Assessment, diagnosis and management. Philadelphia: 2010. ISBN 1608310892. p. 35.
- ^ Boas RA, Schug SA & Acland RH. Perineal pain after rectal amputation: A 5 year follow up. Pain. 1993;52:62–70. doi:10.1016/0304-3959(93)90115-6. PMID 8446438.
- ^ a b c International Association for the Study of Pain Treatment-Related Pain
- ^ a b Savage L. Chemotherapy-induced pain puzzles scientists. Journal of the National Cancer Institute. 2007;99(14):1070–1071.
- ^ a b c Windebank AJ & Grisold W. Chemotherapy-induced neuropathy. Journal of the Peripheral Nervous System. 2008 Mar;13(1):27–46. PMID 18346229.
- ^ a b c d e Paice JA, Ferrell B. The management of cancer pain. CA – A Cancer Journal for Clinicians. 2011;61(3):157–82. doi:10.3322/caac.20112. PMID 21543825.
- ^ del Pino BM. Chemotherapy-induced Peripheral Neuropathy. NCI Cancer Bulletin. Feb 23, 2010;7(4):6.
- ^ a b c Fitzgibbon DR & Loeser JD. Cancer pain: Assessment, diagnosis and management. Philadelphia: 2010. ISBN 1608310892. p. 39.
- ^ Fitzgibbon DR & Loeser JD. Cancer pain: Assessment, diagnosis and management. Philadelphia: 2010. ISBN 1608310892. p. 102–3.
- ^ a b c d e f g h i j k l Schug SA & Auret K. Clinical pharmacology: Principles of analgesic drug management. In: Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain. 2nd ed. London: Hodder Arnold; 2008. ISBN 9780340940075. p. 104–22.
- ^ Deandrea S, Montanari M, Moja L, Apolone G. Prevalence of undertreatment in cancer pain. A review of published literature. Ann. Oncol.. 2008;19(12):1985–91. doi:10.1093/annonc/mdn419. PMID 18632721.
- ^ a b c d e f Randall F. Ethical issues in cancer pain management. In: Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain. 2nd ed. London: Hodder Arnold; 2008. ISBN 9780340940075. p. 93–100.
- ^ a b c WHO guidelines:
- World Health Organization (1996). Cancer pain relief. With a guide to opioid availability (2 ed.). Geneva: WHO. ISBN 9241544821. http://books.google.com/books?id=FhaII7PMHZcC&printsec=frontcover&source=gbs_atb#v=onepage&q&f=false.
- World Health Organization (1998). Cancer pain relief and palliative care in children. Geneva: WHO. ISBN 9789241545129.
- ^ Other clinical guidelines:
- "Consensus statement - Symptom management in cancer: Pain, depression and fatigue". USA National Institutes of Health. 2002. http://consensus.nih.gov/2002/2002CancerPainDepressionFatiguesos022html.htm. Retrieved 2011-08-22.
- "Recommendations: morphine and alternative opioids for cancer pain". European Association for Palliative Care. 2001. http://www.eapcnet.eu/Themes/Clinical/Publicationsdocuments/EAPCRecommendations/tabid/1499/ctl/Details/ArticleID/139/mid/2812/Morphine-and-alternative-opioids-in-cancer-pain-the-EAPC-recommendations.aspx. Retrieved 2011-08-22.
- "Control of pain in adults with cancer". Scottish Intercollegiate Guidelines Network. 2008. http://www.sign.ac.uk/guidelines/fulltext/106/index.html. Retrieved 2011-08-22.
- "Clinical practice guidelines in oncology: adult cancer pain (free membership required)" (PDF). USA National Comprehensive Cancer Network. 2011. http://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Retrieved 2011-08-22.
- ^ Price DD, Riley JL & Wade JB. Psychophysical approaches to measurement of the dimensions and stages of pain. In: Turk DC & Melzack R. Handbook of pain assessment. Guildford Press; 2001. ISBN 157230488X. p. 65.
- ^ a b c d e f g h Atallah JN. Management of cancer pain. In: Vadivelu N, Urman RD, Hines RL. Essentials of pain management. New York: Springer; 2011. doi:10.1007/978-0-387-87579-8. ISBN 9780387875781. p. 597–628.
- ^ Hoskin PJ. Radiotherapy. In: Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain. 2nd ed. London: Hodder Arnold; 2008. ISBN 9780340940075. p. 251–55.
- ^ a b Williams JE. Nerve blocks: Chemical and physical neurolytic agents. In: Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain. 2nd ed. London: Hodder Arnold; 2008. ISBN 9780340940075. p. 225–35.
- ^ a b c d e Cosgrove MA, Towns DK, Fanciullo GJ & Kaye AD. Interventional pain management. In: Vadivelu N, Urman RD, Hines RL. Essentials of pain management. New York: Springer; 2011. doi:10.1007/978-0-387-87579-8. ISBN 9780387875781. p. 237–299.
- ^ a b Johnson MI, Oxberry SG & Robb K. Stimulation-induced analgesia. In: Sykes N, Bennett MI & Yuan C-S. Clinical pain management: Cancer pain. 2nd ed. London: Hodder Arnold; 2008. ISBN 9780340940075. p. 235–250.
- ^ Young RF & Brechner T. Electrical stimulation of the brain for relief of intractable pain due to cancer. Cancer. 1986;57:1266–72. PMID 3484665.
- ^ a b Hearn J, Higginson IJ. Cancer pain epidemiology: A systematic review. In: Bruera E, Portenoy RK. Cancer pain: assessment and management. Cambridge UK: Cambridge University Press; 2003. ISBN 0-521-773326. p. 3.
- ^ van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Annals of oncology. 2007:1437–1449. PMID 17355955.
Wikimedia Foundation. 2010.