- Squamous-cell carcinoma
-
Squamous cell carcinoma, NOS Classification and external resources 
SCC of the skin tends to arise from pre-malignant lesions, actinic keratoses; surface is usually scaly and often ulcerates (as shown here).ICD-10 C44 ICD-9 199 ICD-O: M8070/3 MedlinePlus 000829 eMedicine derm/401 MeSH D002294 Squamous cell carcinoma (SCC or SqCC), occasionally rendered as "squamous-cell carcinoma", is a histologically distinct form of cancer. It arises from the uncontrolled multiplication of malignant cells deriving from epithelium, or showing particular cytological or tissue architectural characteristics of squamous cell differentiation, such as the presence of keratin, tonofilament bundles, and/or desmosomes).
Squamous cell carcinoma is one of the most common cancers in humans and other animals, and usually arises from mutated ectodermal or endodermal cells lining body cavities. Therefore, it can develop in a large number of organs and tissues, including the skin, lips, mouth, esophagus, urinary bladder, prostate, lung, vagina, and cervix, among others.
Despite the common name, squamous cell carcinomas arising in different body sites can show tremendous differences in their presenting signs and symptoms, natural history, prognosis, and response to treatment.
Though the use of these terms has been decreasing in the literature, SqCC is still sometimes referred to as "epidermoid carcinoma" and "squamous cell epithelioma".
Contents
Classification
Cancer can be considered a very large and exceptionally heterogeneous family of malignant diseases, with squamous cell carcinomas comprising one of the largest subsets.[1][2][3]
The International Classification of Diseases for Oncology (ICD-O) system lists a number of morphological subtypes and variants of malignant squamous cell neoplasms, including:[4]
- Papillary carcinoma (Code 8050/3)
- Verrucous squamous cell carcinoma (Code 8051/3)
- Papillary squamous cell carcinoma (Code 8052/3)
- Squamous cell carcinoma (Code 8270/3)
- Large cell keratinizing squamous cell carcinoma (Code 8071/3)
- Large cell keratinizing squamous cell carcinoma (Code 8072/3)
- Small cell keratinizing squamous cell carcinoma (Code 8073/3)
- Spindle cell squamous cell carcinoma (Code 8074/3)
- Adenoid/pseudoglandular squamous cell carcinoma (Code 8075/3)
- Intraepidermal squamous cell carcinoma (Code 8081/3)
- Lymphoepithelial carcinoma (Code 8082/3)
Other variants of squamous cell carcinoma are recognized under other systems, such as:
- Basaloid squamous cell carcinoma[3]
- Clear-cell squamous cell carcinoma[3]
- Keratoacanthoma
- Signet-ring-cell squamous-cell carcinoma
Terminology
All squamous cell carcinoma lesions are thought to begin via the repeated, uncontrolled division of cancer stem cells of epithelial lineage or characteristics. Accumulation of these cancer cells cause a microscopic focus of abnormal cells that are, at least initially, locally confined within the specific tissue in which the progenitor cell resided. This condition is called squamous cell carcinoma in situ, and it is diagnosed when the tumor has not yet penetrated the basement membrane or other delimiting structure to invade adjacent tissues. Once the lesion has grown and progressed to the point where it has breached, penetrated, and infiltrated adjacent structures, it is referred to as "invasive" squamous cell carcinoma. Once a carcinoma becomes invasive, it is able to spread to other organs and cause a metastasis, or "secondary tumor", to form.
Related conditions
- Basal cell carcinoma
- Bowen's disease is a sunlight-induced skin disease, and is considered to be an early form of squamous cell carcinoma.
- Erythroplasia of Queyrat
- Keratoacanthoma is a low-grade malignancy of the skin. It originates in the pilo-sebaceous glands, and is similar in clinical presentation and microscopic analysis to squamous cell carcinoma, except that it contains a central keratin plug. Statistically, it is less likely to become invasive than squamous cell carcinoma.
- Marjolin's ulcer is a type of squamous cell carcinoma that arises from a non-healing ulcer or burn wound.
- Melanoma
Signs and symptoms
Symptoms are highly variable depending on the involved organs.
SCC of the skin begins as a small nodule and as it enlarges the center becomes necrotic and sloughs and the nodule turns into an ulcer.
- The lesion caused by SCC is often asymptomatic
- Ulcer or reddish skin plaque that is slow growing
- Intermittent bleeding from the tumor, especially on the lip
- The clinical appearance is highly variable
- Usually the tumor presents as an ulcerated lesion with hard, raised edges
- The tumor may be in the form of a hard plaque or a papule, often with an opalescent quality, with tiny blood vessels
- The tumor can lie below the level of the surrounding skin, and eventually ulcerates and invades the underlying tissue
- The tumor commonly presents on sun-exposed areas (e.g. back of the hand, scalp, lip, and superior surface of pinna)
- On the lip, the tumor forms a small ulcer, which fails to heal and bleeds intermittently
- Evidence of chronic skin photodamage, such as multiple actinic keratoses (solar keratoses)
- The tumor grows relatively slowly
- Unlike basal cell carcinoma (BCC), squamous cell carcinoma (SCC) has a substantial risk of metastasis
- Risk of metastasis is higher in SCC arising in scars, on the lower lips or mucosa, and occurring in immunosuppressed patients.
About one-third of lingual and mucosal tumors metastasize before diagnosis (these are often related to tobacco and alcohol use)
Causes
Human papilloma virus
Human papilloma virus (HPV) has been associated with SqCC of the oropharynx, lung,[5] fingers,[6] and anogenital region.
By region
Skin
Squamous cell carcinoma is the second-most common cancer of the skin (after basal cell carcinoma but more common than melanoma). It usually occurs in areas exposed to the sun. Sunlight exposure and immunosuppression are risk factors for SqCC of the skin, with chronic sun exposure being the strongest environmental risk factor.[7] The risk of metastasis is low, but is much higher than with basal cell carcinoma. Squamous cell cancers of the lip and ears have high rates of local recurrence and distant metastasis (20–50%).[8] Squamous cell cancers of the skin in individuals on immunotherapy or suffering from lymphoproliferative disorders (i.e. leukemia) tend to be much more aggressive, regardless of their location.[9]
Squamous cell carcinoma are generally treated by surgical excision or Mohs surgery. Non-surgical options for the treatment of cutaneous SqCC include topical chemotherapy, topical immune response modifiers, photodynamic therapy (PDT), radiotherapy, and systemic chemotherapy. The use of topical therapy, such as Imiquimod cream and PDT is generally limited to premalignant (i.e., AKs) and in situ lesions. Radiation therapy is a primary treatment option for patients in whom surgery is not feasible and is an adjuvant therapy for those with metastatic or high-risk cutaneous SqCC. At this time, systemic chemotherapy is used exclusively for patients with metastatic disease.[citation needed]
Head and neck cancer
Ninety percent [10] of cases of head and neck cancer (cancer of the mouth, nasal cavity, nasopharynx, throat and associated structures) are due to squamous cell carcinoma. Symptoms may include a poorly healing mouth ulcer, a hoarse voice or other persistent problems in the area. Treatment is usually with surgery (which may be extensive) and radiotherapy. Risk factors include smoking, alcohol consumption and hematopoietic stem cell transplantation.[11] In addition, recent studies show that about 25% of mouth and 35% of throat cancers are associated with HPV. The 5 year disease free survival rate for HPV positive cancer is significantly higher when appropriately treated with surgery, radiation and chemotherapy as compared to non-HPV positive cancer, substantiated by multiple studies including research conducted by Dr. Maureen Gillison, et al. of Johns Hopkins Sidney Kimmel Cancer Center.
Esophagus
Esophageal cancer may be due to either squamous cell carcinoma (ESCC) or adenocarcinoma (EAC). SCCs tend to occur closer to the mouth, while adenocarcinomas occur closer to the stomach. Dysphagia (difficulty swallowing, solids worse than liquids) and odynophagia are common initial symptoms. If the disease is localized, esophagectomy may offer the possibility of a cure. If the disease has spread, chemotherapy and radiotherapy are commonly used.
Lung
Main article: Squamous cell lung carcinomaWhen associated with the lung, it often causes ectopic production of parathyroid hormone-related protein (PTHrP), resulting in hypercalcemia.
Penis
When squamous cell carcinoma in situ (Bowen's disease) is found on the penis, it is called erythroplasia of Queyrat.[12] This type of cancer responds very well to imiquimod[citation needed].
Prostate
When associated with the prostate, squamous cell carcinoma is very aggressive in nature. It is difficult to detect as there is no increase in prostate specific antigen levels seen; meaning that the cancer is often diagnosed at an advanced stage.
Vagina and cervix
Vaginal squamous cell carcinoma spreads slowly and usually stays near the vagina, but may spread to the lungs and liver. This is the most common type of vaginal cancer.
Bladder
Most bladder cancer is transitional cell, but bladder cancer associated with Schistosomiasis is often squamous cell carcinoma.
Diagnosis
Diagnosis is via a biopsy. For the skin, look under skin biopsy.
The pathological appearance of a squamous cell cancer varies with the depth of the biopsy. For that reason, a biopsy including the subcutaneous tissue and basalar epithelium, to the surface is necessary for correct diagnosis. The performance of a shave biopsy (see skin biopsy) might not acquire enough information for a diagnosis. An inadequate biopsy might be read as actinic keratosis with follicular involvement. A deeper biopsy down to the dermis or subcutaneous tissue might reveal the true cancer. An excision biopsy is ideal, but not practical in most cases. An incisional or punch biopsy is preferred. A shave biopsy is least ideal, especially if only the superficial portion is acquired.
Prevention
Appropriate clothing, avoidance of intense sun exposure and sunscreen may prevent skin cancer.[13]
Management
Most squamous cell carcinomas are removed with surgery. A few selected cases are treated with topical medication. Surgical excision with a free margin of healthy tissue is a frequent treatment modality. Radiotherapy, given as external beam radiotherapy or as brachytherapy (internal radiotherapy), can also be used to treat squamous cell carcinomas.
Mohs surgery is frequently utilized; considered the treatment of choice for squamous cell carcinoma of the skin, physicians have also utilized the method for the treatment of squamous cell carcinoma of the mouth, throat, and neck.[14] An equivalent method of the CCPDMA standards can be utilized by a pathologist in the absence of a Mohs-trained physician. Radiation therapy often used afterward in high risk cancer or patient types.
Electrodesiccation and curettage or EDC can be done on selected squamous cell carcinoma of the skin. In areas where SCC's are known to be non-aggressive, and where the patient is not immunosuppressed, EDC can be performed with good to adequate cure rate.
Imiquimod (Aldara) has been used with success for squamous cell carcinoma in situ of the skin and the penis, but the morbidity and discomfort of the treatment is severe. An advantage is the cosmetic result: after treatment, the skin resembles normal skin without the usual scarring and morbidity associated with standard excision. Imiquimod is not FDA-approved for any squamous cell carcinoma.
In 2007, Australian biopharmaceutical company Clinuvel Pharmaceuticals Limited began clinical trials with an experimental treatment, a melanocyte-stimulating hormone called afamelanotide (formerly CUV1647)[15] to provide photoprotection for organ transplant patients against squamous cell carcinoma of the skin and actinic keratosis.[16][17]
Epidemiology
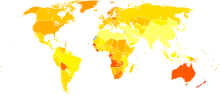 Age-standardized death from melanoma and other skin cancers per 100,000 inhabitants in 2004.[18]
Age-standardized death from melanoma and other skin cancers per 100,000 inhabitants in 2004.[18] no dataless than 0.70.7–1.41.4–2.12.1–2.82.8–3.53.5–4.24.2–4.94.9–5.65.6–6.36.3–77–7.7more than 7.7
no dataless than 0.70.7–1.41.4–2.12.1–2.82.8–3.53.5–4.24.2–4.94.9–5.65.6–6.36.3–77–7.7more than 7.7Incidence of squamous cell carcinoma varies with age, gender, race, geography, and genetics. The incidence of SCC increases with age and the peak incidence is usually around 66 years old. Males are affected with SCC at a ratio of 2:1 in comparison to females. Caucasians are more likely to be affected, especially those with fair Celtic skin, if chronically exposed to UV radiation. There are also a few rare congenital diseases predisposed to cutaneous malignancy. In certain geographic locations, exposure to arsenic in well water or from industrial sources may significantly increase the risk of SCC.[7]
References
- ^ Berman JJ (November 2004). "Tumor taxonomy for the developmental lineage classification of neoplasms". BMC Cancer 4: 88. doi:10.1186/1471-2407-4-88. PMC 535937. PMID 15571625. http://www.biomedcentral.com/1471-2407/4/88.
- ^ Berman JJ (March 2004). "Tumor classification: molecular analysis meets Aristotle". BMC Cancer 4: 10. doi:10.1186/1471-2407-4-10. PMC 415552. PMID 15113444. http://www.biomedcentral.com/1471-2407/4/10.
- ^ a b c Travis, William D; Brambilla, Elisabeth; Muller-Hermelink, H Konrad et al., eds (2004). Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. World Health Organization Classification of Tumours. Lyon: IARC Press. ISBN 92 832 2418 3. http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb10/bb10-cover.pdf. Retrieved 27 March 2010.
- ^ World Health Organization. International Classification of Diseases for Oncology, Second Edition. Geneva, Switzerland: World Health Organization, 1990.
- ^ Yu Y, Yang A, Hu S, Yan H (June 2009). "Correlation of HPV-16/18 infection of human papillomavirus with lung squamous cell carcinomas in Western China". Oncol. Rep. 21 (6): 1627–32. PMID 19424646. http://www.spandidos-publications.com/or/21/6/1627.
- ^ "Recurrent Squamous Cell Carcinoma In Situ of the Finger". http://www.medscape.com/viewarticle/458357. Retrieved 2010-09-22.
- ^ a b Cutaneous squamous cell carcinoma
- ^ http://www.aad.org/public/publications/pamphlets/sun_squamous.html
- ^ http://www.skincarephysicians.com/skincancernet/squamous_cell_carcinoma.html
- ^ http://www.macmillan.org.uk/Cancerinformation/Cancertypes/Headneck/Aboutheadneckcancers/Typesofheadneckcancer.aspx
- ^ Elad S, Zadik Y, Zeevi I, et al. (December 2010). "Oral cancer in patients after hematopoietic stem-cell transplantation: long-term follow-up suggests an increased risk for recurrence". Transplantation 90 (11): 1243–4. doi:10.1097/TP.0b013e3181f9caaa. PMID 21119507.
- ^ Erythroplasia of rat (Bowen Disease of the Glans Penis) at eMedicine
- ^ Gallagher, RP; Lee, TK, Bajdik, CD, Borugian, M (2010). "Ultraviolet radiation.". Chronic diseases in Canada 29 (Suppl 1): 51–68. PMID 21199599.
- ^ Gross, K.G., et al. (1999). Mohs Surgery, Fundamentals and Techniques. Mosby.
- ^ "World Health Organisation assigns CUV1647 generic name" (PDF). Clinuvel. 2008. http://www.clinuvel.com/resources/pdf/asx_announcements/2008/20080617WHOGenericName.pdf. Retrieved 2008-06-17.
- ^ Clinuvel » Investors » FAQs
- ^ PharmaAsia - Clinuvel’s Drug Begins Global Phase II Skin Cancer Trials
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html. Retrieved Nov. 11, 2009.
External links
- Information on Squamous Cell Carcinoma from The Skin Cancer Foundation
- DermNet NZ: Squamous cell carcinoma
- Squamous cell carcinoma in transplant recipients
- Including TCC, CIS and papillary tumour SCC
- Cancer Management Handbook: Head and Neck Tumors
Glandular and epithelial neoplasms (ICD-O 8010-8589) Epithelium Small cell carcinoma · Combined small cell carcinoma · Verrucous carcinoma · Squamous cell carcinoma · Basal cell carcinoma · Transitional cell carcinoma · Inverted papillomaGlands Other/multipleAdnexal and
skin appendage (8390-8429)Cystic, mucinous,
and serous (8440-8499)Cystic generalSerousOvarian serous cystadenoma/Pancreatic serous cystadenoma/Serous cystadenocarcinoma/Papillary serous cystadenocarcinomaDuctal, lobular,
and medullary (8500-8549)Lobular carcinoma in situ · Invasive lobular carcinomaAcinar cell (8550-8559)Other Complex epithelial (8560-8589)see also Template:Epithelium and epithelial tissueTumors: Skin neoplasm, Epidermis (C44.L12–L38/D23.L53-83, 173/216) Tumor Micronodular basal cell carcinoma · Superficial basal cell carcinoma · Nodular basal cell carcinoma (Rodent ulcer) · Cystic basal cell carcinoma · Cicatricial basal cell carcinoma · Pigmented basal cell carcinoma · Aberrant basal cell carcinoma · Infiltrative basal cell carcinoma · Nevoid basal cell carcinoma syndrome · Polypoid basal cell carcinoma · Pore-like basal cell carcinoma · Fibroepithelioma of PinkusSCCAcanthoma (Large cell acanthoma) · Adenoid squamous cell carcinoma · Basaloid squamous cell carcinoma · Clear cell squamous cell carcinoma · Signet-ring cell squamous cell carcinoma · Spindle cell squamous cell carcinoma · Bowen's disease
Marjolin's ulcer · Erythroplasia of QueyratOther/ungroupedMerkel cell carcinoma · Microcystic adnexal carcinoma · Mucinous carcinoma · Primary cutaneous adenoid cystic carcinoma · Verrucous carcinomaOtherAcanthoma: Acanthoma fissuratum · Clear cell acanthoma · Epidermolytic acanthoma · Melanoacanthoma · Pilar sheath acanthoma · Seboacanthoma
Keratoacanthoma: Generalized eruptive keratoacanthoma · Keratoacanthoma centrifugum marginatum · Multiple keratoacanthomas · Solitary keratoacanthoma
Adenocarcinoma: Aggressive digital papillary adenocarcinoma · Extramammary Paget's disease
Mixed tumor (Malignant mixed tumor)Ungrouped epidermal nevus: Epidermal nevus syndrome · Inflammatory linear verrucous epidermal nevus · Linear verrucous epidermal nevus · Pigmented hairy epidermal nevus syndrome · Systematized epidermal nevus · Schimmelpenning syndrome · Nevus comedonicus/Nevus comedonicus syndrome · Phakomatosis pigmentokeratotica
other nevus: Nevus unius lateris · Patch blue nevus · Unilateral palmoplantar verrucous nevus · Zosteriform speckled lentiginous nevus
ungrouped: balanitis (Balanitis plasmacellularis, Pseudoepitheliomatous keratotic and micaceous balanitis) · Cutaneous hornTumors: Mediastinal tumors/Thoracic neoplasm/respiratory neoplasia (C30–C34/D14, 160–163/212.0–212.4) Upper RT Lower RT Tracheal tumorSquamous cell carcinoma · Adenocarcinoma of the lung · Large-cell lung carcinoma · Rhabdoid carcinoma · Sarcomatoid carcinoma · Carcinoid · Salivary gland-like carcinoma of the lung · Adenosquamous carcinoma · Papillary adenocarcinomaNon-carcinomaBy locationPleura Tumors: female urogenital neoplasia (C51–C58/D25–D28, 179–184/218–221) Adnexa Glandular and epithelial/
surface epithelial-
stromal tumorCMS: Ovarian serous cystadenoma · Mucinous cystadenoma · Cystadenocarcinoma (Papillary serous cystadenocarcinoma) · Krukenberg tumorSex cord-gonadal stromalLeydig cell tumour · Sertoli cell tumour · Sertoli-Leydig cell tumour · Thecoma · Granulosa cell tumour · LuteomaDysgerminoma · Nongerminomatous (Embryonal carcinoma, Endodermal sinus tumor, Gonadoblastoma, Teratoma/Struma ovarii, Choriocarcinoma)Uterus Endometrioid tumor · Uterine papillary serous carcinoma · Clear cell carcinoma · Endometrial intraepithelial neoplasiaGeneralVagina SCC · Botryoid rhabdomyosarcoma · Clear cell adenocarcinoma of the vagina · Vaginal intraepithelial neoplasiaVulva Categories:- Anatomical pathology
- Gastrointestinal cancer
- Gynaecological cancer
- Lung cancer
- Epidermal nevi, neoplasms, cysts
- Carcinoma
Wikimedia Foundation. 2010.


