- Mammary ductal carcinoma
-
Ductal Carcinoma Classification and external resources 
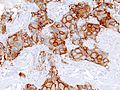
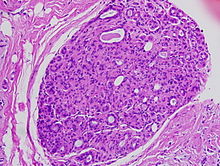
Histopathologic image from ductal cell carcinoma in situ (DCIS) of breast. Hematoxylin-eosin stain.ICD-10 C50, D05 ICD-9 174-175, 233.0 ICD-O: M8500/2-M8500/3 MeSH D018270  Mastectomy specimen containing a very large invasive ductal carcinoma of the breast
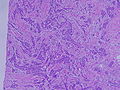
Mastectomy specimen containing a very large invasive ductal carcinoma of the breast
 Typical macroscopic (gross) appearance of the cut surface of a mastectomy specimen containing an invasive ductal carcinoma of the breast (pale area at the center).
Typical macroscopic (gross) appearance of the cut surface of a mastectomy specimen containing an invasive ductal carcinoma of the breast (pale area at the center).
Mammary ductal carcinoma is the most common type of breast cancer in women. It comes in two forms: invasive ductal carcinoma (IDC), an infiltrating, malignant and abnormal proliferation of neoplastic cells in the breast tissue, or ductal carcinoma in situ (DCIS), a noninvasive, possibly malignant, neoplasm that is still confined to the milk ducts (lactiferous ducts), where breast cancer most often originates. Many doctors feel that DCIS is overdiagnosed and that many women who are treated for DCIS do not actually have cancer.[1]
Contents
Invasive ductal carcinoma
Invasive ductal carcinoma (IDC) is the most common form of invasive breast cancer. It accounts for 55% of breast cancer incidence upon diagnosis, according to statistics from the United States in 2004.[2] On a mammogram, it is usually visualized as a mass with fine spikes radiating from the edges. On physical examination, this lump usually feels much harder or firmer than benign breast lesions such as fibroadenoma. On microscopic examination, the cancerous cells invade and replace the surrounding normal tissues. IDC is divided in several histological subtypes.
Prognosis for IDC
The prognosis of IDC depends, in part, on its histological subtype. Mucinous, papillary, cribriform, and tubular carcinomas have longer survival, and lower recurrence rates. The prognosis of the most common form of IDC, called "IDC Not Otherwise Specified", is intermediate. Finally, some rare forms of breast cancer (e.g. sarcomatoid carcinoma, inflammatory carcinoma) have a poor prognosis.
Regardless of the histological subtype, the prognosis of IDC depends also on tumor size, presence of cancer in the lymph nodes, histological grade, presence of cancer in small vessels (vascular invasion), expression of hormone receptors and of oncogenes like HER2/neu.
These parameters can be entered into models that provide a statistical probability of systemic spread. The probability of systemic spread is a key factor in determining whether radiation and chemotherapy are worthwhile. The individual parameters are important also because they can predict how well a cancer will respond to specific chemotherapy agents.
Overall, the 5-year survival rate of invasive ductal carcinoma was approximately 85% in 2003.[3]
Tumor size
Tumors under 1 cm in diameter are unlikely to spread systemically. Tumors are staged by size.[4]
Diameter Tumor Size Staging Number 0–5 mm T1a 5–10 mm T1b 10–20 mm T1c 20-50mm T2 >50 mm T3 Tumor involves skin or chest wall T4 Lymph node involvement
Absence of cancer cells in the lymph nodes is a good indication that the cancer has not spread systemically. Presence of cancer in the lymph nodes indicates the cancer may have spread. In studies, some women have had presence of cancer in the lymph nodes, were not treated with chemotherapy, and still did not have a systemic spread. Therefore, lymph node involvement is not a positive predictor of spread.[4]
Lymph Node Status Lymph Node Involvement Grade No involved nodes N0 Involved node or nodes N1 Involved nodes that are fixed to one another N2 Clinical staging
Tumor size staging and node involvement staging can be combined into a single clinical staging number.
Tumor Size Staging Node Involvement Staging Clinical Stage T1 N0 I T1 N1 IIA T2 N0 IIA T2 N1 IIB T3 N0 IIB T1-T2 N2 IIIA T3 N1 IIIA T3 N2 IIIA T4 N0-N2 IIIB Histologic appearance
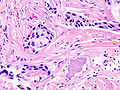
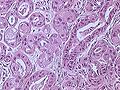
Main article: Bloom-Richardson grading systemThe appearance of cancer cells under a microscope is another predictor of systemic spread. The more different the cancer cells look compared to normal duct cells, the greater the risk of systemic spread. There are three characteristics that differentiate cancer cells from normal cells.
- Tendency to form tubular structures
- Nuclear size, shape, and staining intensity
- Mitotic rate - Rate of cell division
The histologic appearance of cancer cells can be scored on these three parameters on a scale from one to three. The sum of these grades is a number between 3 and 9. The score is called a Bloom Richardson Grade (BR) and is expressed [sum of the grades]/9. For example, cells that were graded 2 on all three parameters would result in a BR score of 6/9.
A score of 5 and under is considered Low. 6 to 7 is considered Intermediate. 8 to 9 is considered High.[4]
Vascular invasion
The presence of cancer cell in small blood vessels is called vascular invasion. The presence of vascular invasion increases the probability of systemic spread.[4]
DNA analysis
DNA analysis indicates the amount of DNA in cancer cells and how fast the cancer is growing.
Cells with the normal amount of DNA are called diploid. Cells with too much or too little DNA are called aneuploid. Aneuploid cells are more likely to spread than diploid cells.
DNA testings indicates the rate of growth by determining the number of cells in the synthetic phase (S Phase). An S Phase > 10% means a higher chance of spreading.
The results of DNA testing are considered less reliable predictors of spread than size, histology, and lymph node involvement.[4]
Treatment options for IDC
Treatment of IDC depends on the size of the mass (size of the tumor measured in its longest direction):
- <4 cm mass: surgery to remove the main tumor mass and to sample the lymph nodes in the axilla. The stage of the tumor is ascertained after this first surgery. Adjuvant therapy (i.e. treatment after surgery) may include a combination of chemotherapy, radiotherapy, hormonal therapy (e.g. tamoxifen) and/or targeted therapy (e.g. trastuzumab). More surgery is occasionally needed to complete the removal of the initial tumor or to remove recurrences.
- 4 cm or larger mass: modified (a less aggressive form of radical mastectomy) radical mastectomy (because any malignant mass in excess of 4 cm in size exceeds the criteria for a lumpectomy) along with sampling of the lymph nodes in the axilla.
The treatment options offered to an individual patient are determined by the form, stage and location of the cancer, and also by the age, history of prior disease and general health of the patient. Not all patients are treated the same way.
Additional images of invasive ductal carcinoma
Ductal carcinoma in situ (intraductal carcinoma)
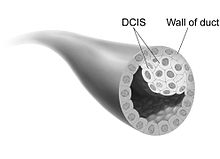
Ductal carcinoma In Situ, DCIS (also known as intraductal carcinoma) is the most common type of noninvasive breast cancer or pre-cancer in women. Ductal carcinoma refers to the development of cancer cells within the milk ducts of the breast. In situ means "in place" and refers to the fact that the cancer has not moved out of the duct and into any surrounding tissue.
DCIS is often referred to as "stage zero breast cancer", and experts disagree on whether it should even be called "cancer" at all. It is known to be a risk factor for invasive ("real") breast cancer, and in a small fraction of cases it is a precancerous condition that may eventually transform into invasive breast cancer.[5] DCIS is not traditionally regarded as being harmful in itself; however, there is evidence of metastases in up to 2% of cases of DCIS.[6] The use of the term carcinoma in the official is misleading and frightening to women diagnosed with DCIS, and at least one expert responsible for its naming now regrets the choice.[5]
DCIS almost never produces symptoms or a lump that can be felt, so it is almost always found through screening mammography.[5] As screening mammography has become more widespread, DCIS has become one of the most commonly diagnosed breast conditions, now accounting for 20% of breast cancers and pre-cancers that are detected through screening mammography.[7] DCIS is usually seen on a mammogram as very small specks of calcium known as microcalcifications. However, not all microcalcifications indicate the presence of DCIS, which must be confirmed by biopsy.
Even without treatment, a majority of women with DCIS will not develop invasive breast cancer from the DCIS.[5] However, surgical excision, aimed at excising all of the abnormal duct elements, is a common treatment, and radiation after surgery further reduces the risk that the DCIS will recur.
Treatment options for DCIS
DCIS patients have two surgery strategy choices: They are lumpectomy (most commonly followed by radiation therapy) or mastectomy. The survival rate is equally high for both treatments, 96 percent or higher.[8]
Women also have the option of rejecting surgery. The survival rate here is unknown, but since a majority of DCIS never transforms into invasive breast cancer,[5] it is not small. Women who reject surgery tend to be older or have other, serious health problems, which further complicates comparisons.
Biomarkers can identify which women who were initially diagnosed with DCIS are at high or low risk of subsequent invasive cancer.[9][10]
Adjunct radiotherapy after lumpectomy offers equivalent survival to mastectomy, although there is a slightly higher risk of recurrence of DCIS or breast cancer. The addition of radiation therapy to lumpectomy reduces the risk of local recurrence to approximately 12 percent, of which approximately half will be DCIS and half will be breast cancer; the risk of recurrence is 1 percent for women undergoing mastectomy.[11] In addition, radiation therapy may reduce recurrence among patients with DCIS getting breast-conserving surgery (lumpectomy) as compared to breast-conserving surgery alone according to a systematic review.[12] Patients who received breast-conserving surgery plus radiation therapy had a lower DCIS recurrence rate than patients who received breast conserving surgery alone. The use of radiation therapy did not have an effect on mortality.
Black women with DCIS have higher risks of local recurrence of DCIS or breast cancer than white women. Extensive DCIS of high grade, large size, and resected with minimal surgical margins, even with radiotherapy, also have a higher risk of recurrence.
Because of the higher risk of recurrence, mastectomy may be the preferred treatment for some women or in certain instances e.g. if:
- DCIS is "multi-focal" (present in two or more areas of the breast).
- The DCIS tumor is relatively large or of high grade.
- Failure to achieve adequate margins on attempted lumpectomy.
- The breast has previously received radiation treatment.
- The patient has had scleroderma or another disease of the connective tissue, which can complicate radiation treatment.
- The patient lives in an area where radiation treatment is inaccessible or inconvenient.
- The patient is under the age of 40.
A system for analysing the suitability of DCIS patients for the options of breast conservation without radiation, breast conservation with radiation, or mastectomy is called the VanNuys Prognostic Scoring Index (VNPI). This VNPI analyzes DCIS features in terms of size, grade, surgical margins, and patient age and assigns "scores" to favourable features.
Tamoxifen or another hormonal therapy is recommended for some women with estrogen-receptor positive DCIS to help prevent breast cancer.[11] Hormonal therapy further decreases the risk of recurrence of DCIS or the development of invasive breast cancer. However, hormone treatment increases the risk of endometrial cancer, severe circulatory problems, or stroke. In addition, hot flashes, vaginal dryness, abnormal vaginal bleeding, and a possibility of premature menopause are common for pre—menopausal women who start treatment.
Unlike women with invasive breast cancer, women with DCIS do not undergo chemotherapy and have traditionally not been advised to have their lymph nodes tested or removed. Some institutional series reporting significant rates of recurrent invasive cancers after mastectomy for DCIS have recently endorsed routine sentinel node biopsy (SNB) in these patients,[13] while others have concluded it be reserved for selected patients. Most agree that SNB should be considered with tissue diagnosis of high risk DCIS (grade III with palpable mass or larger size on imaging) as well as in patients undergoing mastectomy after a core or excisional biopsy diagnosis of DCIS.[14][15] Experts are not sure whether all women with DCIS would eventually develop invasive breast cancer if they live long enough without undergoing treatment.
What happens if DCIS is not treated?
According to the NIH Consensus Conference, many DCIS lesions will never become breast cancer, and some will disappear without treatment.[16] If DCIS is allowed to go untreated, the natural course or natural history varies according to the grade of the DCIS.
Unless treated, approximately 60 percent of low-grade DCIS lesions will become invasive at 40 years follow-up—long after many of the diagnosed women have died from other causes.[16] The remaining 40 percent of low-grade DCIS lesions will remain harmless.
High-grade DCIS lesions that have been inadequately resected and not given radiotherapy have a 50 percent risk of becoming invasive breast cancer within seven years. Approximately half of low-grade DCIS detected at screening will represent overdiagnosis, but overdiagnosis of high-grade DCIS is rare.
The natural history of intermediate-grade DCIS is difficult to predict. Approximately one-third of malignant calcification clusters detected at screening mammography already have an invasive focus.
See also
- Breast cancer
- Atypical ductal hyperplasia
- Collagenous spherulosis
References
- ^ Prone to Error: Earliest Steps to Find Cancer By STEPHANIE SAUL, New York Times, July 19, 2010
- ^ Percentage values are from United States statistics 2004. Subtype specific incidences are taken from Table 6 (invasive) and Table 3 (in situ) from Eheman CR, Shaw KM, Ryerson AB, Miller JW, Ajani UA, White MC (June 2009). "The changing incidence of in situ and invasive ductal and lobular breast carcinomas: United States, 1999-2004". Cancer Epidemiol. Biomarkers Prev. 18 (6): 1763–9. doi:10.1158/1055-9965.EPI-08-1082. PMID 19454615.. These are divided by total breast cancer incidence (211,300 invasive and 55,700 in situ cases) as reported from Breast Cancer Facts & Figures 2003-2004 [1]
- ^ NOTE: Number really refers to invasive ductal carcinoma, despite title. Arpino G, Bardou VJ, Clark GM, Elledge RM (2004). "Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome". Breast Cancer Res. 6 (3): R149–56. doi:10.1186/bcr767. PMC 400666. PMID 15084238. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=400666.
- ^ a b c d e Link, John; The Breast Cancer Survival Manual, 4th Edition
- ^ a b c d e Welch HG, Woloshin S, Schwartz LM (February 2008). "The sea of uncertainty surrounding ductal carcinoma in situ--the price of screening mammography". J. Natl. Cancer Inst. 100 (4): 228–9. doi:10.1093/jnci/djn013. PMID 18270336.
- ^ Kelly TA, Kim JA, Patrick R, Grundfest S, Crowe JP (October 2003). "Axillary lymph node metastases in patients with a final diagnosis of ductal carcinoma in situ". American Journal of Surgery 186 (4): 368–70. doi:10.1016/S0002-9610(03)00276-9. PMID 14553852.
- ^ Ernster VL, Ballard-Barbash R, Barlow WE, et al. (October 2002). "Detection of ductal carcinoma in situ in women undergoing screening mammography". Journal of the National Cancer Institute 94 (20): 1546–54. doi:10.1093/jnci/94.20.1546. PMID 12381707.
- ^ Zuckerman, D (December 2009). "DCIS: Mostly Good News". Cancer Prevention and Treatment Fund. http://www.stopcancerfund.org/posts/145.
- ^ Kerlikowske, K.; Molinaro, A. M.; Gauthier, M. L.; Berman, H. K.; Waldman, F.; Bennington, J.; Sanchez, H.; Jimenez, C. et al. (2010). "Biomarker Expression and Risk of Subsequent Tumors After Initial Ductal Carcinoma in Situ Diagnosis". JNCI Journal of the National Cancer Institute 102 (9): 627. doi:10.1093/jnci/djq101. PMC 2864293. PMID 20427430. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2864293.
- ^ Witkiewicz AK, Dasgupta A, Nguyen KH, et al. (June 2009). "Stromal caveolin-1 levels predict early DCIS progression to invasive breast cancer". Cancer Biology & Therapy 8 (11): 1071–1079. doi:10.4161/cbt.8.11.8874. PMID 19502809. http://www.landesbioscience.com/journals/cbt/abstract.php?id=8874.
- ^ a b "NIH DCIS Consensus Conference Statement". National Institutes of Health. September 2009. http://consensus.nih.gov/2009/dcisstatement.htm.
- ^ Virnig, BA; Tuttle, TM; Shamliyan, T; Kane, RL (2010). "Ductal carcinoma in situ of the breast: a systematic review of incidence, treatment, and outcomes". Journal of the National Cancer Institute 102 (3): 170–8. doi:10.1093/jnci/djp482. PMID 20071685.
- ^ Tan JC, McCready DR, Easson AM, Leong WL (February 2007). "Role of sentinel lymph node biopsy in ductal carcinoma-in-situ treated by mastectomy". Annals of Surgical Oncology 14 (2): 638–45. doi:10.1245/s10434-006-9211-9. PMID 17103256.
- ^ van Deurzen CH, Hobbelink MG, van Hillegersberg R, van Diest PJ (April 2007). "Is there an indication for sentinel node biopsy in patients with ductal carcinoma in situ of the breast? A review". European Journal of Cancer 43 (6): 993–1001. doi:10.1016/j.ejca.2007.01.010. PMID 17300928.
- ^ Yen TW, Hunt KK, Ross MI, et al. (April 2005). "Predictors of invasive breast cancer in patients with an initial diagnosis of ductal carcinoma in situ: a guide to selective use of sentinel lymph node biopsy in management of ductal carcinoma in situ". Journal of the American College of Surgeons 200 (4): 516–26. doi:10.1016/j.jamcollsurg.2004.11.012. PMID 15804465.
- ^ a b Evans, A. (2004). Breast Cancer Research 6: P23. doi:10.1186/bcr842. [2]
External links
Glandular and epithelial neoplasms (ICD-O 8010-8589) Epithelium Glands Other/multipleAdnexal and
skin appendage (8390-8429)Cystic, mucinous,
and serous (8440-8499)Cystic generalSerousOvarian serous cystadenoma/Pancreatic serous cystadenoma/Serous cystadenocarcinoma/Papillary serous cystadenocarcinomaDuctal, lobular,
and medullary (8500-8549)Mammary ductal carcinoma · Pancreatic ductal carcinoma · Comedocarcinoma · Paget's disease of the breast/Extramammary Paget's diseaseLobular carcinoma in situ · Invasive lobular carcinomaAcinar cell (8550-8559)Other Complex epithelial (8560-8589)see also Template:Epithelium and epithelial tissue Tumors: breast cancer (C50/D24, 174–175/217) – Histopathologic classification Fibroepithelial/stromal Ductal, lobular, and medullary Intraductal papillomaInvasive lobular carcinoma (ILC)MedullaryOther/ungroupedPrecursor lesions Atypical ductal hyperplasiaOther Related subjects Main article · Classification · Risk factors (Alcohol · Hereditary breast-ovarian cancer syndrome · BRCA mutation) · Screening · Treatment
Categories:
Wikimedia Foundation. 2010.