- Breast cancer screening
-
Breast cancer screening refers to the medical screening of asymptomatic, apparently healthy women for breast cancer in an attempt to achieve an earlier diagnosis. The assumption is that early detection will improve outcomes. A number of screening test have been employed including: clinical and self breast exams, mammography, genetic screening, ultrasound, and magnetic resonance imaging.
A clinical or self breast exam involves feeling the breast for lumps or other abnormalities. Evidence however does not support its use in women with a typical risk for breast cancer.[1] The use of mammography in universal screening for breast cancer is also controversial. The Cochrane collaboration in 2009 concluded that it is unclear whether screening does more good than harm.[2] Many national organizations still recommend it for most older women. If screening mammography (as opposed to diagnostic mammography) is chosen for women at normal risk for breast cancer, it should only be done every two years in women between the ages of 50 and 74.[3] Several tools are available to help target breast cancer screening to older women with longer life expectancies.[4] Similar imaging studies can be performed with magnetic resonance imaging.
Earlier, more aggressive, and more frequent screening is recommended for women at particularly high risk of developing breast cancer, such as those with a confirmed BRCA mutation, those who have previously had breast cancer, and those with a strong family history of breast and ovarian cancer.
Abnormal findings on screening are further investigated by surgically removing a piece of the suspicious lumps (biopsy) to examine them under the microscope. Ultrasound may be used to guide the biopsy needle during the procedure. Magnetic resonance imaging is used to guide treatment, but is not an established screening method for healthy women.
Contents
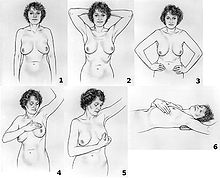
Breast exam
Main article: Breast self-examinationBreast examination (either clinical breast exams (CBE) by a health care provider or by self exams) were once widely recommended. They however are not supported by evidence and may, like mammography and other screening methods that produce false positive results, contribute to harm. The use of screening in women without symptoms and at low risk is thus controversial.[5]
A 2003 Cochrane review found screening by breast self-examination or by clinical exam is not associated with death rates among women who report performing breast self-examination and does, like other breast cancer screening methods, increase harms, in terms of increased numbers of benign lesions identified and an increased number of biopsies performed. They conclude "screening by breast self-examination or physical examination cannot be recommended." [1]
Mammography
Main article: MammographyMammography is a common screening method, since it is relatively fast and widely available in developed countries. Mammography is a type of radiography used on the breasts. Mammography is not useful in finding breast tumors in dense breast tissue characteristic of women under 40 years. It is typically used for two purposes: to aid in the diagnosis of a woman who is experiencing symptoms (called diagnostic mammography), and for medical screening of apparently healthy women (called screening mammography). In women over 50 without dense breasts, breast cancers detected by screening mammography are usually smaller and less aggressive than those detected by patients or doctors as a breast lump. This is because the most aggressive breast cancers are found in dense breast tissue which mammograms can not image.
The presumption is that by detecting the cancer in an earlier stage, women will be more likely to be cured by treatment. This assertion however has been challenged by recent reviews which have found the significance of these benefits to be questionable.
How it works
Screening mammography is usually recommended to women who are most likely to develop breast cancer. In general, this means women with a personal or family history of breast cancer, and most older women, but not frail elderly women, who are unlikely to benefit from treatment.
Women who agree to be screened have their breasts X-rayed on a specialized X-ray machine. This exposes the woman's breasts to a small amount of ionizing radiation, which has a very small, but non-zero, chance of causing cancer.
The X-ray image, called a radiograph, is sent to a physician who specializes in interpreting these images, called a radiologist. The image may be on plain photographic film or digital mammography on a computer screen; despite the much higher cost of the digital systems, the two methods are generally considered equally effective. The equipment may use a computer-aided diagnosis (CAD) system.
There is considerable variation in interpreting the images; the same image may be declared normal by one radiologist and suspicious by another. It can be helpful to compare the images to any previously taken images, as changes over time may be significant.
If a suspicious signs are identified in the image, then the woman is usually recalled for a second mammogram, sometimes after waiting six months to see whether the spot is growing, or a biopsy of the breast.[6] Most of these will prove to be false positives, resulting in sometimes debilitating anxiety over nothing. Most women recalled will undergo additional imaging only, without any further intervention. Recall rates are higher in the U.S. than in the UK.[7]
Whether it works
On balance, screening mammography in older women noticeably increases medical treatment and saves a small number of lives. Usually, it has no effect on the outcome of the cancer. Screening targeted towards women with above-average risk produces more benefit than screening of women at normal or low risk for breast cancer.
A 2009 Cochrane review estimated that mammography in women between 50 and 75 years old results in a relative risk reduction of death from breast cancer of 15% or an absolute risk reduction of 0.05%. Those who have mammograms however end up with increased surgeries, chemotherapy, radiotherapy and other potentially procedures resulting from the over-detection of harmless lumps. Many women will experience important psychological distress for many months because of false positive findings.[2] Consequently, the value of routine mammography in women at low or average risk is controversial.[2] With unnecessary treatment of ten women for every one woman whose life was prolonged, the authors concluded that routine mammography may do more harm than good.[2]
If 1,000 women in their 50s are screened every year for ten years, the following outcomes are considered typical in the developed world:[8]
- One woman's life will be extended due to earlier detection of breast cancer.
- 2–10 women will be overdiagnosed and needlessly treated for a cancer that would have stopped growing on its own or otherwise caused no harm during the woman's lifetime.
- 5–15 women will be treated for breast cancer, with the same outcome as if they had been detected after symptoms appeared.
- 250–500 will be incorrectly told they might have breast cancer (false positive).
- 125–250 will undergo breast biopsy.
The outcomes are worse for women in their 20s, 30s, and 40s, as they are far less likely to have a life-threatening breast cancer, and more likely to have dense breasts that make interpreting the mammogram more difficult. Among women in their 60s, who have a somewhat higher rate of breast cancer, the proportion of positive outcomes to harms are better:[9]
- For women in their 40s: 2,000 women would need to be screened every year for 10 years to prevent one death from breast cancer. 1,000 of these women would experience false results and 250 healthy women would undergo unnecessary biopsies.
- For women in their 50s: 1,339 women would need to be screened for every year for 10 years to prevent one death from breast cancer. Half of these women would experience false positives and one quarter would undergo unnecessary biopsies.
- For women in their 60s: 377 women would need to be screened for every year for 10 years to prevent one death from breast cancer. Half of these women would experience false positives and one quarter would undergo unnecessary biopsies.
Mammography is not generally considered as an effective screening technique for women at average or low risk of developing cancer who are less than 50 years old. For normal-risk women 40 to 49 years of age, the risks of mammography outweigh the benefits,[10] and the US Preventive Services Task Force says that the evidence in favor of routine screening of women under the age of 50 is "weak".[11] Part of the difficulty in interpreting mammograms in younger women stems from breast density. Radiographically, a dense breast has a preponderance of glandular tissue, and younger age or estrogen hormone replacement therapy contribute to mammographic breast density. After menopause, the breast glandular tissue gradually is replaced by fatty tissue, making mammographic interpretation much more accurate.
What is recommended
Different countries and organizations make different recommendations about screening mammography. The most important differences are the age at which it should begin and how frequently it should be performed in women at typical risk for developing breast cancer.
In the UK, all women are invited for screening once every three years beginning at age 50. As of 2009 the United States Preventive Services Task Force recommends that women over the age of 50 receive mammography once every two years.[11] Some other organizations recommend mammograms begin as early as age 40 in normal-risk women, and take place more frequently, up to once each year.
Women at higher risk may benefit from earlier or more frequent screening. Women with one or more first-degree relatives (mother, sister, daughter) with premenopausal breast cancer often begin screening at an earlier age, perhaps at an age 10 years younger than the age when the relative was diagnosed with breast cancer.
Health programs
In 2005, about 68% of all U.S. women age 40–64 had a mammogram in the past two years (75% of women with private health insurance, 56% of women with Medicaid insurance, 38% of currently uninsured women, and 33% of women uninsured for more than 12 months).[12] All U.S. states except Utah require private health insurance plans and Medicaid to pay for breast cancer screening.[13] As of 1998, Medicare (available to those aged 65 or older or who have been on Social Security Disability Insurance for over 2 years) pays for annual screening mammography in women aged 40 or older.
All organized breast cancer screening programs in Canada offer clinical breast examinations for women aged 40 and over and screening mammography every two years for women aged 50–69.[14] In 2003, about 61% of women aged 50–69 in Canada reported having had a mammogram within the past two years.[15]
The UK's NHS Breast Screening Programme, the first of its kind in the world, began in 1988 and achieved national coverage in the mid-1990s. It provides free breast cancer screening mammography every three years for all women in the UK aged 50 and over.[16] As 2006, about 76% of women aged 53–64 resident in England had been screened at least once in the previous three years.[17]
The Australian national breast screening program, BreastScreen Australia, was commenced in the early 1990s and invites women aged 50–69 to screening every 2 years. No routine clinical examination is performed, and the cost of screening is free to the point of diagnosis.
The Singapore national breast screening program, BreastScreen Singapore, is the only publicly funded national breast screening program in Asia, and enrolls women aged 50–64 for screening every two years. Like the Australian system, no clinical examination is performed routinely. Unlike most national screening systems, however, clients have to pay half of the cost of the screening mammogram; this is in line with the Singapore health system's core principle of co-payment for all health services.
Criticisms
Most women significantly overestimate both their own risk of dying from breast cancer and the effect screening mammography could have on it.[18] Some researchers worry that if women correctly understood that screening programs offer a small, but statistically significant benefit, more women would refuse to participate.[18]
The contribution of mammography to the early diagnosis of cancer is controversial, and for those found with benign lesions, mammography can create a high psychological and financial cost. Most women participating in mammography screening programs accept the risk of false positive recall, and the majority do not find it very distressing.[citation needed] Many patients find the recall very frightening, and are intensely relieved to discover that it was a false positive, as about 90% of women do.[19]
A major effect of routine breast screening is to greatly increase the rate of early breast cancer detection, in particular for non-invasive ductal carcinoma in situ (DCIS), sometimes called "pre-breast cancer", which is almost never forms a lump and which generally cannot be detected except through mammography. While this ability to detect such very early breast malignancies is at the heart of claims that screening mammography can improve survival from breast cancer, it is also controversial. This is because a very large proportion of such cases will not progress to kill the patient, and thus mammography cannot be genuinely claimed to have saved any lives in such cases; in fact, it would lead to increased sickness and unnecessary surgery for such patients.
Consequently, finding and treating many cases of DCIS represents overdiagnosis and overtreatment. Treatment is given to all women with DCIS because it is currently impossible to predict which patients with DCIS will have an indolent, non-fatal course, and which few will inevitably progress to invasive cancer and premature death if left untreated. Consequently, all patients with DCIS are treated in much the same way, with at least wide local excision, and sometimes mastectomy if the DCIS is very extensive. The cure rate for DCIS if treated appropriately is extremely high, partly because the majority of DCIS cases were harmless in the first place.
The phenomenon of finding pre-invasive malignancy or nonmalignant benign disease is commonplace in all forms of cancer screening, including pap smears for cervical cancer, fecal occult blood testing for colon cancer, and prostate-specific antigen testing for prostate cancer. All of these tests have the potential to detect asymptomatic cancers, and all of them have a high rate of false positives and lead to invasive procedures that are unlikely to benefit the patient.
Molecular breast imaging
Molecular breast imaging is a nuclear medicine technique that is currently under study. It shows promising results for imaging people with dense breast tissue and may have accuracies comparable to MRI.[20] MBI is claimed to be cheaper than MRI.[21]
Ultrasonography
Medical ultrasonography (Ultrasound) is a diagnostic aid to mammography.
Breast MRI
Magnetic resonance imaging (MRI) has been shown to detect cancers not visible on mammograms. The chief strength of breast MRI is its very high negative predictive value. A negative MRI can rule out the presence of cancer to a high degree of certainty, making it an excellent tool for screening in patients at high genetic risk or radiographically dense breasts, and for pre-treatment staging where the extent of disease is difficult to determine on mammography and ultrasound. MRI can diagnose benign proliferative change, fibroadenomas, and other common benign findings at a glance, often eliminating the need for costly and unnecessary biopsies or surgical procedures. The spatial and temporal resolution of breast MRI has increased markedly in recent years, making it possible to detect or rule out the presence of small in situ cancers, including ductal carcinoma in situ.
However, breast MRI has long been regarded to have disadvantages. For example, although it is 27–36% more sensitive, it has been claimed to be less specific than mammography.[22] As a result, MRI studies may have more false positives (up to 30%), which may have undesirable financial and psychological costs. It is also a relatively expensive procedure, and one which requires the intravenous injection of gadolinium, which has been implicated in a rare reaction called nephrogenic systemic fibrosis. Although NSF is extremely uncommon, patients with a history of renal disease may not be able to undergo breast MRI. Further, an MRI may not be used for screening patients with a pacemaker or breast reconstruction patients with a tissue expander due to the presence of metal.
Proposed indications for using MRI for screening include:[23]
- Strong family history of breast cancer
- Patients with BRCA-1 or BRCA-2 oncogene mutations
- Evaluation of women with breast implants
- History of previous lumpectomy or breast biopsy surgeries
- Axillary metastasis with an unknown primary tumor
- Very dense or scarred breast tissue
In addition, breast MRI may be helpful for screening in women who have had breast augmentation procedures involving intramammary injections of various foreign substances that may mask the appearances of breast cancer on mammography and/or ultrasound. These substances include silicone oil and polyacrylamide gel.
Two studies published in 2007 demonstrated the strengths of MRI-based screening:
- In March 2007, an article published in the New England Journal of Medicine demonstrated that in 3.1% of patients with breast cancer, whose contralateral breast was clinically and mammographically tumor-free, MRI could detect breast cancer. Sensitivity for detection of breast cancer in this study was 91%, specificity 88%.[24]
- In August 2007, an article published in The Lancet compared MRI breast cancer screening to conventional mammographic screening in 7,319 women. MRI screening was highly more sensitive (97% in the MRI group vs. 56% in the mammography group) in recognizing early high-grade Ductal Carcinoma in situ (DCIS), the most important precursor of invasive carcinoma. Despite the high sensitivity, MRI screening had a positive predictive value of 52%, which is totally accepted for cancer screening tests.[25] The author of a comment published in the same issue of The Lancet concludes that "MRI outperforms mammography in tumour detection and diagnosis."[26]
Based on this evidence, and the lack of effective alternative methods for screening in young women of very high genetic risk (either an extremely strong first degree family history or proven BRCA1 or BRCA2 oncogene mutation carrier status) for breast cancer, the Australian federal government decided to routinely reimburse annual breast MRI scans for such women under the age of 50 from January 2009 onwards.
BRCA testing
Genetic testing does not detect cancers, but may reveal a propensity to develop cancer. Women who are known to have a higher risk of developing breast cancer usually undertake more aggressive screening programs.
A clinical practice guideline by the US Preventive Services Task Force recommends against routine referral for genetic counseling or routine testing for BRCA mutations, on fair evidence that the harms outweigh the benefits.[27] It also encourages a referral for counseling and testing in women whose a family history that indicates they have an increased risk of a BRCA mutation, on fair evidence of benefit.[27] About 2% of American women have family histories that indicate an increased risk of having a medically significant BRCA mutation.[27]
References
- ^ a b Kösters JP, Gøtzsche PC (2003). Kösters, Jan Peter. ed. "Regular self-examination or clinical examination for early detection of breast cancer". Cochrane Database Syst Rev (2): CD003373. doi:10.1002/14651858.CD003373. PMID 12804462.
- ^ a b c d Gøtzsche PC, Nielsen M (2009). Gøtzsche, Peter C. ed. "Screening for breast cancer with mammography". Cochrane Database Syst Rev (4): CD001877. doi:10.1002/14651858.CD001877.pub3. PMID 19821284.
- ^ "Breast Cancer: Screening". United States Preventive Services Task Force. http://www.ahrq.gov/clinic/USpstf/uspsbrca.htm.
- ^ Schonberg M. Breast cancer screening: at what age to stop? Consultant. 2010;50(May):196-205.
- ^ Saslow D, Hannan J, Osuch J, et al. (2004). "Clinical breast examination: practical recommendations for optimizing performance and reporting". CA Cancer J Clin 54 (6): 327–44. doi:10.3322/canjclin.54.6.327. PMID 15537576.
- ^ Croswell JM, Kramer BS, Kreimer AR, et al. (2009). "Cumulative incidence of false-positive results in repeated, multimodal cancer screening". Ann Fam Med 7 (3): 212–22. doi:10.1370/afm.942. PMC 2682972. PMID 19433838. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2682972.
- ^ Smith-Bindman R, Ballard-Barbash R, Miglioretti DL, Patnick J, Kerlikowske K (2005). "Comparing the performance of mammography screening in the USA and the UK". Journal of Medical Screening 12 (1): 50–4. doi:10.1258/0969141053279130. PMID 15814020.
- ^ Welch, H. Gilbert; Woloshin, Steve; Schwartz, Lisa A. (2011). Overdiagnosed: Making People Sick in the Pursuit of Health. Beacon Press. p. 149. ISBN 0-8070-2200-4.
- ^ Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L (November 2009). "Screening for breast cancer: an update for the U.S. Preventive Services Task Force". Ann. Intern. Med. 151 (10): 727–37, W237–42. doi:10.1059/0003-4819-151-10-200911170-00009. PMC 2972726. PMID 19920273. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2972726.
- ^ Armstrong K, Moye E, Williams S, Berlin JA, Reynolds EE (2007). "Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians". Ann. Intern. Med. 146 (7): 516–26. PMID 17404354.
- ^ a b US Preventive Services Task Force (November 2009). "Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement". Ann. Intern. Med. 151 (10): 716–26, W–236. doi:10.1059/0003-4819-151-10-200911170-00008. PMID 19920272.
- ^ Ward E, Halpern M, Schrag N, Cokkinides V, DeSantis C, Bandi P, Siegel R, Stewart A, Jemal A (January—February 2008). "Association of insurance with cancer care utilization and outcomes". CA Cancer J Clin 58 (1): 9–31. doi:10.3322/CA.2007.0011. PMID 18096863. http://caonline.amcancersoc.org/cgi/content/full/CA.2007.0011v1.
- ^ Kaiser Family Foundation (December 31, 2006). "State Mandated Benefits: Cancer Screening for Women, 2006". http://www.statehealthfactsonline.org/comparemaptable.jsp?ind=488&cat=10&yr=17&typ=5.
- ^ Canadian Cancer Society (August 10, 2007). "Breast cancer screening in your 40s". http://www.cancer.ca/ccs/internet/standard/0,3182,3172_573785695_2026817819_langId-en,00.html.
- ^ Canadian Cancer Society (April 2006). "Canadian Cancer Statistics, 2006" (PDF). http://www.cancer.ca/vgn/images/portal/cit_86751114/31/21/935505792cw_2006stats_en.pdf.pdf.
- ^ NHS Cancer Screening Programmes (2007). "NHS Breast Screening Programme". http://cancerscreening.org.uk/breastscreen/.
- ^ The Information Centre (NHS) (March 23, 2007). "Breast Screening Programme 2005/06". http://www.ic.nhs.uk/statistics-and-data-collections/screening/breast-cancer/breast-screening-programme-2005-06-%5Bns%5D?.
- ^ a b "Women 'misjudge screening benefits'". BBC News. 15 October 2001. http://news.bbc.co.uk/1/hi/health/1601267.stm. Retrieved 2007-04-04.
- ^ Welch, 2011. pp. 177–178.
- ^ O'Connor, M; Rhodes, D, Hruska, C (2009 Aug). "Molecular breast imaging.". Expert review of anticancer therapy 9 (8): 1073–80. doi:10.1586/era.09.75. PMC 2748346. PMID 19671027. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2748346.
- ^ "Molecular Breast Imaging More Effective than Mammography at Detecting Cancer in High-Risk Women with Dense Breasts". http://newsblog.mayoclinic.org/2008/09/03/breast-cancer-molecular-breast-imaging-mammography/.
- ^ Hrung J, Sonnad S, Schwartz J, Langlotz C (1999). "Accuracy of MR imaging in the work-up of suspicious breast lesions: a diagnostic meta-analysis". Acad Radiol 6 (7): 387–97. doi:10.1016/S1076-6332(99)80189-5. PMID 10410164.
- ^ Morrow M (2004). "Magnetic resonance imaging in breast cancer: one step forward, two steps back?". JAMA 292 (22): 2779–80. doi:10.1001/jama.292.22.2779. PMID 15585740.
- ^ Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L, Peacock S, Smazal SF, Maki DD, Julian TB, DePeri ER, Bluemke DA, Schnall MD (2007). "MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer". N Engl J Med. 356 (13): 1295–1303. doi:10.1056/NEJMoa065447. PMID 17392300.
- ^ Kuhl CK, Schrading S, Bieling HB, Wardelmann E, Leutner CC, Koenig R, Kuhn W, Schild HH (2007). "MRI for diagnosis of pure ductal carcinoma in situ: a prospective observational study". The Lancet 370 (9586): 485–492. doi:10.1016/S0140-6736(07)61232-X. PMID 17693177.
- ^ Boetes C, Mann RM (2007). "Ductal carcinoma in situ and breast MRI". The Lancet 370 (9586): 459–460. doi:10.1016/S0140-6736(07)61207-0.
- ^ a b c "Genetic Risk Assessment and BRCA Mutation Testing for Breast and Ovarian Cancer Susceptibility: Recommendation Statement". Agency for Healthcare Research and Quality (United States Preventive Services Task Force). September 2005. http://www.uspreventiveservicestaskforce.org/uspstf05/brcagen/brcagenrs.htm. Retrieved 2011-03-07.
External links
- Breast cancer at the Open Directory Project
- Breast cancer screening page from the National Cancer Institute
- Breast Cancer Screening from AARP.org
Tumors: breast cancer (C50/D24, 174–175/217) – Histopathologic classification Fibroepithelial/stromal Ductal, lobular, and medullary Intraductal papillomaInvasive lobular carcinoma (ILC)MedullaryOther/ungroupedPrecursor lesions Atypical ductal hyperplasiaOther Related subjects Main article · Classification · Risk factors (Alcohol · Hereditary breast-ovarian cancer syndrome · BRCA mutation) · Screening · Treatment
Pathology: Tumor, Neoplasm, Cancer, and Oncology (C00–D48, 140–239) Conditions Malignant progressionTopographyHead/Neck (Oral, Nasopharyngeal) · Digestive system · Respiratory system · Bone · Skin · Blood · Urogenital · Nervous system · Endocrine systemHistologyOtherPrecancerous condition · Paraneoplastic syndromeStaging/grading Carcinogenesis Misc. M: NEO
tsoc, mrkr
tumr, epon, para
drug (L1i/1e/V03)
Categories:- Breast cancer
- Ribbon symbolism
- Cancer screening
Wikimedia Foundation. 2010.