- Basal-cell carcinoma
-
Basal-cell carcinoma Classification and external resources
A basal-cell carcinomaICD-10 C44 (ILDS C44.L21) ICD-9 173 ICD-O: M8090/3-8093/3 OMIM 605462 DiseasesDB 1264 MedlinePlus 000824 eMedicine med/214 MeSH D002280 Basal-cell carcinoma is the most common type of skin cancer. It rarely metastasizes or kills. However, because it can cause significant destruction and disfigurement by invading surrounding tissues, it is still considered malignant.[1][2] Statistically, approximately 3 out of 10 Caucasians may develop a basal-cell cancer within their lifetime.[3] In 80 percent of all cases, basal-cell cancers are found on the head and neck.[3] There appears to be an increase in the incidence of basal-cell cancer of the trunk (torso) in recent years.[3]
Contents
Classification
Basal-cell carcinomas may be divided into the following types:[4][5]:646-650
- Nodular basal-cell carcinoma (Classic basal-cell carcinoma)
- Cystic basal-cell carcinoma
- Cicatricial basal-cell carcinoma (Morpheaform basal-cell carcinoma, Morphoeic basal-cell carcinoma)
- Infiltrative basal-cell carcinoma
- Micronodular basal-cell carcinoma
- Superficial basal-cell carcinoma (Superficial multicentric basal-cell carcinoma)
- Pigmented basal-cell carcinoma
- Rodent ulcer (Jacobi ulcer)
- Fibroepithelioma of Pinkus
- Polypoid basal-cell carcinoma
- Pore-like basal-cell carcinoma
- Aberrant basal-cell carcinoma
For simplicity, one can also divide basal-cell carcinoma into 3 groups, based on location and difficulty of therapy:
- Superficial basal-cell carcinoma, or some might consider to be equivalent to "in-situ". Very responsive to topical chemotherapy such as Aldara, or Fluorouracil. It is the only type of basal-cell cancer that can be effectively treated with topical chemotherapy.
- Infiltrative basal-cell carcinoma, which often encompasses morpheaform and micronodular basal-cell cancer. More difficult to treat with conservative treatment methods such as electrodessiccation and currettage, or with currettage alone.
- Nodular basal-cell carcinoma, which essentially includes most of the remaining categories of basal-cell cancer. It is not unusual to encounter morphologic features of several variants of basal-cell cancer in the same tumor.
See also:
- Nevoid basal-cell carcinoma syndrome
Signs and symptoms
Patients present with a shiny, pearly nodule. However, superficial basal-cell cancer can present as a red patch like eczema. Infiltrative or morpheaform basal-cell cancers can present as a skin thickening or scar tissue – making diagnosis difficult without using tactile sensation and a skin biopsy. It is often difficult to distinguish basal-cell cancer from acne scar, actinic elastosis, and recent cryodestruction inflammation.
Distribution
About two thirds of basal-cell carcinomas occur on sun-exposed areas of the body. One-third occur on areas of the body that are not exposed to sunlight, emphasizing the genetic susceptibility of basal-cell cancer patients.
Diagnosis
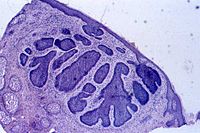
To diagnose basal-cell carcinomas, a skin biopsy is taken for pathological study. The most common method is a shave biopsy under local anesthesia. Most nodular basal-cell cancers can be diagnosed clinically; however, other variants can be very difficult to distinguish from benign lesions such as intradermal nevus, sebaceomas, fibrous papules, early acne scars, and hypertrophic scarring.[6]
Pathophysiology
Basal-cell carcinomas develop in the basal cell layer of the skin. Sun light exposure leads to the formation of thymine dimers, a form of DNA damage. While DNA repair removes most UV-induced damage, not all crosslinks are excised. There is, therefore, cumulative DNA damage leading to mutations. Apart from the mutagenesis, sunlight depresses the local immune system, possibly decreasing immune surveillance for new tumor cells.
Basal-cell carcinoma also develops as a result of Basal-Cell Nevus Syndrome, or Gorlin Syndrome, which is also characterized by keratocystic odontogenic tumors of the jaw, palmar or plantar (sole of the foot) pits, calcification of the falx cerebri (in the center line of the brain) and rib abnormalities. The cause of the syndrome is a mutation in the PTCH1 tumor-suppressor gene at chromosome 9q22.3, which inhibits the hedgehog signaling pathway. A mutation in the SMO gene, which is also on the hedgehog pathway, also causes basal-cell carcinoma.[7]
Prevention
Basal-cell carcinoma is the most common skin cancer. It occurs mainly in fair-skinned patients with a family history of this cancer. Sunlight is a factor in about two-thirds of these cancers; therefore, doctors recommend sun screens with at least SPF 30. One-third occur in non-sun-exposed areas.
The use of a chemotherapeutic agent such as 5-Fluorouracil or Imiquimod, can prevent development of skin cancer. It is usually recommended to individuals with extensive sun damage, history of multiple skin cancers, or precancerous growths. It is often repeated every 2 to 3 years to further decrease the risk of skin cancer.
Treatment
The following methods are employed in the treatment of basal-cell carcinoma (BCC):
- Standard surgical excision with either frozen section histology, or paraffin embedded fixed tissue pathology. This is the preferred method for removal of most BCCs. The cure rate for this method, whether done by a plastic surgeon, family doctor, or dermatologist is totally dependent on the surgical margin. When standard surgical margin is applied (usually 4 mm or more),[8] a high cure rate can be achieved with standard excision[9][10] A dermatoscope can help an experienced surgeon accurately identify the visible tumour that the naked eye can not see.[11][12] The narrower the free surgical margin (skin removed that is free of visible tumor) the higher the recurrence rate.[13][14][15][16] A weakness with standard surgical excision is the high recurrence rate of basal-cell cancers of the face, especially around eyelids,[17] nose, and facial structures.[18] A diagram on page 33 of the NCCN publication demonstrate the area of high risk of recurrence as most the face with the exception of the central cheek and upper forehead.[9][19] On the face, or on recurrent basal-cell cancer after previous surgery, special surgical margin controlled processing (CCPDMA - complete circumferential peripheral and deep margin assessment[19][20])[21] using frozen section histology (Mohs surgery is one of the methods) is required.[22][23] With surgical margin controlled frozen section histology, a surgeon can achieve a high cure rate and low recurrence rate on the same day of the excision.[24] However, most standard excisions done in a plastic surgeon or dermatologist's office are sent to an outside laboratory for standard bread loafing method of processing.[25] This method has a high "false negative" rate due to the random sampling of the tumour. It is likely that less than 5% of the surgical margin is examined, as each slice of tissue is only 6 micrometres thick, about 3 to 4 serial slices are obtained per section, and only about 3 to 4 sections are obtained per specimen (see figure 2 of reference[26]). Usually, the rule of thumb is if a 4 mm free surgical margin is obtained around a small tumor (less than 6mm), or a wider 6 mm free surgical margin is obtained around a larger tumor (greater than 6mm), the cure rate is very high - 95% or better.[27][28][29] For cosmetic reasons, many doctors take only very small surgical margins 1–2 mm,[30] especially when facial tumour is being removed. A pathology report from such a case indicating "margins free of residual tumour", often is inaccurate, and a high recurrence rate of up to 38% might occur.[8][17][30][31] When in doubt, a patient should demand that either Mohs surgery or frozen section histology with either margin control (ccpdma) or thin serial bread-loafing is utilized when dealing with a tumour on the face.[9] The pathologist processing the frozen section specimen should cut multiple sections through the block to minimize the false negative error rate. Or one should simply process the tissue utilizing a method approximating the Mohs method (described in most basic histopathology text books or described in this reference [22]) during frozen section processing. Unfortunately, these methods are difficult when applied to frozen sections; and is very tedious to process. When not utilizing frozen section, the surgeon might have to wait a week or more, before informing the patient if more tumour is left, or if the surgical margin is too narrow.[32] And a second surgery must be performed to remove the residual or potential residual tumour once the surgeon inform the patient of the positive or narrow surgical margin on the surgical pathology report.
- Mohs surgery: Mohs surgery (or Mohs micrographic surgery) is an outpatient procedure in which the tumor is surgically excised and then immediately examined under a microscope. It is a form of pathology processing called CCPDMA. It is claimed to have the highest cure rate of 97% to 99.8% by some individuals[who?]. The base and edges are microscopically examined to verify sufficient margins before the surgical repair of the site. If the margins are insufficient, more is removed from the patient until the margins are sufficient. It is also used for squamous-cell carcinoma; however, the cure rate is not as high as Mohs surgery for basal-cell carcinoma.
- Chemotherapy: Some superficial cancers respond to local therapy with 5-fluorouracil, a chemotherapy agent. Topical treatment with 5% Imiquimod cream, with five applications per week for six weeks has a reported 70-90% success rate at reducing, even removing, the BCC [basal-cell carcinoma]. Both Imiquimod and 5-fluorouracil have received FDA approval for the treatment of superficial basal-cell carcinoma. Off label use of imiquimod on invasive basal-cell carcinoma has been reported. Imiquimod may be used prior to surgery in order to reduce the size of the carcinoma. One can expect a great deal of inflammation with this treatment.[33] Chemotherapy often follows Mohs surgery to eliminate the residual superficial basal-cell carcinoma after the invasive portion is removed. Some advocate the use of imiquimod prior to Mohs surgery to remove the superficial component of the cancer[34] Removing the residual superficial tumor with surgery alone can result in large and difficult to repair surgical defects. One often waits a month or more after surgery before starting the Imiquimod or 5-fluorouracil to make sure the surgical wound has adequately healed. Some individuals[who?] advocate the use of curettage (see EDC below) first, then followed by chemotherapy. These experimental procedure likely will result in better cure rate than one alone, but are not standard care.
- Immunotherapy: Immunotherapy research suggests that treatment using Euphorbia peplus, a common garden weed, may be effective.[35] Australian biopharmaceutical company Peplin[36] is developing this as topical treatment for BCC. Imiquimod or Aldara is an immunotherapy but is listed here under chemotherapy.
- Radiation: Radiation therapy is appropriate for all forms of BCC as adequate doses will eradicate the disease. Radiation therapy can be delivered either as external beam radiotherapy or as brachytherapy (internal radiotherapy). Although radiotherapy is generally used in older patients who are not candidates for surgery, it is also used in cases where surgical excision will be disfiguring or difficult to reconstruct (especially on the tip of the nose, and the nostril rims). Radiation treatment often takes as few as 5 visits to as many as 25 visits for radiation therapy. Usually, the more visits scheduled for therapy, the less complication or damage is done to the normal tissue supporting the tumor. Radiotherapy can also be useful if surgical excision has been done incompletely or if the pathology report following surgery suggests a high risk of recurrence, for example if nerve involvement has been demonstrated. Cure rate can be as high as 95% for small tumor, or as low as 80% for large tumors. Usually, recurrent tumors after radiation are treated with surgery, and not with radiation. Further radiation treatment will further damage normal tissue, and the tumor might be resistant to further radiation.
- Photodynamic therapy: Photodynamic therapy is a new modality for treatment of basal-cell carcinoma, which is administrated by application of photosensitizers to the target area. When these molecules are activated by light, they become toxic, therefore destroy the target cells. Methyl aminolevulinate is approved by EU as a photosensitizer since 2001. This therapy is also used in other skin cancer types.[37]
- Cryosurgery: Cryosurgery is an old modality for the treatment of many skin cancers. When accurately utilized with a temperature probe and cryotherapy instruments, it can result in very good cure rate. Disadvantages include lack of margin control, tissue necrosis, over or under treatment of the tumor, and long recovery time. Overall, there are sufficient data to consider cryosurgery as a reasonable treatment for BCC. There are no good studies, however, comparing cryosurgery with other modalities, particularly with Mohs surgery, excision, or electrodesiccation and curretage so that no conclusion can be made whether cryosurgery is as efficacious as other methods. Also, there is no evidence on whether curetting the lesions before cryosurgery affects the efficacy of treatment.[38] Several textbooks are published on the therapy, and a few physicians still apply the treatment to selected patients.[39]
- Electrodesiccation and curettage: or EDC is accomplished by using a round knife, or curette, to scrape away the soft cancer. The skin is then burned with an electric current. This further softens the skin, allowing for the knife to cut more deeply with the next layer of curettage. The cycle is repeated, with a safety margin of curettage of normal skin around the visible tumor. This cycle is repeated 3 to 5 times, and the free skin margin treated is usually 4 to 6 mm. Cure rate is very much user dependent and depends on the size and type of tumor. Infiltrative or morpheaform BCCs can be difficult to eradicate with EDC. Generally, this method is used on cosmetically unimportant areas like the trunk (torso). Some physicians believe that it is acceptable to utilize EDC on the face of elderly patients over the age of 70. However, with increasing life expectancy, such an objective criterion cannot be supported. The cure rate can be low or high, depending on the aggressiveness of the EDC and the free margin treated. Some advocate curettage alone without electrodesiccation, and with the same cure rate.[40]
Treating surgeons will recommend one of these modalities as appropriate treatment depending on the tumour size, location, patient age, and other variables.
Prognosis
Prognosis is excellent if the appropriate method of treatment is used in early primary basal-cell cancers. Recurrent cancers are much harder to cure, with a higher recurrent rate with any methods of treatment. Although basal-cell carcinoma rarely metastasizes, it grows locally with invasion and destruction of local tissues. The cancer can impinge on vital structures like nerves and result in loss of sensation or loss of function or rarely death. The vast majority of cases can be successfully treated before serious complications occur. The recurrence rate for the above treatment options ranges from 50 percent to 1 percent or less.
Epidemiology
Basal-cell cancer is the most common skin cancer. It is much more common in fair-skinned individuals with a family history of basal-cell cancer and increases in incidence closer to the equator or at higher altitude. According to Skin Cancer Foundation, there are approximately 800,000[41] new cases yearly in the United States alone. Up to 30% of caucasians develop basal-cell carcinomas in their lifetime.[3] In Canada, the most common skin cancer is basal cell carcinoma (as much as one third of all cancer diagnoses), affecting 1 in 7 individuals over a lifetime. [42][43]
Most sporadic BCC arises in small numbers on sun-exposed skin of people over age 50, although younger people may also be affected. The development of multiple basal-cell cancer at an early age could be indicative of Nevoid basal-cell carcinoma syndrome.
References
- ^ MedlinePlus Encyclopedia Basal cell carcinoma
- ^ "Basal Cell Carcinoma - Symptoms, Treatment and Prevention". http://www.healthscout.com/ency/1/199/main.html.
- ^ a b c d Wong CS, Strange RC, Lear JT (October 2003). "Basal cell carcinoma". BMJ 327 (7418): 794–8. doi:10.1136/bmj.327.7418.794. PMC 214105. PMID 14525881. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=214105.
- ^ Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ^ http://www.skincancerguide.ca/basal/what_is_basal_cell_cancer.html
- ^ Epstein EH, Shepard JA, Flotte TJ (Jan 2008). "Case records of the Massachusetts General Hospital. Case 3-2008. An 80-year-old woman with cutaneous basal-cell carcinomas and cysts of the jaws". N Engl J Med 358 (4): 393–401. doi:10.1056/NEJMcpc0707893. PMID 18216361.
- ^ a b Wolf DJ, Zitelli JA (March 1987). "Surgical margins for basal cell carcinoma". Arch Dermatol 123 (3): 340–4. doi:10.1001/archderm.123.3.340. PMID 3813602. http://archderm.ama-assn.org/cgi/pmidlookup?view=long&pmid=3813602.
- ^ a b c http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf
- ^ Silverman MK, Kopf AW, Bart RS, Grin CM, Levenstein MS (June 1992). "Recurrence rates of treated basal cell carcinomas. Part 3: Surgical excision". J Dermatol Surg Oncol 18 (6): 471–6. PMID 1592998.
- ^ Scalvenzi M, Lembo S, Francia MG, Balato A (October 2008). "Dermoscopic patterns of superficial basal cell carcinoma". Int. J. Dermatol. 47 (10): 1015–8. doi:10.1111/j.1365-4632.2008.03731.x. PMID 18986346.
- ^ Cuellar F, Vilalta A, Puig S, Palou J, Zaballos P, Malvehy J (September 2008). "Dermoscopy of early recurrent basal cell carcinoma". Arch Dermatol 144 (9): 1254. doi:10.1001/archderm.144.9.1254. PMID 18794487.
- ^ Maloney ME, et al. (1999). Surgical Dermatopathology. Cambridge, MA: Blackwell Publishers. p. 110. ISBN 0-86542-299-0.
- ^ Kimyai-Asadi A, Katz T, Goldberg LH, et al. (December 2007). "Margin involvement after the excision of melanoma in situ: the need for complete en face examination of the surgical margins". Dermatol Surg 33 (12): 1434–9; discussion 1439–41. doi:10.1111/j.1524-4725.2007.33313.x. PMID 18076608.
- ^ Mosterd K, Krekels GA, Nieman FH, et al. (December 2008). "Surgical excision versus Mohs' micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years' follow-up". Lancet Oncol. 9 (12): 1149–56. doi:10.1016/S1470-2045(08)70260-2. PMID 19010733.
- ^ Kimyai-Asadi A, Goldberg LH, Jih MH (September 2005). "Accuracy of serial transverse cross-sections in detecting residual basal cell carcinoma at the surgical margins of an elliptical excision specimen". J. Am. Acad. Dermatol. 53 (3): 469–74. doi:10.1016/j.jaad.2005.02.049. PMID 16112355.
- ^ a b Sigurdsson H, Agnarsson BA (August 1998). "Basal cell carcinoma of the eyelid. Risk of recurrence according to adequacy of surgical margins". Acta Ophthalmol Scand 76 (4): 477–80. doi:10.1034/j.1600-0420.1998.760416.x. PMID 9716337.
- ^ Farhi D, Dupin N, Palangié A, Carlotti A, Avril MF (October 2007). "Incomplete excision of basal cell carcinoma: rate and associated factors among 362 consecutive cases". Dermatol Surg 33 (10): 1207–14. doi:10.1111/j.1524-4725.2007.33255.x. PMID 17903153. http://www3.interscience.wiley.com/journal/118489368/abstract.
- ^ a b http://wwwu.tsgh.ndmctsgh.edu.tw/commcpc/images/nccn/Non-Melanoma%20Skin%20Cancer-2007.pdf
- ^ http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf pages 6 and 7
- ^ Dhingra N, Gajdasty A, Neal JW, Mukherjee AN, Lane CM (June 2007). "Confident complete excision of lid-margin BCCs using a marginal strip: an alternative to Mohs' surgery". Br J Ophthalmol 91 (6): 794–6. doi:10.1136/bjo.2006.109892. PMC 1955612. PMID 17229804. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1955612.
- ^ a b Bentkover SH, Grande DM, Soto H, Kozlicak BA, Guillaume D, Girouard S (2002). "Excision of head and neck basal cell carcinoma with a rapid, cross-sectional, frozen-section technique". Arch Facial Plast Surg 4 (2): 114–9. doi:10.1001/archfaci.4.2.114. PMID 12020207. http://archfaci.ama-assn.org/cgi/pmidlookup?view=long&pmid=12020207.
- ^ Minton TJ (August 2008). "Contemporary Mohs surgery applications". Curr Opin Otolaryngol Head Neck Surg 16 (4): 376–80. doi:10.1097/MOO.0b013e3283079cac. PMID 18626258. http://journals.lww.com/co-otolaryngology/pages/articleviewer.aspx?year=2008&issue=08000&article=00013&type=abstract.
- ^ Nagore E, Grau C, Molinero J, Fortea JM (March 2003). "Positive margins in basal cell carcinoma: relationship to clinical features and recurrence risk. A retrospective study of 248 patients". J Eur Acad Dermatol Venereol 17 (2): 167–70. doi:10.1046/j.1468-3083.2003.00535.x. PMID 12705745. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0926-9959&date=2003&volume=17&issue=2&spage=167.
- ^ Lane JE, Kent DE (2005). "Surgical margins in the treatment of nonmelanoma skin cancer and mohs micrographic surgery". Curr Surg 62 (5): 518–26. doi:10.1016/j.cursur.2005.01.003. PMID 16125611.
- ^ Maloney ME, et al. (1999). "Determining Cancer at Surgical margin". Surgical Dermatopathology. Cambridge, MA: Blackwell Publishers. p. 113. ISBN 0-86542-299-0.
- ^ Skin Malignancies, Squamous Cell Carcinoma at eMedicine
- ^ Staub G, Revol M, May P, Bayol JC, Verola O, Servant JM (October 2008). "[Excision skin margin and recurrence rate of skin cancer: a prospective study of 844 cases]" (in French). Ann Chir Plast Esthet 53 (5): 389–98. doi:10.1016/j.anplas.2007.07.015. PMID 17961898.
- ^ http://www.bccancer.bc.ca/HPI/CancerManagementGuidelines/Skin/NonMelanoma/ManagementPolicies/start.htm
- ^ a b Griffiths RW, Suvarna SK, Stone J (2007). "Basal cell carcinoma histological clearance margins: an analysis of 1539 conventionally excised tumours. Wider still and deeper?". J Plast Reconstr Aesthet Surg 60 (1): 41–7. doi:10.1016/j.bjps.2006.06.009. PMID 17126265.
- ^ Hauben DJ, Zirkin H, Mahler D, Sacks M (January 1982). "The biologic behavior of basal cell carcinoma: analysis of recurrence in excised basal cell carcinoma: Part II". Plast. Reconstr. Surg. 69 (1): 110–6. PMID 7053498.
- ^ http://gateway.nlm.nih.gov/MeetingAbstracts/ma?f=102272107.html
- ^ [1]
- ^ Butler DF, Parekh PK, Lenis A (January 2009). "Imiquimod 5% cream as adjunctive therapy for primary, solitary, nodular nasal basal-cell carcinomas before Mohs micrographic surgery: a randomized, double blind, vehicle-controlled study". Dermatol Surg 35 (1): 24–9. doi:10.1111/j.1524-4725.2008.34378.x. PMID 19018814.
- ^ "Peplin's skin cancer gel trial a success". The Age (Melbourne). 1 May 2006. http://www.theage.com.au/news/Business/Peplins-skin-cancer-trial-a-success/2006/05/01/1146335660056.html.
- ^ Peplin
- ^ Peng Q, Juzeniene A, Chen J, et al. (2008). "Lasers in Medicine". Rep. Prog. Phys. 71 (056701): 056701. doi:10.1088/0034-4885/71/5/056701.
- ^ Kokoszka A, Scheinfeld N (June 2003). "Evidence-based review of the use of cryosurgery in treatment of basal cell carcinoma". Dermatol Surg 29 (6): 566–71. PMID 12786697.
- ^ http://www.webmd.com/cancer/cryosurgery-for-nonmelanoma-skin-cancer
- ^ Barlow JO, Zalla MJ, Kyle A, DiCaudo DJ, Lim KK, Yiannias JA (June 2006). "Treatment of basal cell carcinoma with curettage alone". J. Am. Acad. Dermatol. 54 (6): 1039–45. doi:10.1016/j.jaad.2006.01.041. PMID 16713459.
- ^ Skin Cancer Foundation: Basal Cell Carcinoma
- ^ http://www.bccancer.bc.ca/HPI/CE/skincancer/skincancercourses/readings/preventionreadings/Epidemiology.htm
- ^ http://www.cancercare.on.ca/cms/one.aspx?pageId=9684
External links
Glandular and epithelial neoplasms (ICD-O 8010-8589) Epithelium Small cell carcinoma · Combined small cell carcinoma · Verrucous carcinoma · Squamous cell carcinoma · Basal cell carcinoma · Transitional cell carcinoma · Inverted papillomaGlands Other/multipleAdnexal and
skin appendage (8390-8429)Cystic, mucinous,
and serous (8440-8499)Cystic generalSerousOvarian serous cystadenoma/Pancreatic serous cystadenoma/Serous cystadenocarcinoma/Papillary serous cystadenocarcinomaDuctal, lobular,
and medullary (8500-8549)Lobular carcinoma in situ · Invasive lobular carcinomaAcinar cell (8550-8559)Other Complex epithelial (8560-8589)see also Template:Epithelium and epithelial tissueTumors: Skin neoplasm, Epidermis (C44.L12–L38/D23.L53-83, 173/216) Tumor BCCMicronodular basal cell carcinoma · Superficial basal cell carcinoma · Nodular basal cell carcinoma (Rodent ulcer) · Cystic basal cell carcinoma · Cicatricial basal cell carcinoma · Pigmented basal cell carcinoma · Aberrant basal cell carcinoma · Infiltrative basal cell carcinoma · Nevoid basal cell carcinoma syndrome · Polypoid basal cell carcinoma · Pore-like basal cell carcinoma · Fibroepithelioma of PinkusAcanthoma (Large cell acanthoma) · Adenoid squamous cell carcinoma · Basaloid squamous cell carcinoma · Clear cell squamous cell carcinoma · Signet-ring cell squamous cell carcinoma · Spindle cell squamous cell carcinoma · Bowen's disease
Marjolin's ulcer · Erythroplasia of QueyratOther/ungroupedMerkel cell carcinoma · Microcystic adnexal carcinoma · Mucinous carcinoma · Primary cutaneous adenoid cystic carcinoma · Verrucous carcinomaOtherAcanthoma: Acanthoma fissuratum · Clear cell acanthoma · Epidermolytic acanthoma · Melanoacanthoma · Pilar sheath acanthoma · Seboacanthoma
Keratoacanthoma: Generalized eruptive keratoacanthoma · Keratoacanthoma centrifugum marginatum · Multiple keratoacanthomas · Solitary keratoacanthoma
Adenocarcinoma: Aggressive digital papillary adenocarcinoma · Extramammary Paget's disease
Mixed tumor (Malignant mixed tumor)Ungrouped epidermal nevus: Epidermal nevus syndrome · Inflammatory linear verrucous epidermal nevus · Linear verrucous epidermal nevus · Pigmented hairy epidermal nevus syndrome · Systematized epidermal nevus · Schimmelpenning syndrome · Nevus comedonicus/Nevus comedonicus syndrome · Phakomatosis pigmentokeratotica
other nevus: Nevus unius lateris · Patch blue nevus · Unilateral palmoplantar verrucous nevus · Zosteriform speckled lentiginous nevus
ungrouped: balanitis (Balanitis plasmacellularis, Pseudoepitheliomatous keratotic and micaceous balanitis) · Cutaneous hornCategories:- Epidermal nevi, neoplasms, cysts
- Histopathology
- Carcinoma
Wikimedia Foundation. 2010.