- Skin neoplasm
-
Skin cancer Classification and external resources 
A basal cell carcinoma. Note the pearly appearance and telangiectasia.ICD-10 C43-C44 ICD-9 172, 173 ICD-O: 8010-8720 MedlinePlus 001442 eMedicine article/276624, article/870538, article/1100753, article/1965430 MeSH D012878 Skin neoplasms (also known as "skin cancer") are skin growths with differing causes and varying degrees of malignancy. The three most common malignant skin cancers are basal cell cancer, squamous cell cancer, and melanoma, each of which is named after the type of skin cell from which it arises. Skin cancer generally develops in the epidermis (the outermost layer of skin), so a tumor can usually be seen. This means that it is often possible to detect skin cancers at an early stage. Unlike many other cancers, including those originating in the lung, pancreas, and stomach, only a small minority of those affected will actually die of the disease,[1] though it can be disfiguring. Melanoma survival rates are poorer than for non-melanoma skin cancer, although when melanoma is diagnosed at an early stage, treatment is easier and more people survive.[2]
Skin cancer is the most commonly diagnosed type of cancer. Melanoma and non-melanoma skin cancers combined are more common than lung, breast, colorectal, and prostate cancer.[1] Melanoma is less common than both basal cell carcinoma and squamous cell carcinoma, but it is the most serious — for example, in the UK there were over 11,700 new cases of melanoma in 2008, and over 2,000 deaths.[3] It is the second most common cancer in young adults aged 15–34 in the UK.[4] Most cases are caused by over-exposure to UV rays from the sun or sunbeds.[5] Non-melanoma skin cancers are the most common skin cancers. The majority of these are basal cell carcinomas. These are usually localized growths caused by excessive cumulative exposure to the sun and do not tend to spread.
Contents
Classification
There are three main types of skin cancer: basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and malignant melanoma.
Cancer Description Illustration Basal cell carcinoma Note the pearly translucency to fleshy color, tiny blood vessels on the surface, and sometime ulceration which can be characteristics. The key term is translucency. Squamous cell carcinoma Commonly presents as a red, crusted, or scaly patch or bump. Often a very rapid growing tumor, pain is a common characteristic. Malignant melanoma The common appearance is an asymmetrical area, with an irregular border, color variation, and often greater than 6 mm diameter.[6] Basal cell carcinomas are present on sun-exposed areas of the skin, especially the face. They rarely metastasize and rarely cause death. They are easily treated with surgery or radiation. Squamous cell carcinomas (SCC) are common, but much less common than basal cell cancers. They metastasize more frequently than BCCs. Even then, the metastasis rate is quite low, with the exception of SCCs of the lip, ear, and in immunosuppressed patients. Melanomas are the least frequent of the 3 common skin cancers. They frequently metastasize, and could potentially cause death once they spread.[citation needed]
Less common skin cancers include: Dermatofibrosarcoma protuberans, Merkel cell carcinoma, Kaposi's sarcoma, keratoacanthoma, spindle cell tumors, sebaceous carcinomas, microcystic adnexal carcinoma, Pagets's disease of the breast, atypical fibroxanthoma, leimyosarcoma, and angiosarcoma.
The BCC and the SCC often carry a UV-signature mutation indicating that these cancers are caused by UV-B radiation via the direct DNA damage. However the malignant melanoma is predominantly caused by UV-A radiation via the indirect DNA damage.[citation needed] The indirect DNA damage is caused by free radicals and reactive oxygen species. Research indicates that the absorption of three sunscreen ingredients into the skin, combined with a 60-minute exposure to UV, leads to an increase of free radicals in the skin, if applied in too little quantities and too infrequently.[7] However, the researchers add that newer creams often do not contain these specific compounds, and that the combination of other ingredients tends to retain the compounds on the surface of the skin. They also add the frequent re-application reduces the risk of radical formation.
Signs and symptoms
There are a variety of different skin cancer symptoms. These include changes in the skin that do not heal, ulcering in the skin, discolored skin, and changes in existing moles, such as jagged edges to the mole and enlargement of the mole.
Basal cell carcinoma
Basal cell carcinoma usually presents as a raised, smooth, pearly bump on the sun-exposed skin of the head, neck or shoulders. Sometimes small blood vessels can be seen within the tumor. Crusting and bleeding in the center of the tumor frequently develops. It is often mistaken for a sore that does not heal. This form of skin cancer is the least deadly and with proper treatment can be completely eliminated, often without scarring.
Squamous cell carcinoma
Squamous cell carcinoma is commonly a red, scaling, thickened patch on sun-exposed skin. Some are firm hard nodules and dome shaped like keratoacanthomas. Ulceration and bleeding may occur. When SCC is not treated, it may develop into a large mass. Squamous cell is the second most common skin cancer. It is dangerous, but not nearly as dangerous as a melanoma.
Melanoma
Most melanomas are brown to black looking lesions. Unfortunately, a few melanomas are pink, red or fleshy in color; these are called amelanotic melanomas. These tend to be more aggressive. Warning signs of malignant melanoma include change in the size, shape, color or elevation of a mole. Other signs are the appearance of a new mole during adulthood or new pain, itching, ulceration or bleeding. An often-used mnemonic is "ABCD", where A= asymmetrical, B= "borders" (irregular= "Coast of Maine sign"), C= "color" (variegated) and D= "diameter" (larger than 6 mm—the size of a pencil eraser).
Other
Merkel cell carcinomas are most often rapidly growing, non-tender red, purple or skin colored bumps that are not painful or itchy. They may be mistaken for a cyst or other type of cancer.[8]
Causes
Ultraviolet radiation from sun exposure is the primary cause of skin cancer.[9][10] Other factors that play a role include:
- Smoking tobacco[10]
- HPV infections increase the risk of squamous cell carcinoma.[10]
- Some genetic syndromes[10] including congenital melanocytic nevi syndrome which is characterized by the presence of nevi (birthmarks or moles) of varying size which are either present at birth, or appear within 6 months of birth. Nevi larger than 20 mm (3/4") in size are at higher risk for becoming cancerous.
- Chronic non-healing wounds.[10] These are called Marjolin's ulcers based on their appearance, and can develop into squamous cell carcinoma.
- Ionizing radiation, environmental carcinogens, artificial UV radiation (e.g. tanning beds), aging, and light skin color.[10]
Pathophysiology
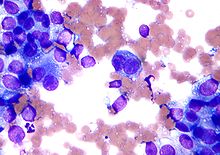
Squamous cell carcinoma is a malignant epithelial tumor which originates in epidermis, squamous mucosa or areas of squamous metaplasia.[citation needed]
Macroscopically, the tumor is often elevated, fungating, or may be ulcerated with irregular borders. Microscopically, tumor cells destroy the basement membrane and form sheets or compact masses which invade the subjacent connective tissue (dermis). In well differentiated carcinomas, tumor cells are pleomorphic/atypical, but resembling normal keratinocytes from prickle layer (large, polygonal, with abundant eosinophilic (pink) cytoplasm and central nucleus). Their disposal tends to be similar to that of normal epidermis: immature/basal cells at the periphery, becoming more mature to the centre of the tumor masses. Tumor cells transform into keratinized squamous cells and form round nodules with concentric, laminated layers, called "cell nests" or "epithelial/keratinous pearls". The surrounding stroma is reduced and contains inflammatory infiltrate (lymphocytes). Poorly differentiated squamous carcinomas contain more pleomorphic cells and no keratinization.[11]
Prevention
The risk of developing skin cancer can be reduced through a number of measures including:
- Decreasing indoor tanning and mid day sun exposure and increasing the use of sunscreen[12]
- Avoiding the use of tobacco products
- Reducing overexposure to ultraviolet (UV) radiation, especially in early years
- Wearing protective clothing (long sleeves and hats) when outdoors
- Broad-spectrum sunscreen that blocks both UVA and UVB radiation
- Reapplying sun block according to the manufacturer's directions
There is insufficient evidence to recommend for or against screening for skin cancer,[13]
While sunscreen has been shown to protect against BCC and SCC it may not protect against malignant melanoma. When sunscreen penetrates into the skin it generates reactive chemicals.[7] The experimental and epidemiological evidence suggests that sunscreen use is correlated with malignant melanoma incidence.[14][15][16][17][18][19] This gives rise to questions regarding the possibility that a sunscreen user's lifetime exposure to ultraviolet light may be higher than average. Alternatively, one might question whether sun screens are themselves tumor promoters or carcinogens. Arguably, sunscreen users are the ones most likely to be burned or have been burned by sun light. Similarly, most sunscreens primarily screen UVB, the primary cause of sunburn, while UVA is the primary cause of melanoma. Thus, by limiting the discomfort of sunburn, UVB screening may indirectly result in more UVA exposure. In any case, if some sunscreens promote skin cancer, physical light-scattering sunscreens based in zinc oxide, titanium dioxide or some other natural base are likely safer than chemical blockers such as benzones, etc., as they will be less chemically active.[20]Management
Treatment is dependent on type of cancer, location of the cancer, age of the patient, and whether the cancer is primary or a recurrence. Treatment is also determined by the specific type of cancer. A small basal cell cancer in a young person the treatment with the best cure rate (Mohs surgery or CCPDMA) might be indicated. In the case of an elderly frail man with multiple complicating medical problems, a difficult to excise basal cell cancer of the nose might warrant radiation therapy (slightly lower cure rate) or no treatment at all. Topical chemotherapy might be indicated for large superficial basal cell carcinoma for good cosmetic outcome, whereas it might be inadequate for invasive nodular basal cell carcinoma or invasive squamous cell carcinoma.[citation needed]. In general, melanoma is poorly responsive to radiation or chemotherapy.
For low-risk disease, radiation therapy (external beam radiotherapy or brachytherapy), topical chemotherapy (imiquimod or 5-fluorouracil) and cryotherapy (freezing the cancer off) can provide adequate control of the disease; both, however, may have lower overall cure rates than certain type of surgery. Other modalities of treatment such as photodynamic therapy, topical chemotherapy, electrodesiccation and curettage can be found in the discussions of basal cell carcinoma and squamous cell carcinoma.
Mohs' micrographic surgery (Mohs surgery) is a technique used to remove the cancer with the least amount of surrounding tissue and the edges are checked immediately to see if tumor is found. This provides the opportunity to remove the least amount of tissue and provide the best cosmetically favorable results. This is especially important for areas where excess skin is limited, such as the face. Cure rates are equivalent to wide excision. Special training is required to perform this technique. An alternative method is CCPDMA and can be performed by a pathologist not familiar with Mohs surgery.
In the case of disease that has spread (metastasized), further surgical procedures or chemotherapy may be required.[21]
Reconstruction
Currently, surgical excision is the most common form of treatment for skin cancers. The goal of reconstructive surgery is restoration of normal appearance and function. The choice of technique in reconstruction is dictated by the size and location of the defect. Excision and reconstruction of facial skin cancers is generally more challenging due to presence of highly visible and functional anatomic structures in the face.
When skin defects are small in size, most can be repaired with simple repair where skin edges are approximated and closed with sutures. This will result in a linear scar. If the repair is made along a natural skin fold or wrinkle line, the scar will be hardly visible. Larger defects may require repair with a skin graft, local skin flap, pedicled skin flap, or a microvascular free flap. Skin grafts and local skin flaps are by far more common than the other listed choices.
Skin grafting is patching of a defect with skin that is removed from another site in the body. The skin graft is sutured to the edges of the defect, and a bolster is placed atop the graft for seven to ten days, to immobilize the graft as it heals in place. There are two forms of skin grafting: split thickness and full thickness. In a split thickness skin graft, a shaver is used to shave a layer of skin from the abdomen or thigh. The donor site, regenerates skin and heals over a period of two weeks. In a full thickness skin graft, a segment of skin is totally removed and the donor site needs to be sutured closed.[22] Split thickness grafts can be used to repair larger defects, but the grafts are inferior in their cosmetic appearance. Full thickness skin grafts are more acceptable cosmetically. However, full thickness grafts can only be used for small or moderate sized defects.
Local skin flaps are a method of closing defects with tissue that closely matches the defect in color and quality. Skin from the periphery of the defect site is mobilized and repositioned to fill the deficit. Various forms of local flaps can be designed to minimize disruption to surrounding tissues and maximize cosmetic outcome of the reconstruction. Pedicled skin flaps are a method of transferring skin with an intact blood supply from a nearby region of the body. An example of such reconstruction is a pedicled forehead flap for repair of a large nasal skin defect. Once the flap develops a source of blood supply form its new bed, the vascular pedicle can be detached.[23]
Prognosis
The mortality rate of basal cell and squamous cell carcinoma are around 0.3% causing 2000 deaths per year in the US. In comparison the mortality rate of melanoma is 15-20% and it causes 6500 deaths per year.[24]:29,31 Even though it is much less common, malignant melanoma is responsible for 75% of all skin cancer-related deaths.[25]
Epidemiology
 Age-standardized death from melanoma and other skin cancers per 100,000 inhabitants in 2004.[26]
Age-standardized death from melanoma and other skin cancers per 100,000 inhabitants in 2004.[26] no dataless than 0.70.7-1.41.4-2.12.1-2.82.8-3.53.5-4.24.2-4.94.9-5.65.6-6.36.3-77-7.7more than 7.7
no dataless than 0.70.7-1.41.4-2.12.1-2.82.8-3.53.5-4.24.2-4.94.9-5.65.6-6.36.3-77-7.7more than 7.7A study of the incidence of non-melanoma skin cancer from 1992 to 2006 in the United States was performed by the dermatologist Howard Rogers, MD, PhD, and his colleagues based on the evaluation of Medicare databases. The results of their research showed that cases of non-melanoma skin cancer rose an average of 4.2% a year.[27]
More than 3.5 million cases of skin cancer are diagnosed annually in the United States, which makes it the most common form of cancer in that country. According to the Skin Cancer Foundation, one in five Americans will develop skin cancer at some point of their lives. The first most common form of skin cancer is basal cell carcinoma, followed by the squamous cell carcinoma. Although the incidence of many cancers in the United States is falling, the incidence of melanoma keeps growing, with approximately 68,729 melanomas diagnosed in 2004 according to reports of the National Cancer Institute.[28]
The survival rate for patients with melanoma depends upon when they start treatment. The cure rate is very high when melanoma is detected in early stages, when it can easily be removed surgically. The prognosis is less favorable if the melanoma has spread to other parts of the body.[29]
In the UK, 84,500 non-melanoma skin cancers were registered in 2007 although a study estimated that at least 100,000 cases are diagnosed each year. Most NMSCs were basal cell carcinomas or squamous cell carcinomas. In 2007, 10,672 cases of malignant melanoma were diagnosed.[30]
According to the British Association of Dermatologists children, from 0 to 14 years, and teenagers, from 15 to 19 years, exhibit the highest rates of skin cancers of any European country. Furthermore, incidence of melanoma increased four times in UK teenagers from 1978 to 1997.[31]
Australia exhibits one of the highest rates of skin cancer incidence in the world, almost four times the rates registered in the United States, the UK and Canada. Around 434,000 people receive treatment for non-melanoma skin cancers and 10,300 are treated for melanoma. Melanoma is the common type of cancer in people between 15–44 years in Australia.[32]
References
- ^ a b National Cancer Institute — Common Cancer Types (http://www.cancer.gov/cancertopics/commoncancers)
- ^ CancerStats — Skin cancer survival, Cancer Research UK
- ^ CancerStats — Skin Cancer statistics UK Cancer Research UK
- ^ Two young adults diagnosed with skin cancer each day, Cancer Research UK press release, 6th April 2011
- ^ Marks R (January 1995). "An overview of skin cancers. Incidence and causation". Cancer 75 (2 Suppl): 607–12. doi:10.1002/1097-0142(19950115)75:2+<607::AID-CNCR2820751402>3.0.CO;2-8. PMID 7804986. http://www3.interscience.wiley.com/journal/112688770/abstract?CRETRY=1&SRETRY=0.
- ^ "Malignant Melanoma: eMedicine Dermatology". http://emedicine.medscape.com/article/1100753-overview.
- ^ a b Hanson Kerry M.; Gratton Enrico; Bardeen Christopher J. (2006). "Sunscreen enhancement of UV-induced reactive oxygen species in the skin". Free Radical Biology and Medicine 41 (8): 1205–1212. doi:10.1016/j.freeradbiomed.2006.06.011. PMID 17015167.
- ^ Bickle, K; Glass, LF, Messina, JL, Fenske, NA, Siegrist, K (2004 Mar). "Merkel cell carcinoma: a clinical, histopathologic, and immunohistochemical review.". Seminars in cutaneous medicine and surgery 23 (1): 46–53. PMID 15095915.
- ^ Narayanan, DL; Saladi, RN, Fox, JL (2010 Sep). "Ultraviolet radiation and skin cancer.". International journal of dermatology 49 (9): 978–86. doi:10.1111/j.1365-4632.2010.04474.x. PMID 20883261.
- ^ a b c d e f Saladi, RN; Persaud, AN (2005 Jan). "The causes of skin cancer: a comprehensive review.". Drugs of today (Barcelona, Spain : 1998) 41 (1): 37–53. PMID 15753968.
- ^ ""Squamous cell carcinoma (epidermoid carcinoma) — skin" pathologyatlas.ro". http://www.pathologyatlas.ro/squamous-cell-carcinoma-skin.php. Retrieved 2007-07-21.
- ^ Lin, JS; Eder, M, Weinmann, S (2011-02-01). "Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force.". Annals of internal medicine 154 (3): 190–201. doi:10.1059/0003-4819-154-3-201102010-00009. PMID 21282699.
- ^ "Screening for Skin Cancer". U.S. Preventive Services Task Force. 2009. http://www.uspreventiveservicestaskforce.org/uspstf/uspsskca.htm.
- ^ Garland C, Garland F, Gorham E (1992). "Could sunscreens increase melanoma risk?". Am J Public Health 82 (4): 614–5. doi:10.2105/AJPH.82.4.614. PMC 1694089. PMID 1546792. http://www.ajph.org/cgi/reprint/82/4/614.
- ^ Westerdahl J; Ingvar C; Masback A; Olsson H (2000). "Sunscreen use and malignant melanoma.". International journal of cancer. Journal international du cancer 87 (1): 145–50. doi:10.1002/1097-0215(20000701)87:1<145::AID-IJC22>3.0.CO;2-3. PMID 10861466.
- ^ Autier P; Dore J F; Schifflers E; et al. (1995). "Melanoma and use of sunscreens: An EORTC case control study in Germany, Belgium and France". Int. J. Cancer 61 (6): 749–755. doi:10.1002/ijc.2910610602. PMID 7790106.
- ^ Weinstock, M. A. (1999). "Do sunscreens increase or decrease melanoma risk: An epidemiologic evaluation.". Journal of Investigative Dermatology Symposium Proceedings 4: 97–100. PMID 10537017.
- ^ Vainio, H., Bianchini, F. (2000). "Cancer-preventive effects of sunscreens are uncertain.". Scandinavian Journal of Work Environment and Health 26: 529–31.
- ^ Ainsleigh HG (1993). "Beneficial effects of sun exposure on cancer mortality.". Prev Med. 22 (1): 132–40. doi:10.1006/pmed.1993.1010. PMID 8475009.
- ^ Anti Aging Source Skin Cancer Facts (http://www.anti-aging-source.com/skin-cancer-facts.html)
- ^ Doherty, Gerard M.; Mulholland, Michael W. (2005). Greenfield's Surgery: Scientific Principles And Practice. Baltimore: Williams & Wilkins. ISBN 0-7817-5626-X.
- ^ Maurice M Khosh, MD, FACS. "Skin Grafts, Full-Thickness". eMedicine. http://emedicine.medscape.com/article/876379-overview.
- ^ Skin Cancer Reconstruction
- ^ C. C. Boring, T. S. Squires and T. Tong (1991). "Cancer statistics, 1991". SA Cancer Journal for Clinician 41 (1): 19–36. doi:10.3322/canjclin.41.1.19. PMID 1984806. http://caonline.amcancersoc.org/cgi/reprint/41/1/19.pdf.
- ^ "Early Detection and Treatment of Skin Cancer". American Family Physician 62 (2): 357–68, 375–6, 381–2. July 2000. ISBN 0962768804. PMID 10929700. http://www.aafp.org/afp/20000715/357.html. Retrieved 2008-04-21.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html. Retrieved Nov. 11, 2009.
- ^ "Epidemic of Skin Cancer in the U.S.?". http://www.webmd.com/melanoma-skin-cancer/news/20100316/epidemic-of-skin-cancer-in-the-united-states. Retrieved 2010-07-02.
- ^ "Skin Cancer Facts". http://www.skincancer.org/Skin-Cancer-Facts/. Retrieved 2010-07-02.
- ^ "Malignant Melanoma Cancer". http://www.skincancerjournal.com/melanoma/. Retrieved 2010-07-02.
- ^ "Skin Cancer – UK Incidence Statistics". http://info.cancerresearchuk.org/cancerstats/types/skin/incidence/index.htm. Retrieved 2010-07-02.
- ^ "UK Children Have Europe's Highest Skin Cancer Rates". http://www.medicalnewstoday.com/articles/106249.php. Retrieved 2010-07-02.
- ^ "Skin Cancer Facts and Figures". http://www.cancer.org.au/cancersmartlifestyle/SunSmart/Skincancerfactsandfigures.htm. Retrieved 2010-07-02.
External links
- skintumor.info Gallery
- American Cancer Society's Detailed Guide: Skin Cancer — Basal and Squamous Cell
- American Cancer Society's Detailed Guide: Skin Cancer — Melanoma
- skin neoplasm
- Medical Encyclopedia WebMD: Melanoma/Skin Cancer Health Center
- Medical Encyclopedia WebMD: Skin Cancer, Non Melanoma Guide
- Medical Encyclopedia MayoClinic: Skin cancer
- Skin Cancer Melanoma Warning Signs
- Interactive Health Tutorials Medline Plus: Skin cancer Using animated graphics and you can also listen to the tutorial
- Skin cancer at the Open Directory Project
- Skin cancer at the Yahoo! Directory
- Skin Cancer Foundation — Basal Cell Carcinoma
- Skin Cancer Foundation — Melanoma
- Skin Cancer Foundation — Squamous Cell Carcinoma
- Skin Cancer Foundation — Skin Cancer Facts
- Clinically reviewed non-melanoma skin cancer information for patients, from Cancer Research UK
Pathology: Tumor, Neoplasm, Cancer, and Oncology (C00–D48, 140–239) Conditions Malignant progressionTopographyHead/Neck (Oral, Nasopharyngeal) · Digestive system · Respiratory system · Bone · Skin · Blood · Urogenital · Nervous system · Endocrine systemHistologyOtherPrecancerous condition · Paraneoplastic syndromeStaging/grading Carcinogenesis Misc. M: NEO
tsoc, mrkr
tumr, epon, para
drug (L1i/1e/V03)
Tumors: Skin neoplasm, Nevi and melanomas (C43/D22, 172/216, ICD-O 8720-8799) Melanoma Mucosal melanoma · Superficial spreading melanoma · Nodular melanoma · lentigo (Lentigo maligna/Lentigo maligna melanoma, Acral lentiginous melanoma)Amelanotic melanoma · Desmoplastic melanoma · Melanoma with features of a Spitz nevus · Melanoma with small nevus-like cells · Polypoid melanoma · Soft-tissue melanomaNevus/
melanocytic nevusNevus of Ito/Nevus of Ota · Compound nevus · Spitz nevus (Pigmented spindle cell nevus) · Halo nevus · Pseudomelanoma
Blue nevus (Blue nevus of Jadassohn–Tièche, Cellular blue nevus, Epithelioid blue nevus, Deep penetrating nevus, Amelanotic blue nevus, Malignant blue nevus)
Congenital melanocytic nevus (Giant pigmented nevus, Medium-sized congenital nevocytic nevus, Small-sized congenital nevocytic nevus)
Balloon cell nevus · Dysplastic nevus/Dysplastic nevus syndrome
Tumors: Skin neoplasm, Epidermis (C44.L12–L38/D23.L53-83, 173/216) Tumor Micronodular basal cell carcinoma · Superficial basal cell carcinoma · Nodular basal cell carcinoma (Rodent ulcer) · Cystic basal cell carcinoma · Cicatricial basal cell carcinoma · Pigmented basal cell carcinoma · Aberrant basal cell carcinoma · Infiltrative basal cell carcinoma · Nevoid basal cell carcinoma syndrome · Polypoid basal cell carcinoma · Pore-like basal cell carcinoma · Fibroepithelioma of PinkusAcanthoma (Large cell acanthoma) · Adenoid squamous cell carcinoma · Basaloid squamous cell carcinoma · Clear cell squamous cell carcinoma · Signet-ring cell squamous cell carcinoma · Spindle cell squamous cell carcinoma · Bowen's disease
Marjolin's ulcer · Erythroplasia of QueyratOther/ungroupedMerkel cell carcinoma · Microcystic adnexal carcinoma · Mucinous carcinoma · Primary cutaneous adenoid cystic carcinoma · Verrucous carcinomaOtherAcanthoma: Acanthoma fissuratum · Clear cell acanthoma · Epidermolytic acanthoma · Melanoacanthoma · Pilar sheath acanthoma · Seboacanthoma
Keratoacanthoma: Generalized eruptive keratoacanthoma · Keratoacanthoma centrifugum marginatum · Multiple keratoacanthomas · Solitary keratoacanthoma
Adenocarcinoma: Aggressive digital papillary adenocarcinoma · Extramammary Paget's disease
Mixed tumor (Malignant mixed tumor)Ungrouped epidermal nevus: Epidermal nevus syndrome · Inflammatory linear verrucous epidermal nevus · Linear verrucous epidermal nevus · Pigmented hairy epidermal nevus syndrome · Systematized epidermal nevus · Schimmelpenning syndrome · Nevus comedonicus/Nevus comedonicus syndrome · Phakomatosis pigmentokeratotica
other nevus: Nevus unius lateris · Patch blue nevus · Unilateral palmoplantar verrucous nevus · Zosteriform speckled lentiginous nevus
ungrouped: balanitis (Balanitis plasmacellularis, Pseudoepitheliomatous keratotic and micaceous balanitis) · Cutaneous hornTumors: Skin neoplasm, dermis (C44/D23, 173/216) Dermis Subcutaneous
tumorsConnective and
vascularsee Template:Soft tissue tumors and sarcomas, Template:Vascular tumors, Template:Myeloid malignancy (for mastocytosis)Otherurogenital: Hirsuties papillaris genitalisneuro: Solitary neurofibroma · Cutaneous meningioma · Ganglioneuroma · Schwannoma · Palisaded encapsulated neuroma · Infantile neuroblastoma · Neuroma cutisnevus: Nevus anemicus · Nevus flammeus · Nevus flammeus nuchae · Nevus lipomatosus superficialis · Nevus oligemicus · Connective tissue nevus · Midline nevus flammeus · Porokeratotic eccrine ostial and dermal duct nevushistiocytoma: Malignant fibrous histiocytoma · Plexiform fibrohistiocytic tumor · Progressive nodular histiocytomaTeratoma · Adenoma sebaceum · Metastatic carcinoma · Giant cell tumor of the tendon sheath · Glomus tumor · Granular cell tumor · Carcinoid · Desmoid tumor · Neurothekeoma · Solitary angiokeratoma · Zosteriform metastasis · Keratinizing metaplasia · Epithelioid sarcomaTumors: Skin neoplasm, skin appendages / Adnexal and skin appendage (C44.L40–L68/D23.L15–49, 173/216) Glands Apocrine: Cylindroma (Dermal cylindroma) · Syringocystadenoma papilliferum · Papillary hidradenoma · Hidrocystoma · Apocrine gland carcinoma · Apocrine nevus · Spiradenomaapocrine or eccrine: Syringoma · Acrospiroma (Malignant acrospiroma) · Hidradenoma/Hidradenocarcinoma
ungrouped: CeruminomaNevus sebaceous · Muir–Torre syndrome · Sebaceous carcinoma · Sebaceous adenoma · Sebaceoma · Sebaceous nevus syndrome · Sebaceous hyperplasia · MantleomaHair Pilomatrixoma/Malignant pilomatricoma · Trichoepithelioma (Multiple familial trichoepithelioma, Solitary trichoepithelioma, Desmoplastic trichoepithelioma, Generalized trichoepithelioma) · Trichodiscoma · Trichoblastoma · Fibrofolliculoma · Trichilemmoma · Trichilemmal carcinoma · Giant solitary trichoepithelioma · Trichofolliculoma · Trichoadenoma
Hamartoma: Basaloid follicular hamartoma · Folliculosebaceous cystic hamartoma · Folliculosebaceous-apocrine hamartoma
Isthmicoma · Fibrofolliculoma · Perifollicular fibroma · Birt–Hogg–Dubé syndromeNails Categories:- Integumentary neoplasia
Wikimedia Foundation. 2010.