- Keratoacanthoma
-
Keratoacanthoma Classification and external resources 
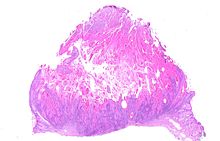
Keratoacanthoma.ICD-10 D23 (ILDS D23.L71) ICD-9 238.2 DiseasesDB 29383 eMedicine derm/206 MeSH D007636 Keratoacanthoma (KA) is a common low-grade (unlikely to metastasize or invade) skin tumour that is believed to originate from the neck of the hair follicle.[1] Many pathologists consider it to be a form of squamous cell carcinoma (SCC).[2] The pathologist often labels KA as "well-differentiated squamous cell carcinoma, keratoacanthoma variant", because about 6% of KA manifest itself as squamous cell carcinoma when left untreated.[3] KA is commonly found on sun-exposed skin, and often is seen on the face, forearms and hands.[4] The defining characteristic of KA is that it is dome-shaped, symmetrical, surrounded by a smooth wall of inflamed skin, and capped with keratin scales and debris. It always grows rapidly, reaching a large size within days or weeks, and if untreated will starve itself of nourishment, necrose (die), slough, and heal with scarring. While some pathologists classify KA as a distinct tumor and not a malignancy, enough clinical and histological KA do progress to invasive and aggressive squamous cell cancers, therefore prompt and aggressive treatment is required.[5][6] In reality, the defining characteristics of a KA can not be found when only a small fragment of a large KA is submitted for pathology review. If the keratin debris is submitted, no diagnosis can be made. If a deep core or peripheral deep wedge is performed, a squamous cell carcinoma is often noted. Only when almost the entire structure is submitted, can a true diagnosis of a KA be made. This further complicates the distinction between a clinical diagnosis of a KA and the pathologic diagnosis of a KA vs a squamous cell cancer.
Contents
Classification
Keratoacanthomas (molluscum sebaceum) may be divided into the following types:[7]:763-764[8]:643-646
-
- Giant keratoacanthoma
- Keratoacanthoma centrifugum marginatum
- Multiple keratoacanthomas (Ferguson Smith type of multiple self-healing keratoacanthomas, Multiple keratoacanthomas of the Ferguson-Smith type)
- Generalized eruptive keratoacanthoma (Generalized eruptive keratoacanthoma of Grzybowski)
- Subungual keratoacanthoma
Etiology
The tumors usually occur in older individuals (mean age 64 years old). Like squamous cell cancer, data suggests ultraviolet light from the sun causes the development of KA.[9] Just like its close relative, the squamous cell cancer, sporadic cases have been found co-infected with the human papilloma virus (HPV).[10]
Diagnosis
Diagnosis is best done with clinical exam and history. It presents as a fleshy, elevated and nodular lesion with an irregular crater shape and a characteristic central hyperkeratotic core. Usually the patient will notice a rapidly growing dome-shaped tumor on sun-exposed skin.
A skin biopsy must be performed to confirm the diagnosis. Unfortunately, a shave biopsy will often reveal only keratin fragments. A deep punch biopsy will often reveal a well differentiated, mildly atypical, squamous cell suggestive of an actinic keratosis or a squamous cell carcinoma. Only when the pathologist has access to the entire lesion (not practical in many circumstances) can a correct diagnosis be made. From a practical standpoint (insurance reimbursement), the correct diagnosis should be "well differentiated squamous cell carcinoma, keratoacanthoma variant". This is especially important for facial and nasal KA's, as it allows the surgeon to treat the tumor with the proper respect it deserves, with margin-controlled surgery like Mohs surgery. Correct diagnosis often requires communication between the surgeon and the pathologist. Many pathologists are still under the impression that keratoacanthomas are benign growths that do not require surgery. Unfortunately, when the lesion appears on the nose, face, or hands it often grows to marble or golf ball size before necrosing, and leaving a sizable crater in the process. From a practical standpoint, the correct diagnosis of low grade squamous cell carcinoma should be rendered after communication between the surgeon and pathologist, as the tumor is often much more aggressive and the morbidity is much higher than the relatively benign basal cell carcinoma.
Treatment
On the trunk, arms, and legs, electrodesiccation and curettage often suffice. Excision of the entire lesion is often required if one wants to confirm the clinical diagnosis of keratoacanthoma. On the nose and face, Mohs surgery allows for good margin control with minimal tissue removal; unfortunately, many insurance companies require the correct diagnosis of a malignancy before allowing such procedure. Recurrence after electrodesiccation and curettage is common, and usually can be identified and treated promptly with either further curettage or surgical excision. Allowing the KA to grow and necrose spontaneously is not acceptable in today's standard of care.
See also
References
- ^ Fisher, B.K., Elliot, G.B. Keratoacanthoma: Reflections on an Unusual Lesion. Can Med Assoc J. 1965 August 7; 93(6): 272–273.
- ^ Kossard S; Tan KB; Choy C; Keratoacanthoma and infundibulocystic squamous cell carcinoma. Am J Dermatopathol. 2008; 30(2):127-34 (ISSN: 1533-0311)
- ^ Weedon DD, et al. Squamous cell carcinoma arising in keratoacanthoma: a neglected phenomenon in the elderly. Am J Dermatopathol. 2010; 32(5):423-6
- ^ Schwartz RA. The Keratoacanthoma: A Review. J Surg Oncol 1979; 12:305-17.
- ^ Ko CJ, Keratoacanthoma: facts and controversies. Clin Dermatol. 2010; 28(3):254-61 (ISSN: 1879-1131)
- ^ http://www.emedicine.com/derm/topic206.htm
- ^ Freedberg, et. al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0071380760.
- ^ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0721629210.
- ^ Schwartz RA (February 2004). "Keratoacanthoma: a clinico-pathologic enigma". Dermatol Surg 30 (2 Pt 2): 326–33; discussion 333. doi:10.1111/j.1524-4725.2004.30080.x. PMID 14871228. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=1076-0512&date=2004&volume=30&issue=2%20Pt%202&spage=326.
- ^ Niebuhr M, et al. Giant keratoacanthoma in an immunocompetent patient with detection of HPV 11. Hautarzt. 2009; 60(3):229-32 (ISSN: 1432-1173)
Tumors: Skin neoplasm, Epidermis (C44.L12–L38/D23.L53-83, 173/216) Tumor Micronodular basal cell carcinoma · Superficial basal cell carcinoma · Nodular basal cell carcinoma (Rodent ulcer) · Cystic basal cell carcinoma · Cicatricial basal cell carcinoma · Pigmented basal cell carcinoma · Aberrant basal cell carcinoma · Infiltrative basal cell carcinoma · Nevoid basal cell carcinoma syndrome · Polypoid basal cell carcinoma · Pore-like basal cell carcinoma · Fibroepithelioma of PinkusAcanthoma (Large cell acanthoma) · Adenoid squamous cell carcinoma · Basaloid squamous cell carcinoma · Clear cell squamous cell carcinoma · Signet-ring cell squamous cell carcinoma · Spindle cell squamous cell carcinoma · Bowen's disease
Marjolin's ulcer · Erythroplasia of QueyratOther/ungroupedMerkel cell carcinoma · Microcystic adnexal carcinoma · Mucinous carcinoma · Primary cutaneous adenoid cystic carcinoma · Verrucous carcinomaOtherAcanthoma: Acanthoma fissuratum · Clear cell acanthoma · Epidermolytic acanthoma · Melanoacanthoma · Pilar sheath acanthoma · Seboacanthoma
Keratoacanthoma: Generalized eruptive keratoacanthoma · Keratoacanthoma centrifugum marginatum · Multiple keratoacanthomas · Solitary keratoacanthoma
Adenocarcinoma: Aggressive digital papillary adenocarcinoma · Extramammary Paget's disease
Mixed tumor (Malignant mixed tumor)Ungrouped epidermal nevus: Epidermal nevus syndrome · Inflammatory linear verrucous epidermal nevus · Linear verrucous epidermal nevus · Pigmented hairy epidermal nevus syndrome · Systematized epidermal nevus · Schimmelpenning syndrome · Nevus comedonicus/Nevus comedonicus syndrome · Phakomatosis pigmentokeratotica
other nevus: Nevus unius lateris · Patch blue nevus · Unilateral palmoplantar verrucous nevus · Zosteriform speckled lentiginous nevus
ungrouped: balanitis (Balanitis plasmacellularis, Pseudoepitheliomatous keratotic and micaceous balanitis) · Cutaneous hornCategories:- Epidermal nevi, neoplasms, cysts
-
Wikimedia Foundation. 2010.