- Endometrial cancer
Infobox_Disease
Name = Endometrial cancer
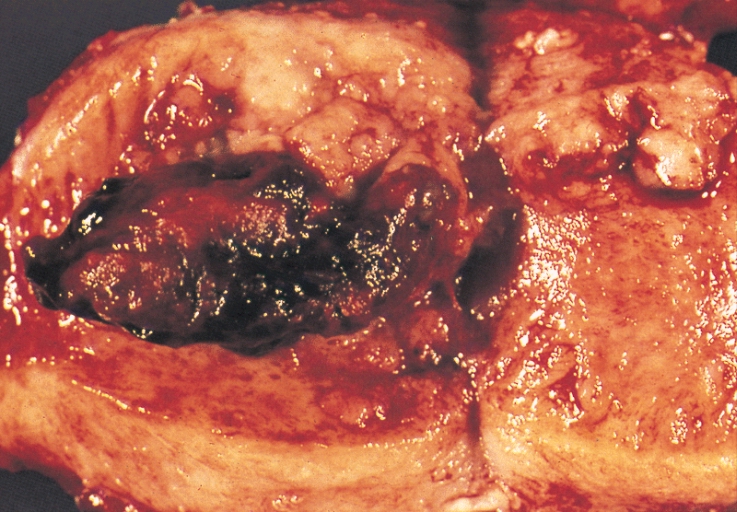
Caption = An "endometrial adenocarcinoma" invading the uterine muscle
DiseasesDB = 4252
ICD10 = ICD10|C|54|1|c|51
ICD9 = ICD9|182
ICDO =
OMIM = 608089
MedlinePlus = 000910
eMedicineSubj = med
eMedicineTopic = 674
eMedicine_mult = eMedicine2|radio|253
MeshID =Endometrial cancer refers to several types of malignancy which arise from the
endometrium , or lining of theuterus . Endometrial cancers are the most common gynecologic cancers in the United States, with over 35,000 women diagnosed each year in the U.S. The most common subtype, "endometrioid adenocarcinoma," typically occurs within a few decades ofmenopause , is associated with excessiveestrogen exposure, often develops in the setting ofendometrial hyperplasia , and presents most often withvaginal bleeding . Endometrial carcinoma is the third most common cause of gynecologic cancer death (behind ovarian andcervical cancer ). A total abdominalhysterectomy (surgical removal of the uterus) with bilateral salpingo-oophorectomy is the most common therapeutic approach.Endometrial cancer may sometimes be referred to as "
uterine cancer ". However, different cancers may develop not only from the endometrium itself but also from other tissues of the uterus, includingcervical cancer , sarcoma of themyometrium , andtrophoblastic disease .Classification
Most endometrial cancers are
carcinoma s (usuallyadenocarcinoma s), meaning that they originate from the single layer of epithelial cells which line the endometrium and form the endometrial glands. There are many microscopic subtypes of "endometrial carcinoma", including the common "endometrioid" type, in which the cancer cells grow in patterns reminiscent of normal endometrium, and the far more aggressive "papillary serous" and "clear cell" endometrial carcinomas. Some authorities have proposed that endometrial carcinomas be classified into two pathogenetic groups: [cite journal |author=Bokhman JV |title=Two pathogenetic types of endometrial carcinoma |journal=Gynecol. Oncol. |volume=15 |issue=1 |pages=10–7 |year=1983 |pmid=6822361 |doi=]*Type I: These cancers occur most commonly in pre- and peri-menopausal women, often with a history of unopposed
estrogen exposure and/orendometrial hyperplasia . They are often minimally invasive into the underlying uterine wall, are of the "low-grade endometrioid" type, and carry a good prognosis.*Type II: These cancers occur in older, post-menopausal women, are more common in
African-Americans , and are not associated with increased exposure to estrogen. They are typically of the "high-grade endometrioid", "papillary serous" or "clear cell" types, and carry a generally poor prognosisIn contrast to "endometrial carcinomas", the uncommon "endometrial stromal
sarcomas " are cancers which originate in the non-glandularconnective tissue of the endometrium. Uterinecarcinosarcoma ,"formerly called Malignant mixed müllerian tumor", is a rare uterine cancer which contains cancerous cells of both glandular andsarcoma tous appearance - in this case, the cell of origin is unknown.cite book |author=Richard Cote, Saul Suster, Lawrence Weiss, Noel Weidner (Editor) |title=Modern Surgical Pathology (2 Volume Set) |publisher=W B Saunders |location=London |year= |pages= |isbn=0-7216-7253-1 |oclc= |doi=]igns and symptoms
*Abnormal uterine bleeding, abnormal menstrual periods
*Bleeding between normal periods in premenopausal women
*Vaginal bleeding and/or spotting in postmenopausal women in women older than 40: extremely long, heavy, or frequent episodes of bleeding (may indicate premalignant changes)
*Anemia , caused by chronic loss of blood. (This may occur if the woman has ignored symptoms of prolonged or frequent abnormal menstrual bleeding.)
*Lower abdominal pain or pelvic cramping
*Thin white or clearvaginal discharge in postmenopausal women.Risk factors
*high levels of estrogen
*endometrial hyperplasia
*obesity
*hypertension
*polycystic ovary syndrome
*nulliparity (never having carried a pregnancy)
*infertility (inability to become pregnant)
*early menarche (onset of menstruation)
*late menopause (cessation of menstruation)
*endometrial polyps or other benign growths of the uterine lining
*diabetes
*Tamoxifen
*hyperplasia
*high intake of animal fat
*pelvic radiation therapy
*breast cancer
*ovarian cancer
*heavy daily alcohol consumption (possibly a risk factor) [3] ["Thirteen studies to date have reported on the relationship between endometrial cancer and alcohol consumption. Only two of these studies have reported that endometrial cancer incidence is associated with consumption of alcohol; all the others have reported either no definite association, or an inverse association." (Six studies showed an inverse association; that is, drinking was associated with a lower risk of endometrial cancer) "…if such an inverse association exists, it appears to be more pronounced in younger, or premenopausal, women." [3] "Our results suggest that only alcohol consumption equivalent to 2 or more drinks per day increases risk of endometrial cancer in postmenopausal women."]Diagnosis
Clinical evaluation
Routine screening of asymptomatic women is not indicated, since the disease is highly curable in its early stages. Results from a
pelvic examination are frequently normal, especially in the early stages of disease. Changes in the size, shape or consistency of the uterus and/or its surrounding, supporting structures may exist when the disease is more advanced.*A
Pap smear may be either normal or show abnormal cellular changes.
*Endometrialcurettage is the traditional diagnostic method. Both endometrial and endocervical material should be sampled.
*If endometrial curettage does not yield sufficient diagnostic material, adilation and curettage (D&C) is necessary for diagnosing the cancer.
*Endometrial biopsy or aspiration may assist the diagnosis.
*Transvaginalultrasound to evaluate the endometrial thickness in women with postmenopausal bleeding is increasingly being used to evaluate for endometrial cancer.
* Recently, a new method of testing has been introduced called the TruTest, offered throughGynecor . It uses the small flexibleTao Brush to brush the entire lining of the uterus. This method is less painful than apipelle biopsy and has a larger likelihood of procuring enough tissue for testing. Since it is simpler and less invasive, the TruTest can be performed as often, and at the same time as, a routine Pap smear, thus allowing for early detection and treatment.
* Ongoing research suggests that serum p53 antibody may hold value in identifying high-risk endometrial cancer. [ Am J Obstet Gynecol. 2007 Nov;197(5):505.e1-7 PMID: 17980190 ] Diagnostic test study of S-p53 Ab and agreement study for high-risk endometrial cancer Kappa: 0.70 Sensitivity (%): 64 Specificity(%): 96 PPV: 78 NPV: 92Pathology
The histopathology of endometrial cancers is highly diverse. The most common finding is a "well-differentiated endometrioid adenocarcinoma", which is composed of numerous, small, crowded glands with varying degrees of nuclear atypia, mitotic activity, and stratification. This often appears on a background of endometrial hyperplasia. Frank adenocarcinoma may be distinguished from atypical hyperplasia by the finding of clear stromal invasion, or "back-to-back" glands which represent nondestructive replacement of the endometrial stroma by the cancer. With progression of the disease, the myometrium is infiltrated.cite book |author=Richard Cote, Saul Suster, Lawrence Weiss, Noel Weidner (Editor) |title=Modern Surgical Pathology (2 Volume Set) |publisher=W B Saunders |location=London |year= |pages= |isbn=0-7216-7253-1 |oclc= |doi=]
Further evaluation
Patients with newly-diagnosed endometrial cancer do not routinely undergo imaging studies, such as
CT scan s to evaluate for extent of disease, since this is of low yield. Preoperative evaluation should include a complete medical history and physical examination, pelvic examination and rectal examination withstool guaiac test , chest X-ray, complete blood count, and blood chemistry tests, including liver function tests. Colonoscopy is recommended if the stool is guaiac positive or the woman has symptoms, due to the etiologic factors common to both endometrial cancer andcolon cancer . The tumor markerCA-125 is sometimes checked, since this can predict advanced stage disease. [Dotters DJ. Preoperative CA 125 in endometrial cancer: is it useful? Am J Obstet Gynecol 2000;182:1328-34. PMID 10871446.]taging
Endometrial carcinoma is surgically staged using the FIGO
cancer staging system.
*Stage IA: tumor is limited to the endometrium
*Stage IB: invasion of less than half themyometrium
*Stage IC: invasion of more than half the myometrium
*Stage IIA: endocervical glandular involvement only
*Stage IIB: cervical stromal invasion
*Stage IIIA: tumor invades serosa or adnexa, or malignant peritoneal cytology
*Stage IIIB: vaginal metastasis
*Stage IIIC: metastasis to pelvic or para-aortic lymph nodes
*Stage IVA: invasion of the bladder or bowel
*Stage IVB: distant metastasis, including intraabdominal or inguinal lymph nodesTreatment
The primary treatment is surgical. Surgical treatment should consist of, at least, cytologic sampling of the peritoneal fluid, abdominal exploration, palpation and biopsy of suspicious lymph nodes, abdominal
hysterectomy , and removal of both ovaries (bilateral salpingo-oophorectomy). Lymphadenectomy, or removal of pelvic and para-aortic lymph nodes, is sometimes performed for tumors that have high risk features, such as pathologic grade 3 serous or clear-cell tumors, invasion of more than 1/2 the myometrium, or extension to the cervix or adnexa. Sometimes, removal of theomentum is also performed.Abdominal hysterectomy is recommended over vaginal hysterectomy because it affords the opportunity to examine and obtain washings of the abdominal cavity to detect any further evidence of cancer.
Women with stage 1 disease who are at increased risk for recurrence and those with stage 2 disease are often offered surgery in combination with
radiation therapy [ Brachytherapy. 2008 Mar 19 PMID: 18358790 ] .Chemotherapy may be considered in some cases, especially for those with stage 3 and 4 disease. hormonal therapy with progestins and antiestrogens has been used for the treatment of endometrial stromal sarcomas. [ [http://www.cancer.org/docroot/CRI/content/CRI_2_4_4X_Hormone_Therapy_63.asp?sitearea] American Cancer Society - Uterine Sarcomas - Hormonal Therapy (accessed 5-25-07)]Complications of treatment
*A perforation (hole) of the uterus may occur during a D&C or an endometrial biopsy.
upport groups
The stress of illness can often be helped by joining a
support group where members share common experiences and problems.Prognosis
Because endometrial cancer is usually diagnosed in the early stages (70 % to 75 % of cases are in stage 1 at diagnosis; 10 % to 15 % of cases are in stage 2; 10 % to 15 % of cases are in stage 3 or 4), there is a better probable outcome associated with it than with other types of gynecological cancers such as cervical or
ovarian cancer . While endometrial cancers are 40% more common in Caucasian women, an African American woman who is diagnosed with uterine cancer is twice as likely to die, possibly due to the higher frequency of aggressive subtypes in that population.urvival rates
The 5-year survival rate for endometrial cancer following appropriate treatment is:
*75% to 95% for stage 1
*50% for stage 2
*30% for stage 3
*less than 5% for stage 4Epidemiology
Endometrial cancer occurs in both premenopausal (25%) and postmenopausal women (75%). The most commonly affected age group is between 50 and 59 years of age. Most tumors are caught early and thus prognosis is good and morbidity is declining.
References
External links
* [http://www.cancer.gov/cancertopics/types/endometrial U.S. National Cancer Institute: Endometrial cancer]
* [http://www.nlm.nih.gov/medlineplus/ency/article/000910.htm NIH Endometrial cancer fact page]
* [http://www.pathologyatlas.ro/Endometrial%20Carcinoma.html Anatomical pathology]
* [http://www.cancer.net/uterine/ Cancer.Net: Uterine (Endometrial) Cancer]
* [http://rad.usuhs.mil/medpix/medpix.html?mode=single&recnum=2490 MedPix endometrial cancer images]
Wikimedia Foundation. 2010.
